CHAPTER 8
THE NATIONAL SUICIDE PREVENTION STRATEGY
Introduction
8.1
This chapter will address term of reference (h) the effectiveness of the
National Suicide Prevention Strategy (NSPS) in achieving its aims and
objectives, and any barriers to its progress.
National Suicide Prevention
Strategy
8.2
The current NSPS is a program under the COAG National Action Plan for
Mental Health 2006-11. The 2006-07 Federal Budget committed the Commonwealth
funding which included $62.4 million to expand the NSPP to $127.1 million
between 2006-07 and 2011-12.[1]
The five year goal of the NSPS is to reduce deaths by suicide across the
population and among at risk groups and to reduce suicidal behaviour by:
Adopting a whole of community approach to suicide prevention
to extend and enhance public understanding of suicide and its causes;
Enhancing resilience, resourcefulness and social
connectedness in people, families and communities to protect against the risk
factors for suicide; and
Increasing support available to people, families and
communities affected by suicide or suicidal behaviour.[2]
8.3
DoHA described the current NSPS as having four inter-related components.
The first is the LIFE Framework which 'provides national policy for action
based on the best available evidence to guide activities aimed at reducing the
rate at which people take their own lives'.[3]
The second was the National Suicide Prevention Strategy Action Framework which
provides a time limited workplan for taking forward suicide prevention and
investment. The Action Framework was developed in collaboration with ASPAC and '...will
effectively steer the NSPS and NSPP' until 2011. The third, the National Suicide
Prevention Program (NSPP), is the Commonwealth funding program for suicide
prevention activities which is administered by DoHA. The final component was mechanisms
to promote alignment with and enhance state and territory suicide prevention
activities, particularly to progress the relevant actions of related national
frameworks, such as the COAG National Action Plan for Mental Health 2006-2011 and the Fourth
National Mental Health Plan 2009-14.[4]
Suicide prevention in Australia
Department of Health and Ageing
8.4
DoHA has primary responsibility for suicide prevention at the
Commonwealth level but outlined the broad range of services and programs
(usually in the area of mental health) which assist those at risk of suicide. They
stated:
Mental health services and programs, broader health
initiatives such as indigenous health programs, and drug and alcohol support
also comprise an important platform from which DOHA administered programs
contribute to efforts to prevent suicide and support people at risk of suicidal
behaviour. Other Government portfolios similarly administer a broad range of
mainstream programs which contribute to supporting individuals at risk and
protecting against factors which may be associated with suicidality.[5]
8.5
In the area of mental health services DoHA highlighted a recent review
which indicated expenditure had increased to $1.9 billion in 2007-08. They
noted that while only 1 per cent of funding is 'directly contributed to the
NSPS, a large amount of funds are provided for programs and services which
support suicide prevention efforts'.[6]
These included mental health services under the MBS and programs such as ATAPS,
training for mental health professionals, mental health promotion (including the
National Depression Initiative), mental health programs funded for groups at
high risk of suicide (such as indigenous specific mental health programs),
early intervention programs (such as headspace) as well as programs for parents
(perinatal Depression Initiative) and children (KidsMatter Early Childhood).[7]
They also highlighted a range of supported telephone and web based crisis
support and self help therapies. The investment in the National Drug and
Alcohol Strategy was also highlighted as 'extremely relevant to suicide
prevention efforts'.
Broader investment in Indigenous health programs, including
social and emotional wellbeing activities also contributes to suicide
prevention efforts targeting Aboriginal people and Torres Strait Islanders.[8]
Department of Families, Housing,
Community Services and Indigenous Affairs (FