Culturally competent services
A culturally safe health system is as important as a
clinically safe health system. As evidence shows, when people experience
culturally unsafe health care encounters they will not use health services or
they will discontinue treatment, even when this maybe life threatening.[1]
4.1
The focus of this inquiry, the accessibility and quality of mental
health services in rural and remote Australia, is of particular importance to Aboriginal
and Torres Strait Islander peoples. As noted in Chapter 3, Aboriginal and
Torres Strait Islander peoples are much more likely to live in these areas than
non-Indigenous Australians.
4.2
The health outcomes for Aboriginal and Torres Strait Islander peoples is
far poorer compared to non-Indigenous people and addressing this health
disparity is the goal of many close-the-gap programs. Aboriginal and Torres
Strait Islander peoples are have disproportionately low outcomes on almost
every scale of social, health and wellbeing.[2] Of relevance to the health focus of this inquiry, the rate of admissions to specialised
psychiatric care for Aboriginal and Torres Strait Islander peoples is double
that of non-Indigenous Australians.[3]
4.3
The previous chapter outlined key barriers to the accessibility and
quality of mental health services in remote communities of Australia. These
included 'tyranny of distance' issues, workforce shortfalls and a lack of
appropriate support services, among others.
4.4
For Aboriginal and Torres Strait Islander peoples, there is the added
need for those services to be culturally competent in order to provide an
appropriate, and adequate, service that does not re-traumatise people through
the denial of their cultural needs. An overwhelming body of evidence presented
to this inquiry shows that the lack of culturally competent and safe mental
health services results in significantly lower rates of Aboriginal and Torres
Strait Islander peoples accessing the mental health services they need.[4]
4.5
This chapter will outline the frameworks of culturally competent mental
health service delivery in rural and remote locations, discusses the improved
health outcomes when services are culturally competent, and explores the
barriers to culturally competent service delivery. Although services which
target alcohol and other drugs (AOD) services are often co-located with mental
health services, this chapter will focus on clinical mental health services and
social and emotional wellbeing (SEWB) programs, as well as suicide prevention
strategies.
Service contexts
4.6
An overwhelming majority of submitters and witnesses cited the causes of
mental health problems for Aboriginal and Torres Strait Islander peoples as
being significantly different to non-Indigenous Australians, in that the causes
are primarily poor social determinants of health[5] which leave families and whole communities in crisis, combined with the trauma
caused by historical factors. A wide body of research has found that these
historical factors include intergenerational trauma, racism, social exclusion, and
loss of land and culture.[6]
4.7
The Aboriginal Health and Medical Research Council of NSW (AHMRC)
submitted that the compounding impact of removal from families, racism and loss
of culture through past assimilation policies left communities with high levels
of disadvantage and ill health.[7]
4.8
A General Practitioner from Kununurra discussed the range of causative
factors leading to mental health problems that she encounters as being
intergenerational trauma, sexual abuse and 'a whole breakdown of cultural
values, cultural connections, that we see; it's all absolutely contributing to
that.'[8]
4.9
The National Aboriginal Community Controlled Health Organisation (NACCHO)
submitted that:
[I]t is not possible to consider best practice mental health
models of service for Indigenous people without considering culture, including
an understanding of the multi-faceted impact that intergenerational trauma has
on Indigenous people and its inextricable link to mental health, and social and
emotional wellbeing.[9]
4.10
Prior to discussing the cultural competence of mental health service
delivery, it is important to outline the context in which those services are
being delivered. The following sections outline key service delivery factors
within Aboriginal and Torres Strait Islander communities.
Dispossession and colonisation
4.11
Evidence to this inquiry from a range of organisations noted that the
colonisation of Australia involved the disruption and severing of many of the
connections that are at the heart of social and emotional wellbeing and good mental
health for Aboriginal people.
4.12
Witnesses noted that these impacts are still felt in Aboriginal and
Torres Strait Islander communities today. The Aboriginal Medical Services
Alliance Northern Territory (AMSANT) noted that the current delivery of mental
health, SEWB and AOD services, generally without local input and governance,
replicates some of the harmful aspects of colonisation and has significant
implications for accessibility of services.[10]
4.13
The Medical Director of Wurli-Wurlinjang Health Service made a similar
observation:
The wellbeing of the community is affected by dispossession,
by poverty, by all these other things, by lack of respect from the Australian
government ...which has disempowered and continues to do that on a fairly
spectacular basis.[11]
4.14
Miss Nawoola Newry, a local advocate, pointed out that the direct outcomes
of colonisation occurred in Kununurra in living memory, which meant the trauma
was still fresh within that community.[12]
Collective and intergenerational
trauma
4.15
The Aboriginal and Torres Strait Islander Healing Foundation (Healing
Foundation) submitted that intergenerational trauma, where the impacts of
trauma continue down through multiple generations, is complex in its impacts as
it is both collective and cumulative. It is collectively experienced across
communities, it is cumulative over a life-span and can be passed from one
generation to the next.[13]
4.16
The Healing Foundation further submitted that the impacts of collective
trauma can be devastating, as it can cause whole community breakdown and a loss
of connection to community. This emphasises the need to provide collective
healing responses, as individual treatment interventions alone cannot address
this collective factor. The failure thus far to tailor healing efforts at a
community level means families continue to live in vulnerability without the
strength of a community to assist them to heal.[14]
4.17
The Central Australian Rural Practitioners Association told the committee
that the collective trauma of the stolen generation continues to impact
decisions to access mental health services, as 'there is a very strong fear now
still alive for Aboriginal people that welfare will be involved in your family
and you might lose your children. That does have an effect.'[15]
4.18
The committee also heard of the build-up of collective grief, where
communities were dealing with multiple instances of crisis and loss. A
psychologist for the Ord Valley Aboriginal Health Service described this as:
...people being in a constant state of grief and loss. They
have relatives dying consistently. We are talking about people attending a
funeral every week. They are almost in a cycle of grief and loss continuously.[16]
4.19
AMSANT submitted that the combination of these historical and present
day experiences of trauma result in the disconnections in aspects of life that keep
people well and strong and underlie the complex mental health, SEWB and AOD issues
that impact Aboriginal and Torres Strait Islander communities.[17]
Social determinants of health
4.20
Many submitters and witness argued that the provision of mental health
services will not alone address the mental health gap between Aboriginal and
Torres Strait Islander peoples and non-Indigenous Australians, as many of the
causes of poor mental health and wellbeing for Aboriginal and Torres Strait
Islander peoples are the social determinants of health, such as housing access,
adequate food and educational and job opportunities.[18]
4.21
The Manager of the Social Emotional Wellbeing Unit for Yura Yungi
Medical Service told the committee that housing was a significant factor in
stress-related mental health issues:
There's an extensive waiting list on the housing commission,
up to four to eight years. What we find is that this builds frustration. I
honestly think it has sometimes led to suicide, because people are frustrated,
they can't get out of it and there are arguments and things like that within
families.[19]
4.22
Townsville Aboriginal and Islanders Health Services told the committee
that many instances of clients with depression or anxiety are found to have
external stressor causes:
When the doctor talks to them, or even the health worker, in
their yarning they usually find out that it's more of a social thing. It might
be overcrowded at home or dad's not working—he's unemployed—or Billy might be
running off all the time and not going to school.[20]
4.23
The Social and Emotional Wellbeing support worker from the Kununurra
Waringarri Aboriginal Corporation discussed the levels of crisis that
individuals deal with on a regular basis, which leads to feelings of being
overwhelmed, such as dealing with 'housing, Centrelink, the courts, juvenile
justice and all that kind of stuff. A lot of them find it quite daunting and
hard to deal with.'[21]
4.24
The AHMRC argued that mainstream mental health services are not capable
of addressing the social determinants of wellbeing.[22] Mrs Gillian Yearsley, the Executive Director of Clinical Governance and
Performance with the Northern Queensland Primary Health Network (PHN) affirmed
this view and told the committee that:
Current mental health service models are based upon models of
care which are culturally inappropriate and which do not target the underlying
systemic issues within those communities. This impacts upon the health and
wellbeing of all community members, such as housing, employment, education,
access to healthy food and the areas which link to the social determinants of
health.[23]
4.25
The AHMRC pointed to the need for 'equitable funding and resource
allocation towards the determinants of health and wellbeing such as safe and
affordable housing, access to affordable nutritious food, and vocational and
educational opportunities.'[24]
Impacts of trauma on child
development
4.26
The committee heard a range of evidence that showed the social and
historical determinants of health for Aboriginal and Torres Strait Islander
peoples often has a more sharply felt negative impact on children.
4.27
The Healing Foundation submitted that the impact of trauma on children
can effect emotional regulation, attachment, aggressive behaviour and
developmental competencies.[25] This can be compounded by other risk factors experienced by Aboriginal and
Torres Strait Islander children, such as family disruption, family violence,
economic disadvantage, poor living standards, disengagement from school and
overcrowded housing.[26]
4.28
The Healing Foundation further submitted that medical research has also
shown that trauma interferes with childhood neurobiological development, impacts
responses to stress and increases a child's later engagement in correctional,
social and mental health services.[27]
4.29
The Youth Program Manager for the Shire of Halls Creek outlined that
there is higher than average presentation of youth with neurodevelopmental
disorders in that region which is generally undiagnosed until after they have
engaged youth justice services and these children 'are more likely than their
peers to have other mental disorders, such as anxiety, depression and
antisocial behaviour.'[28] The youth worker went on to detail other findings from diagnostic tools used on
this youth cohort:
Young people in the Olabud Doogethu program consistently
present with low baseline scores when tested against the Rosenberg self-esteem
scale, the Oxford happiness questionnaire, the social identification scale,
which relates to belongingness, and the Kessler psychological distress scale.
This indicates that clients have very little to no resilience skills.[29]
4.30
The Senior Medical Officer for the Nganampa Health Council told the
committee that the experiences of poverty, malnutrition, chronic stress and
exposure to violence damage the vulnerable minds and brains for children and
that this could cause physical changes:
The stresses are an ongoing thing. The high cortisol levels
not only change how your body works and ages more quickly from a cardiovascular
point of view but also the way the brain develops.[30]
4.31
A psychologist for the Ord Valley Aboriginal Health Service bluntly told
the committee that 'we've got kids who probably have the same circulating
stress hormones as people living in a combat zone—and that's what they're going
back home to.'[31] He further informed the committee that many of these children, some as young as
10 years old, self-medicate with cannabis to deal with their stress.[32]
4.32
The Mental Health Coordinator of the Ngaanyatjarra Health Service, a
mental health nurse, told the committee of child behaviour cases he sees, with
a range of possible causes such as 'alcohol, drugs, genes, genetics and in
utero stuff' and further told the committee it was things he had 'never seen
before within a city setting, the behaviours. A lot of it could be learnt
behaviours as well, plus the beginning of mental health behaviours.'[33]
4.33
One of the traumas experienced by Aboriginal and Torres Strait Islander
children in higher rates than non-Indigenous children is sexual assault. The
committee was told this can be caused in part by one of the social determinants
of health, overcrowded housing, which leads to children to being more
vulnerable to sexual assault because the 'protective factors of family being
able to provide safety are compromised.'[34]
4.34
A psychologist working for the Ord Valley Aboriginal Health Service told
the committee of the high rates of sexual abuse encountered among their client
population, which can be children as young as five to eight years of age:
Also, regarding seeing clients who are survivors of child
sexual abuse, I've never seen so many as in the Kimberley. I might have three
sessions a day sometimes that are survivors of childhood sexual abuse. So I
know we definitely need the services and skilled clinicians to help people
recover from that devastating history.[35]
4.35
The psychologist further stated that generally the presentation he sees
is an older female adolescent who is dealing with past trauma, who goes on to
being a long-term therapy client.[36]
4.36
The Sexual Assault Counsellor for Anglicare WA told the committee of the
impacts that child sexual assault can have on development:
Child sexual abuse can have a very significant impact on a
person's mental health both as a child and later on when they become an adult.
Child sexual abuse is often a factor in people experiencing mental illness. It
is identified as a factor in suicide and often results in personality
disorders.[37]
4.37
The Sexual Assault Counsellor for Anglicare WA further discussed the lack
of cultural competency in services to address issues of disclosure, including
training for local Aboriginal Health Workers:
There is a strong taboo against, and shame for, victims
speaking about sexual abuse, and this is especially the case for Aboriginal
people. There is a need for culturally appropriate education and resources to
be rolled out by people who are adequately trained. It is my opinion that we
need staff from both Aboriginal and non-Aboriginal backgrounds engaged in this
work. Aboriginal workers may require training and mentoring to overcome the
taboo associated with talking about sexual abuse.[38]
4.38
AMSANT told the committee that the only child and adolescent mental
health services in the Northern Territory are in Darwin and Alice Springs and
said that children are only receiving psychiatric care at crisis point from
mainstream services that are not culturally safe for them.[39] Jesuit Social Services pointed out that this is compounded in the Northern
Territory, where clinical psychologists used to be provided in schools but that
service is no longer funded.[40]
Drug and alcohol issues
4.39
Aboriginal and Torres Strait Islander communities often have high rates
of drug and alcohol use, which compounds and increases the complexity of mental
health service delivery. The Ord Valley Aboriginal Health Service told the
committee that the use of cannabis was 'linked to psychosis' but that clients
reported they used cannabis as a coping strategy:
What we see also is people almost in a perpetual state of
grief and loss, continuously, with many of their relatives passing. So I
believe that, quite often, alcohol and drug use is self-medication for
underlying mental health disorders and psychological distress.[41]
4.40
A local advocate in Kununurra also raised the issue of self-medication,
often to deal with undiagnosed mental health issues:
Because so many [in the] community have these illnesses that
are undiagnosed they turn to alcohol and drugs to mask their issues. When
people are self-medicating on such a level in town it creates all these extra
issues out in community. There can be violent outbursts and everything, which
the family have to deal with, and then that can create further dysfunction in
the family, trying to deal with that as well.[42]
Kinship and family structures
4.41
The different notions of kinship held by Aboriginal and Torres Strait
Islander peoples, alongside the increased cultural obligations to family, was
raised as an important service delivery context that was often overlooked by
non-Indigenous service providers. The Provisional Psychologist for the Derby
Aboriginal Health Service outlined that carer duties can impact on a client's ability
to attend appointments:
An Aboriginal person might book an appointment with me for 10
o'clock, but they don't rock up because Nan has said to them, 'I need to go to
Woolies at 10 o'clock.' I'm not prioritised. And why aren't I prioritised? I'm
not prioritised because they don't have to live the rest of their life with me;
they're going to live it with Nan, and Nan won't forget that they didn't take
her to Woolies at 10 o'clock when she needed to go...funders have difficulty
getting their heads around it.[43]
4.42
The committee was also told that Aboriginal families tended to be
larger, and for Aboriginal women with many children they found it difficult to
attend appointments while caring for their children.[44]
4.43
The committee was also told that the different family structures found
within Aboriginal communities can result in older Aboriginal women running
informal safe houses for children with limited resources, often funded by a
pension and under great stress:
These safe houses, which they run and organise and where
they've given their heart and their soul to the preservation of their children,
are really where the duty of care, in my view, shines...These are receiving
places within their community, built on a strong cultural base and on strong
relationships, either personal or otherwise....That's where the rubber hits the
road in this context. You asked the question: what are the cultural solutions?
There is one.[45]
Committee view
4.44
It is clear that the mental health service contexts for rural and remote
Aboriginal and Torres Strait Islander communities are greatly different to
those for predominantly non-Indigenous communities. These differing contexts
include both the causes of mental illness, as well as barriers to the service
delivery itself.
4.45
The committee heard compelling evidence directly from rural and remote Aboriginal
and Torres Strait Islander people of the environments in which they live, work
and raise families and the impacts these environments have on social and
emotional wellbeing. Aboriginal and Torres Strait Islander communities are
often operating in crisis mode, dealing with the continuing impacts of past
traumas such as colonial dispossession and the stolen generation, compounded by
ongoing traumas caused by high suicide rates and extremely poor social determinants
of health.
4.46
The committee also heard from a range of experts that those social
determinants of health have a far greater impact on individual mental health
outcomes for Aboriginal and Torres Strait Islander peoples than that felt in
non-Indigenous communities.
4.47
It is clear to the committee that health and mental health services
which do not reflect these contexts are not only destined to fail, in the worst
cases these services traumatise and retraumatise the very people for whom they
are supposed to provide therapeutic treatment.
Culturally competent services
4.48
The Implementation Plan for the National Aboriginal and Torres Strait
Islander Health Plan 2013–2023 outlines the importance of health services
being culturally competent.[46] The Implementation Plan states an intention that 'mainstream health services
are supported to provide clinically competent, culturally safe, accessible,
accountable and responsive services to Aboriginal and Torres Strait Islander
peoples in a health system that is free of racism and inequality.'[47]
4.49
The Congress of Aboriginal and Torres Strait Islander Nurses and
Midwives (CATSINaM) submitted that for Aboriginal and Torres Strait Islander peoples,
cultural wellbeing is inextricably linked to health outcomes, and pointed to
the National Aboriginal Health strategy definition of health:
Health is not just the physical wellbeing of the individual,
but the social, emotional and cultural wellbeing of the whole community in
which each individual is able to achieve their full potential as a human being,
thereby bringing about the total wellbeing of their community.[48]
4.50
NACCHO also discussed the importance of culturally competent health services
and submitted that this competency directly impacts the health outcomes of Aboriginal
and Torres Strait Islander peoples accessing those services:
Aboriginal people identify culture as key to mental wellbeing
and evidence highlights that programs and services which provide culturally
safe early intervention and prevention are the most effective in reducing the
likelihood of poor mental health and suicide.'[49]
4.51
However, NACCHO submitted that access to culturally secure mental health
services, particularly in rural and remote locations, is inconsistent and in
many cases is non-existent.[50]
What is cultural competence?
4.52
Before evaluating the cultural competence of mental health service
provision, it is useful to outline what cultural competence is and the impact
that cultural competence can have on the clinical outcomes of mental health
services for Aboriginal and Torres Strait islander peoples.
4.53
The Centre for Cultural Competence provides a definition of cultural
competence in an operational context as 'the integration and transformation of
knowledge about individuals and groups of people into specific standards,
policies, practices, and attitudes used in appropriate cultural settings to
increase the quality of services, thereby producing better outcomes.'[51]
4.54
The Tangentyere Council provided a commonly used definition of cultural
safety as:
An environment that is spiritually, socially and emotionally
safe, as well as physically safe for people, where there is no assault,
challenge or denial of their identity, of who they are and what they need.[52]
4.55
The committee was told that culturally competent service provision is
fundamental to the mental health outcomes of Aboriginal and Torres Strait
peoples. NACCHO submitted that the lack of culturally competent services is a
major barrier to Aboriginal people seeking the mental health care they need,
and that in 2012–13 seven per cent of Aboriginal and Torres Strait Islander peoples
reported avoiding seeking health care because they had been treated unfairly by
medical staff.[53]
4.56
It was also acknowledged to the committee that cultural competence in
the Aboriginal and Torres Strait Islander service setting is not a one size
fits all solution. Each community will have different needs and a different
cultural context and traditions.[54]
Trauma informed and strengths based
care
4.57
The interrelated nature of trauma informed care and culturally competent
care was raised by submitters and witnesses across a number of contexts. It was
contended that without cultural competency, services for Aboriginal and Torres
Strait Islander communities could not be considered trauma informed, as they
often inflicted additional trauma on the very people using the service.
4.58
AMSANT submitted that the mainstream models of trauma informed care,
considered best practice in non-Indigenous settings, could not be considered
best practice for Aboriginal and Torres Strait Islander peoples. AMSANT argued
it can in fact be harmful, because of the differences between non-Indigenous
and Aboriginal and Torre Strait Islander communities' belief systems and
historical experiences of colonisation.[55] AMSANT pointed to Culturally Responsive Trauma Informed Care as an approach of
best practice, which requires the service approach to be contextually tailored
and localised to the nuances of each location.[56]
4.59
The Healing Foundation contended that many mental health staff lack
education about the nature and impact of trauma on the mental health of Aboriginal
and Torres Strait Islander peoples. The Healing Foundation submitted that
despite an increasing awareness of trauma informed care in mainstream health
services, there is a significant gap in the accessibility of genuinely
trauma-informed mental health services for Aboriginal and Torres Strait
Islander peoples.
4.60
The use of fly-in, fly-out (FIFO) services can be particularly
problematic if people are encouraged to talk about traumatic life events, and
then the service is unavailable for over a month leaving the community to
manage the distress of the individual, and in some case suicide attempts.[57]
4.61
The issue of FIFO services was raised by many other witnesses. The Kununurra
Waringarri Aboriginal Corporation told the committee that many people will not
engage with a FIFO service because the periodic nature of the service raises
trauma and then leaves it unresolved:
They're thinking: 'What's the point of going and speaking to someone
who's only to be [here] for a week? We're not going to see them again.'...If they're supporting a person
who's going to be permanently based here in town and they can put a face to a
name and know that that person is going to be here for good, I think it will
encourage them to come out and really speak about our story and talk about what
issues they might be facing.[58]
4.62
The Consultant Psychiatrist with the Kimberley Mental Health and Drug
Service described other health services which are standard for non-Indigenous
patients but can be traumatising to Aboriginal and Torres Strait Islander
peoples:
If there is a compelling health reason to keep someone in
hospital, then yes, of course we will do that. That's our duty of care and it's
our ethical, personal and professional obligation...However, a hospital is an
institution. It's a conventional western institution that's a traumatising
place...that will often make things worse.[59]
4.63
The Consultant Psychiatrist also described how the usual approach to
therapeutic questioning can also be traumatising for an Aboriginal and Torres
Strait Islander patient:
When I take a step back in the consulting room, rather than
me driving that and rather than me being a top-heavy, medical-down
practitioner, if I've asked a local person who can build a bridge between me
and the distressed person rather than me inadvertently retraumatising that
person by grilling them with interrogative questions, the person who's there
building the bridge, the Aboriginal person, makes it a safe interaction and
allows that person and their family to buy in to the strategies that will most
likely make a more meaningful and enduring difference.[60]
4.64
CATSINaM pointed to strengths-based approaches being linked to wellbeing
in Aboriginal and Torres Strait Islander health, as they assist in changing perspectives
of Aboriginal and Torres Strait Islander health and provide alternative ways to
approach social and emotional wellbeing.[61]
4.65
AMSANT pointed to a review conducted for the Closing the Gap
Clearinghouse, which found that programs that show positive results for Aboriginal
and Torres Strait Islander peoples' social and emotional wellbeing are those
that are strengths-based, in that they 'encourage self-determination and
community governance, reconnection and community life, and restoration and
community resilience.'[62]
Cultural competency in
non-Indigenous services
4.66
As outlined above, a key concern raised regarding the cultural
competency of non-Indigenous service providers is the prevalence of the FIFO
model used to service remote communities.
4.67
The Regional Youth Program Manager for the Shire of Halls Creek
discussed how this model is incompatible for Aboriginal and Torres Strait
Islander adolescent mental health, which favours a drop-in model. The FIFO
model means that '[r]apport building with clientele is difficult, and intensive
therapeutical intervention is almost impossible.'[63]
4.68
AMSANT said that FIFO services often do not have access to community
members who do not show up for an appointment–as discussed early in this
chapter this can often be for competing family duty issues. Services run by
local community members with relationships on the ground can have staff drive
around and find those people and then conduct a meeting in a safe environment.[64]
4.69
The Acting Chief Executive Officer (CEO) of Jungarni-Jutiya Indigenous
Corporation gave a similar example, where a non-Indigenous service refused to
find a young man in need of mental health intervention, requiring him to visit
the service or attend hospital:
They waited four weeks until he went off his head. The system
doesn't work for people here because there's no real prevention on the ground.
They're all in these flash offices with the air conditioning and everything
else, but they're not on the ground out there where people can see them just
having a yarn with people. Mental health doesn't have to be that bad. If you
just go and have a yarn with somebody, you could stop those people from being
what they are in some cases.[65]
4.70
The Healing Foundation further submitted that government-funded services
need to reframe their thinking to recognise that service delivery failures are
due to a failure to build trust and safety with clients, rather than viewing Aboriginal
and Torres Strait Islander clients as being 'hard to reach.'[66]
4.71
Mr Nathan Storey, the chair of the Kununurra Region Economic Aboriginal
Corporation, told the committee that a lack of cultural awareness was also felt
in children's counselling services, where children did not engage because the
services were delivered 'in a little sterile room.' Mr Storey outlined how a
culturally competent children's service should engage with Aboriginal and
Torres Strait Islander children:
Take them out bush to hunt a kangaroo. Everyone will cook the
kangaroo and sit around eating damper and even marshmallows, if you want. We
will all sit, dance and sing. We will go to sleep and when we wake up we will
go fishing. We will come back. Eventually you'll get those kids opening up.[67]
4.72
The Youth Program Manager of the Shire of Halls Creek described how
external service providers continue to win service contracts, despite a low
success rate:
Services like this are not successful, and have not been able
to mobilise community buy-in; however, they continue to be funded. CAMHS—Child
and Adolescent Mental Health Services—have closed open cases on multiple
occasions due to little or no engagement with the client. So they've had a
referral, but when they come to Halls Creek every two to three weeks, they
can't find the client or the client does not want to engage, making rapport
building extremely difficult.[68]
4.73
The Healing Foundation contended that successful non-Indigenous service
models not only acknowledge Aboriginal and Torres Strait Islander culture, but
value it as a fundamental cornerstone.[69] This issue was raised by many witnesses, who argue that a lack of service
co-design with local communities resulted in poor services which were not
utilised by the local community:
Little consultation occurs with our communities with regard
to identifying the level of need and service design. Decisions about operating
models are often focused on budget constraints rather than the number requiring
access to the service.[70]
4.74
The CEO of Aarnja Ltd, pointed out that too many service decisions
impacting Aboriginal and Torres Strait Islander peoples are made by
non-Indigenous people:
So when you look at, for example, some of our decision-making
in the Kimberley—no disrespect to the organisations or departments here—when we
sit in discussions on Aboriginal people, it's predominantly non-Aboriginal
managers who sit in that space. They're getting direction and some information
from their Aboriginal staff, but the Aboriginal staff aren't at that
decision-making table. That needs to be changed if we're going to get any traction
within the current system.[71]
4.75
Submitters and witnesses argued that not only are many mainstream
services in remote locations not culturally competent or responsive, they do
not appear to take action to address this issue. Many services do not provide
cultural awareness training.[72] Where it is provided, it is insufficient, ad-hoc and relies on online training
modules.[73]
4.76
The CEO of Aboriginal Interpreting WA told the committee that addressing
intergenerational and vicarious trauma will not happen 'if it's continually
attempted in high English without regard for traditional Aboriginal languages.'
The CEO informed the committee that English is not the first language for many
Aboriginal people in Western Australia and many are missing out on services
where no interpretation is offered.[74]
4.77
The Tangentyere Council pointed out that mental health services also
include phone counselling services, such as Lifeline and beyondblue, which 'are
frequently not appropriate for people where English is a second or third
language or where the people on the end of the phone do not understand the
cultural context of the people they are speaking to.'[75]
4.78
The Healing Foundation recommended that cultural competency should be
tested with agreed criteria and standards, and that local community input
should be required, with measurable outcomes relating to the client's
experience used as the primary indicator of success.[76]
4.79
The Royal Flying Doctor Service (RFDS) told the committee that their
model of ensuring they are culturally competent is based on building
relationships with community controlled organisations:
We visit and work in community controlled organisations only
at the invitation of them. Over many years, those dynamics have developed such
that, for many nurse-led outposts, we provide the medical backup over the phone
and the emergency retrieval as required at the invitation of the community
controlled organisation. That will continue as we expand our mental health
service.[77]
4.80
The RFDS went on to say that the working model went beyond being invited
to a community, but included:
...the establishment of the service in response to local need...I
can flag that, as part of that very long established dialogue with community
controlled organisations, we'd only work where we're invited to do so with Aboriginal
communities and in the manner in which those communities want us to operate.[78]
4.81
Cyrenian House cited a similar approach, where that organisation
provides a monthly written report to the community councils outlining its recent
activities and seeking feedback from communities.[79]
Aboriginal community controlled services
4.82
The committee heard evidence from a range of organisations that the Aboriginal
Community Controlled Health Service (ACCHS) model of comprehensive primary
health care delivers better outcomes for Aboriginal people.[80]
Without exception, where Aboriginal people and communities
lead, define, design, control and deliver services and programs to their
communities, they achieve improved outcomes.[81]
4.83
The AHMRC submitted that for the majority of Aboriginal people, their
local ACCHS is their first point of contact with the health system and is their
preferred provider of primary care services. The AHMRC argued that Aboriginal
communities consider their ACCHS as integral to the wellbeing of the community,
and provides a gathering place where families can safely attend to their
physical and mental health needs.[82]
4.84
NACCHO also pointed to ACCHSs as best placed to deliver mental health
services to Aboriginal communities, as the community-based model of care involves
a sense of empowerment for Aboriginal people with mental illness.[83] Dr Denise Riordan, the Chief Psychiatrist of the Northern Territory, noted that
ACCHSs are also particularly good at delivering SEWB services.[84]
4.85
In some cases, to improve the cultural competency of external mental
health specific diagnostic tools, ACCHSs have rewritten the standard mental
health screening tools to adapt to local culture. This included ensuring that
the diagnostics were undertaken by health workers of the same gender as the
client, as required under local cultural tradition.[85]
4.86
In direct comparison to the clinical-setting services provided by many
non-Indigenous providers, the Derby Aboriginal Health Service outlined the
informal engagement methods they used to build rapport and trust with people
needing mental health support:
We have a community engagement model where a number of our
workers—our youth worker, our perinatal worker and our Aboriginal mental health
worker—actually spend a lot of time out in the community. So it's a more
relaxed approach...Ash, our male Aboriginal health worker, may go footy training
out of work hours and he may lean on the fence and have a yarn with someone.
It's in a very relaxed environment where the client or the patient feels
comfortable, but there's a consultation going on here. So we're reaching out.[86]
4.87
The Derby Aboriginal Health Service outlined that many Aboriginal people
will not attend state mental health services because of the history of institutions
for Aboriginal people.[87] The Danila Dilba Health Service made a similar observation, and pointed out
that the co-location of mental health services in ACCHSs meant that people who
are comfortable with their health service are more likely to access mental
health services located within the same facility.[88]
4.88
The Tangentyere Family Violence Prevention Program described the informal
environment they created to make clients feel safe:
We are surrounded by Aboriginal artwork, and the atmosphere
is welcoming and physically and emotionally safe. We understand that conducting
outreach to people's homes assists them to feel more in control. Many
conversations regarding challenging topics happen in the car.[89]
4.89
Dr Peter Fitzpatrick from the Wurli-Wurlinjang Health Service pointed
out to the committee that federal funding which used to resource the ACCHS
sector is now being diverted to fund PHNs, who then tender out services:
NGOs are all putting in tenders for chunks of money that
previously went to ACCHOs to provide services to Indigenous people, and that's
a concern for us. We've seen that here in Katherine. We've seen NGOs applying
for funding and winning the tender because they have access to great
tender-writers because they're multinational companies.[90]
4.90
Dr Fitzpatrick went on to state that ACCHSs have developed over time to
be highly effective health service delivery organisations:
There are 130-odd across Australia. They're a highly evolved
structure. We're general practice accredited. We're ISO accredited. We get
ticked off by ORIC and every other—we're, really, very organised organisations.
We've got state bodies and national bodies. And we're all paid for by the
Australian taxpayer, so use it. Use the structure that you've created instead
of bypassing it.[91]
Improved outcomes when services are
competent
4.91
The AHMRC pointed to the low numbers of Aboriginal people accessing
non-Indigenous mental health services, resulting in crisis presentation at
Accident and Emergency, resulting in admission for treatment and subsequent
community follow-up after discharge, at a cost of $19 728 per person. The AHMRC
submitted that evidence shows that better allocation of resources to the ACCHS
sector would result in a redaction of hospital admissions and associated costs,
because ACCHSs have made significant impact on the burden of illness in
Aboriginal communities and provide good value for money.[92]
4.92
NACCHO agreed with this view, noting that the ACCHSs sector was able to
deliver lower cost community-based mental health services and that these
services were closer to where people live, which assists in keeping people healthy
in the community and prevents hospital admissions.[93]
4.93
The AHMRC further submitted that although ACCHSs are making referrals to
funded non-government organisations (NGOs) and mainstream mental health
services, Aboriginal people are not presenting for those appointments, usually
as a result of inflexible and culturally unsafe practices in the organisations.[94] NACCHO agreed with this view and submitted that mainstream services are unable
to provide holistic and culturally competent care to Aboriginal people,
particularly those living in rural, remote and very remote locations.[95]
4.94
The Townsville Aboriginal and Islanders Health Services put forward a
similar view and told the committee:
We do have clients that still go out to the hospital, but
they don't ever return out there because of the way that they feel they're
treated. There's not a lot of Indigenous staff to support them when they're out
there, which, I suppose, comes back to resourcing and having enough staff to
help people.[96]
4.95
The Healing Foundation submitted that 'the most successful service
models to address trauma, healing and indeed mental health balance best
practice western methodologies with Aboriginal and Torres Strait Islander
cultural and spiritual healing practices.'[97]
4.96
The Townsville Aboriginal and Islanders Health Services told the
committee of the successful services they delivered using this model, where
Queensland Health are co-located at their clinic. This enabled the services to
establish trust before making a mental health referral, as they 'sometimes go
through another channel instead of going straight to mental health.'[98]
4.97
The Executive Director of medical services at the Wurli-Wurlinjang
Health Service agreed with this view and told the committee that:
...the experts in Indigenous mental health are Indigenous
people. They're not psychiatrists, they're not mental health nurses, they're
not GPs, and we don't recognise that—we don't pay for it and we don't engage
with that group. Those other groups come in and value-add to it but they can't
actually resolve it.[99]
4.98
The CEO of Kimberley Aboriginal Medical Services (KAMS) provided the
committee with an overview of all the positive outcomes that can be achieved
when services are culturally competent, which go far beyond improved service
delivery for individuals:
It will build local Aboriginal community capacity and
resilience through workers [being] trained and people feeling much more
comfortable in dealing with their own community. It will improve access and
coordination of care by having one-stop shops, so people don't have to try and
navigate this complex system. It'll help increase cultural awareness and
cultural safety of mainstream programs, because these workers can work with the
mainstream services to make sure that their programs and services are
appropriate. And it'll reduce costs of service delivery at the acute end if we
can keep people healthy and out of the expensive hospital system.[100]
4.99
Submitters and witnesses strongly argued that a culturally competent
workforce is the foundation to delivering culturally competent services. These
workforce challenges are discussed in detail in the following chapter.
Committee view
4.100
It is an accepted fact within various national health strategies and
implementation plans that health services must be culturally competent in order
to be effective. Cultural competency is not an optional extra. It is not a
gold-standard. Cultural competency is a basic benchmark that health services
must reach in order to meet the needs of the communities they serve, be they
urban, remote, non-Indigenous or a predominantly Aboriginal and Torres Strait
Islander client base.
4.101
The committee has heard overwhelming evidence that in rural and remote
locations, mental health services lack the cultural competency and safety required
to meet the most fundamental principle of medicine: first, do no harm.
4.102
The committee has also heard that the experts in cultural competency,
the local communities, have very little input into service design or scope of
practice. Clearly, until communities have greater say in what services are
funded and how those services will operate, mental health services for Aboriginal
and Torres Strait Islander peoples in rural and remote locations will continue
to fail their patients.
Social and emotional wellbeing programs
4.103
The committee heard from many submitters and witnesses that SEWB
programs are fundamental to improving the overall mental health of Aboriginal
and Torres Strait Islander communities, both on an individual and a collective
level.
4.104
The Social Health Reference Group, responsible for developing the National
Strategic Framework for Aboriginal and Torres Strait Islander People's Mental
Health and Social and Emotional Wellbeing 2004–2009, concluded that:
The concept of mental health comes more from an illness or
clinical perspective and its focus is more on the individual and their level of
functioning in their environment.
The social and emotional wellbeing concept is broader than
this and recognises the importance of connection to land, culture,
spirituality, ancestry, family and community, and how these affect the
individual.[101]
4.105
AMSANT stressed the importance of SEWB programs in Aboriginal and Torres
Strait Islander cultures (see Figure 4.1) and submitted that 'First Nations
Peoples of Australia maintained health and mental health through beliefs,
practices and ways of life that supported their social and emotional wellbeing
across generations and thousands of years'.[102]
Figure 4.1—Social and Emotional Wellbeing from an Aboriginal
and Torres Strait Islanders' perspective

Source: AMSANT.[103]
4.106
The National Mental Health Commission's 2015 Review of Mental Health Programmes
and Services concluded that mainstream mental health services had largely
let down Aboriginal communities and recommended that integrated mental health
and SEWB teams should be established in all ACCHSs.[104] The AHMRC made a similar recommendation to this inquiry, that all ACCHSs are
funded to build and establish SEWB teams including Residential Rehabilitation
and Healing Services.[105]
4.107
AMSANT recommended that integrating SEWB, mental health and AOD programs
into primary health care services is the most cost-effective approach to the
delivery of metal health services in rural locations. AMSANT stressed that this
requires funding for multidisciplinary, culturally and trauma informed teams.[106]
4.108
AMSANT told the committee of a SEWB model developed by a working group
of the Northern Territory Aboriginal Health Forum, based on a combination of a
community based Aboriginal workforce and a mental health professional
workforce. AMSANT told the committee this model includes both a clinical and
community development prevention component and is particularly suited to remote
communities. It provides access to therapy in a culturally safe environment,
noting that the provision of cultural and social support is a crucial part of
mental health care.[107]
4.109
The Healing Foundation cited research which indicates that healing
programs are best delivered on country by people from the same cultural group
as participants.[108]
4.110
The Queensland Alliance for Mental Health discussed the importance of
early intervention SEWB programs in providing people with supports in the early
stages of mental illness, resulting in the diversion of those people from more
expensive hospitalisation or long term National Disability Insurance Scheme
funding. The organisation went on to say that in rural and remote areas, one of
the most effective interventions is community capacity building via informal
programs in local communities.[109]
4.111
The Chief Psychiatrist of the Northern Territory stressed to the
committee the need for a broad approach to mental health, and that while
clinical mental health services are important components in addressing mental
health related conditions, 'the promotion and maintenance of mental health in
the community is influenced by many complex social factors and really is the
responsibility of the whole of the government and the whole of the community.'[110]
Committee view
4.112
As outlined earlier in this chapter, the committee heard that the social
determinants of health in rural and remote Aboriginal and Torres Strait
Islander communities are not being adequately addressed and that these
communities are often operating in a continual cycle of crisis. The committee also
received evidence that the collective social and emotional health of the
community is vital to individual mental health outcomes for Aboriginal and
Torres Strait Islander peoples.
4.113
These service contexts, however, are not being taken into account in
funding decisions and social and emotional wellbeing programs are not being
delivered to the extent needed in remote communities. It is clear to the
committee that increased focus on this form of early intervention would have a significantly
beneficial therapeutic impact to entire Aboriginal and Torres Strait Islander
communities.
Suicide prevention
4.114
Suicide is a major cause of Aboriginal and Torres Strait Islander
peoples' premature mortality and is a contributor to the overall Aboriginal and
Torres Strait Islander peoples' health and life expectancy gap. In 2014 suicide
was the fifth leading cause of death among Aboriginal and Torres Strait
Islander peoples, with the rate double that of non-Indigenous people.[111] In the 15–34 years age bracket, suicide is the leading cause of death[112] and those aged 15–24 are over five times more likely to commit suicide than
their non-Indigenous peers.[113] The Healing Foundation submitted that gender should also be considered as a
factor, as males represent a significant majority of completed Aboriginal and
Torres Strait Islander suicides.[114]
4.115
NACCHO noted that while the prevalence of mental disorders is similar
throughout Australia, the rates of suicide and self-harm are higher in rural
and remote areas, and these rates get higher as areas become more remote.[115] Again, this is more relevant for Aboriginal and Torres Strait Islander peoples,
as the majority of suicides among Aboriginal and Torres Strait Islander peoples
occurred outside of capital cities.[116]
4.116
AMSANT discussed the findings of a review of suicide prevention
strategies for Aboriginal and Torres Strait Islander peoples, which found:
High Indigenous suicide rates arise from a complex web of
interacting personal, social, political and historical circumstances. While
some of the causes and risk factors associated with Indigenous suicide cases
can be the same as those seen among non-Indigenous Australians, the prevalence
and interrelationships of these factors differ due to different historical,
political and social contexts.[117]
4.117
AMSANT further noted that this review found that one of the quality
indicators of suicide prevention services is culturally safe services and that
such services were optimally provided by ACCHSs.[118]
4.118
The Ngaanyatjarra Pitjantjatjara Yankunytjatjara Women's Council agreed
with this view of the non-mental health causes of suicide and told the
committee of their internal suicide register, which shows that half of all
suicides and attempted suicides have a clear link with domestic and family
violence.[119]
4.119
The Chief Executive Officer of the Northern Territory PHN noted that
culturally appropriate suicide prevention strategies need to be developed for
each community:
A prevention strategy that works on one community may have
very little impact on another. Culturally appropriate services need to be
developed, and community consultation and engagement is essential to this.
Those approaches need to be community led.[120]
4.120
NACCHO submitted that efforts to reduce suicide in Aboriginal and Torres
Strait Islander communities must do more than address social and economic
disadvantage and health gaps, and must also promote healing and building the
resilience of individuals, families and the whole community.[121] The Kimberley Aboriginal Law and Cultural Centre (KALACC) concurred with this
view and quoted an expert in indigenous suicide, Professor
Michael Chandler:
[I]f suicide prevention is our serious goal, then the
evidence in hand recommends investing new moneys, not in the hiring of still
more counsellors, but in organized efforts to preserve Indigenous languages, to
promote the resurgence of ritual and cultural practices, and to facilitate communities
in recouping some measure of community control over their own lives.[122]
4.121
KALACC cited the Western Australia (WA) Parliamentary report into
Aboriginal youth suicide, which found the need to focus more on a holistic
approach than a simple clinical approach[123] and recommended restoring culture and a sense of identity as a key protective
factor against Aboriginal and Torres Strait Islander suicide.[124] The CEO of KAMS also recommended that this report 'had a suite of
recommendations that we need to start to act upon.'[125]
4.122
The AHMRC submitted that evidence shows that programs and services which
provide culturally safe early intervention and prevention have proved to be the
most effective in addressing suicide.[126]
4.123
The National Suicide Prevention Trial, outlined in Chapter 2, involves a
number of trial sites, one of which is the Kimberley region of Western Australia
and targets Aboriginal and Torres Strait Islander peoples. This trial is
discussed below.
Kimberley suicide prevention trial
4.124
A decade-long audit quantified the suicide rate in the Kimberley among Aboriginal
and Torres Strait Islander peoples as among the highest rates in the world.[127] The CEO of KAMS told the committee 'this means is that Aboriginal family
members in the Kimberley are losing loved ones at rates that are among the
highest in the world.'[128]
4.125
The trigger factors for suicide in the Kimberley region include alcohol
and other drug use, relationship difficulties, family conflict or a previous
suicide attempt, as well as other causal issues, including intergenerational
trauma, loss of culture and other social determinants, such as employment,
education, and housing.[129] KALACC argued that Aboriginal suicide in the Kimberley has very little to do
with clinical mental health.[130]
4.126
A Consultant Psychiatrist with the Kimberley Mental Health and Drug
Service concurred with this view and listed the causes of Aboriginal and Torres
Strait Islander peoples suicide as the 'upstream factors' which also cause
substance use, poverty, children in custody and incarceration, stating that
'suicide is almost never due to a mental illness. So it's is not due to
something that we can diagnose and treat within a conventional Western model,
within a Western framework of how our hospitals and our clinics are set up.' He
went on to recommend that increased funding for clinical services was not the
answer:
People who are at risk of or complete suicide have drowned at
the end of the stream. If you give us more resources to catch more people with
nets before they drown, then of course we will catch more people before they
drown. However, that doesn't address the upstream factors.[131]
4.127
The committee was told that the National Suicide Prevention Trial was
not culturally competent to factors in the Kimberley region. The CEO of KAMS told
the committee that the National Suicide Prevention Trial needed to be more
responsive to the local factors, and that the trial is 'looking at evidence
from Europe, which senses depression as the centre of why people take their
lives, and all of the evidence in Aboriginal suicides says that it's not
depression; it's often all of the other crap that you're dealing with every
day.'[132]
4.128
Both KALACC and Aarnja sit on the National Suicide Prevention Trial
Kimberley community reference group. Both organisations discussed their
frustration with the project, citing a lack of progress and a lack of community
involvement in designing solutions:
All we get, as the community reference panel—they said,
'We'll set the strategic plan and we'll bring it back to you.' What did we get?
Two meetings in 12 months. No action. At the last meeting they came back and
said, 'We'll just give the money out.' As community organisation we thought we
were going to be consulted and involved in the establishment of the trial. It's
just gone to a fixed interest group. I will be blunt about it, because that's
what it is.[133]
4.129
Aarnja was so frustrated with the lack of progress and cultural
competence of the National Suicide Prevention Trial, they designed their own
suicide program, which is a family empowerment project for extended, rather
than nuclear, families and based is on Bardi and Jawi cultural frameworks.[134]
Inuit suicide prevention program
4.130
The high rate of suicide among Aboriginal and Torres Strait Islander
peoples is also found in other Indigenous peoples throughout the world.[135] The Canadian Inuit peoples' experience of colonisation is relatively comparable
to that of Aboriginal and Torres Strait Islander peoples, both historically and
also in the continued impacts of that colonisation in the form of collective
and intergenerational trauma and the destruction of the protective factors of
culture and a sense of identity.[136]
4.131
The following case study is of a suicide prevention strategy developed
for the Inuit Nunangat (homeland) regions in Canada by Inuit Tapiriit Kanatami,
the national representational organisation of Inuit in Canada.
Case study: National
Inuit Suicide Prevention Strategy
The National Inuit Suicide
Prevention Strategy (NISPS) envisions suicide prevention as a shared national,
regional, and community-wide effort that engages individuals, families, and
communities. The NISPS is a tool for assisting community service providers,
policymakers, and governments in working together to reduce the rate of suicide
among Inuit to a rate that is equal to or below the rate for Canada as a whole.
The NISPS will promote the
dissemination of best practices in suicide prevention, provide tools for the
evaluation of approaches, contribute to ongoing Inuit-led research, provide
leadership and collaboration in the development of policy that supports suicide
prevention, and focus on the healthy development of children and youth as the
basis for a healthy society.
Risk
factors for suicide
The NISPS identifies the key
risk factors for Inuit suicide as:
Historical Trauma: from the social and cultural upheavals tied to Canada's colonization of Inuit
Nunangat, experienced by an entire group as a result of a cumulative and
psychological wounding over a lifespan and across generations.
Social
Inequity: Poverty and other indicators of
social inequity translate into stress and adversity for families, disparities
in health status and increased risk of suicide.
Intergenerational
trauma: Unresolved symptoms of trauma can make
it difficult for caregivers to provide a sense of safety and security to their
children.
Childhood adversity: is linked to negative outcomes that are associated with suicidal behaviour,
such as poor mental health, substance abuse, and poverty.
Mental Distress: there are greater rates of depression, personality disorder and substance
misuse in Inuit who died by suicide.
Acute Stress: Mental
health disorders or developmental adversity impair an individual's ability to
cope with or adapt to life stress or change.
Strategy
The NISPS promotes an evidence-based,
Inuit-specific approach to suicide prevention by identifying priority areas for
intervention that would be most impactful in preventing suicide.
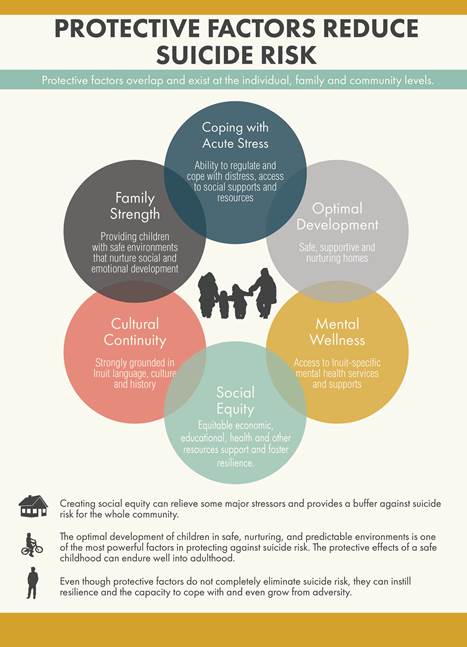
These priority areas are as
follows: (1) creating social equity, (2) creating cultural continuity, (3)
nurturing healthy Inuit children from birth, (4) ensuring access to a continuum
of mental wellness services for Inuit, (5) healing unresolved trauma and grief,
and (6) mobilizing Inuit knowledge for resilience and suicide prevention (see
Figure 4.2).
The Strategy's
evidence-based approach to suicide prevention considers the entire lifespan of
the individual, as well as what can be done to provide support for families and
individuals in the wake of adverse experiences that we know increase suicide
risk. Focusing our resources and efforts on supporting families and nurturing
healthy Inuit children is the most impactful way to ensure that people never
reach the point where they consider suicide.
Figure 4.2—Protective
factors identified by the Inuit suicide prevention strategy
Evaluation
One of the implementation
tasks will be to finalize an evaluation framework for the NISPS, by identifying
key indicators for each action item, and processes for collecting necessary
data in an ongoing way. Progress will be evaluated in two-year increments.
Source:
Inuit Tapiriit Kanatami, National Inuit Suicide Prevention Strategy,
2016.
Committee view
4.132
The committee heard evidence from organisations and communities that
suicide, both attempted and completed, has long since reached a crisis level in
rural and remote Aboriginal and Torres Strait Islander communities. That this
has been allowed to continue unchecked for so long is to Australia's shame.
4.133
The committee heard overwhelming evidence from mental health experts
that in too many cases, the causes of suicide for Aboriginal and Torres Strait
Islander peoples is not mental illness, but despair caused by the history of
dispossession combined with the social and economic conditions in which Aboriginal
and Torres Strait Islander peoples live.
4.134
The committee strongly recognises the Australian and international
evidence that demonstrates the most effective suicide prevention strategies for
Aboriginal and Torres Strait Islander peoples will be to restore strong,
resilient communities who are able to raise children with the inherent
protective factors that arise from safe homes, safe communities and strong
culture.
National strategic framework
4.135
The Australian Minister's Health Advisory Council endorsed the National
Strategic Framework for Aboriginal and Torres Strait Islander Peoples' Mental
Health and Social and Emotional Wellbeing 2017–2023 (Aboriginal Mental
Health Framework) in February 2017.[137]
4.136
The stated purpose of the Aboriginal Mental Health Framework is to 'to
guide and inform Aboriginal and Torres Strait Islander mental health and
wellbeing reforms' and to 'to respond to the high incidence of social and
emotional wellbeing problems and mental ill-health [of Aboriginal and Torres
Strait Islander peoples]'. The purpose also declares that ' the Australian
Government has committed to continue to seek advice from Aboriginal and Torres
Strait Islander mental health and related areas leaders and stakeholders to
shape reform at the national level.' [138]
4.137
The Aboriginal Mental Health Framework contains 5 key action areas, each
with three outcomes. Of particular relevance to discussions of culturally
competent mental health service delivery is the following action areas and
associated outcomes:
ACTION AREA 1: Strengthen the Foundations
Outcome 1.1: An effective and empowered mental health and
social and emotional wellbeing workforce.
Outcome 1.2: A strong evidence base, including a social and
emotional wellbeing and mental health research agenda, under Aboriginal and
Torres Strait Islander leadership.
Outcome 1.3: Effective partnerships between Primary Health
Networks and Aboriginal Community Controlled Health Services.
4.138
The Aboriginal Mental Health Framework notes that a monitoring plan
would need to be prepared, and noted it 'should be developed under the
leadership of, and in partnership with, Aboriginal and Torres Strait Islander
leadership bodies.'[139]
4.139
CATSINaM recommended that all planning and development of mental health
services should follow the recommendations made in the Aboriginal Mental Health
Framework and the National Aboriginal and Torres Strait Islander Health Plan
2013–2023, both of which 'were for and about Aboriginal and Torres Strait
Islander peoples and demonstrated best practice in policy development.'
CATSINaM noted however, that the Aboriginal Mental Health Framework did not yet
have an implementation plan and required associated funding investment.[140]
4.140
The following discussion outlines some continued policy and funding
concerns presented to the committee, which appear to show some inconsistency in
the early implementation of the Aboriginal Mental Health Framework.
Framework failures
4.141
A consistent theme appeared in the evidence presented to the committee,
that the lack of culturally competent mental health services for Aboriginal and
Torres Strait Islander communities was due in part to the fragmentation of
policy advice and funding arrangements across multiple jurisdictions. The
funding framework for mental health services was discussed in detail in chapter
two, including details on how the ACHHS sector is funded. This following
section will focus on certain policy and funding issues that continue to impact
the cultural competency of mental health services.
Policy fragmentation
4.142
The committee heard from a range of organisations that policy
fragmentation, across different geographical regions and different levels of
government, was a contributing factor to poor cultural competency of mental
health service delivery for rural and remote Aboriginal and Torres Strait
Islander peoples.
4.143
NACCHO submitted that policy fragmentation is also felt in how services
operate, citing that a lack of coordination between government and
non-government services impacts mental health service provision, particularly
in addressing needs in a 'culturally appropriate and holistic way.'[141]
4.144
The Danila Dilba Health Service made an overarching recommendation that
all levels of government, as well as non-government service providers, should
adopt a policy to move services to the Aboriginal community-controlled sector,
starting with capacity building of the sector. This could be done by funding
for services to Aboriginal communities including a requirement for non-Indigenous
providers to develop an exit strategy and show progress in implementing that
strategy. Danila Dilba Health Service cited the Jesuit Social Services in
Victoria, who partnered with the Victorian Aboriginal Child Care Agency (VACCA)
and managed a successful transition in the roles where VACCA is now the led
agency in the partnership.[142]
4.145
When asked about this program, Jesuit Social Services told the committee
that organisations must be prepared to allocate enough time within the program
framework 'to enable Aboriginal and Torres Strait Islander people to strengthen
their capacity so that in the long term they may develop the autonomy and
skills required to manage these services.' Jesuit Social Services discussed a
similar approach they took to service delivery in Santa Teresa, and noted that
'Business-wise, that work is difficult because, when you're continually
operating to put yourself out of business, you have to work out how you stay in
business too.'[143]
4.146
CATSINaM submitted that many areas of policy, such as economic and
environmental policy, use impact assessments to predict and assess the
consequences of a proposed policy, to assist in creating better outcomes. CATSINaM
recommended that future policy decisions for mental health should include a
social impact assessment to study the consequences on Aboriginal and Torres
Strait Islander peoples and all peoples in rural and remote Australia. CATSINaM
pointed to this being of particular importance for rural and remote Australia,
as the emphasis on market driven solutions for human services has resulted in
market failure in mental health services delivery in rural and remote
locations.[144]
Funding implications for cultural
competency
4.147
The committee was told that the complexity in funding arrangements for Aboriginal
and Torres Strait Islander-specific health and wellbeing services impacts on
the quality of those services.
4.148
NACCHO argued that the continual underfunding of ACCHSs to deliver
mental health and SEWB services limits the capacity of ACCHSs to improve the
mental health outcomes for Aboriginal people, leading to increases in hospital
admissions for complex and chronic conditions.[145]
4.149
Organisations from the ACCHS sector told the committee there was a
significant reduction in overall funding to the ACCHS sector after policy
oversight of Aboriginal-specific health and wellbeing funding was transferred
in 2013 from the Department of Health's Office of Aboriginal and Torres Strait
Islander Health to the Department of the Prime Minister and Cabinet.[146]
4.150
The committee was also told this transfer has resulted in increasing the
already confusing array of funding sources, which now includes the Department
of Prime Minister and Cabinet, Commonwealth health funding disbursed by PHNs,
as well as State and Territory funding. AMSANT recommended that at a
Commonwealth level, SEWB, mental health and AOD program funding be placed back
into the Indigenous Health Division of the Health Department, with input and
advice on funding decisions from jurisdictional forums such as the Northern Territory
Aboriginal Health Forum.[147]
4.151
The Northern Queensland PHN raised similar concerns, telling the
committee that multiple funding streams, not just in the health portfolio,
could be better coordinated to achieve improved outcomes with the same level of
resources.[148]
4.152
Danila Dilba Health Service commented that the fragmentation of funding
meant that an organisation could apply for capital works to build a facility,
but they did not guarantee funding would be supplied from different areas of
government to actually operate the service.[149] Danila Dilba Health Service also told the committee it takes a full time role
to apply for funding and then complete funding reporting requirements and they
had the capacity to do this only because they are a larger organisation.[150]
4.153
The Wurli-Wurlinjang Health Service noted that the funding fragmentation
of Aboriginal and Torres Strait Islander health and wellbeing programs
sometimes led to the duplication of services. It also noted that this
ever-changing funding environment also meant that organisations have 'no real
foundation in regard to infrastructure to work from. There's no stability;
you're constantly on the move because it's so funding dependent.'[151]
4.154
AMSANT submitted that the small amount of overall funding available for health
and wellbeing services to Aboriginal and Torres Strait Islander peoples often
goes to large NGOs who lack local and cultural expertise. This leads to mental
health services designed and delivered without local Aboriginal input, which
are usually ineffective and inappropriate for Aboriginal communities and
results in people not accessing these services.[152] AMSANT noted that the Northern Territory PHN had prioritised funding of ACCHSs,
but in other PHN areas this did not occur.[153]
4.155
The AHMRC raised a similar concern and submitted that current funding
landscapes, which include commissioning models and competitive tendering, have
resulted in a fragmentation of services where external NGOs are allocated
funding to work with Aboriginal communities, whose preference is to seek
services through their local ACCHS.[154]
4.156
The AHMRC pointed to recommendations from bodies such as the AMA and the
National Aboriginal and Torres Strait Islander Leadership in Mental Health,
which have recommended long term investment in the ACCHS sector by governments.[155]
4.157
The AHMRC submitted this could be implemented through a model where
ACCHSs work with Local Health Districts to develop integrated models of care. The
AHMRC argued that such partnership agreements would provide the framework to
develop better referral pathways, pre-discharge planning and care coordination.
This would also provide mainstream mental health workforces with the exposure
to Aboriginal culture needed to work in a culturally safe manner with
Aboriginal communities The AHMRC made further recommendations for reinvestment
in community mental health services to provide clinical services in thin
markets where specialist psychiatric services are scarce, such as child and
adolescent services. [156]
4.158
Neami National raised concerns that funding is not provided up-front for
service design, to ensure that organisations are 'working with people on the
ground in co-designing what that service might look like.'[157]
4.159
KALAAC pointed to the lack of funding overall for any form of cultural
programs, despite the findings on the important role of Aboriginal culture as a
protective factor against suicide. KALAAC cited Productivity Commission
statistics, that at present 0.74 per cent of Commonwealth and State Government
funding for Aboriginal Affairs in Western Australia are allocated to culturally
based programs.[158]
4.160
The Social and Emotional Wellbeing Manager for Aboriginal Interpreting
WA told the committee that investment in Aboriginal-designed programs was the
overarching solution:
There should be investment and building of the solutions for
our people. It's quite simple. We can have an overarching framework to sit with
our community and talk about our own intergenerational cycles, hold our own
people to accountability, create healing and be responsive and reflective of
our own people's needs. A right delayed is a right denied. The investment and
the solutions are before the government and before the decision-makers and the
influencers who have that power. So, there should be no inquiry and there
should be no royal commission; there should only be investment in the solutions
for a better way.[159]
Concluding committee view
4.161
The committee recognises that the mental health service needs of Aboriginal
and Torres Strait Islander peoples are different to those of non-Indigenous
Australians. This is because the causes of mental illness and disorders are
often very different, and the cultural framework for effective therapeutic
outcomes is also very different.
4.162
What was made clear in the evidence presented to the committee is that
those different health services needs are not being met, to devastating
outcomes for whole communities.
4.163
What was also made clear from experts in mental health and the
Aboriginal Community Controlled Health sector, is that the solutions are there,
but are not being recognised, funded and supported to grow. The committee is
strongly of the view that Aboriginal and Torres Strait Islander peoples mental
health service challenges in remote communities will only be solved when Aboriginal
and Torres Strait Islander peoples are given better opportunity to address
them.
Navigation: Previous Page | Contents | Next Page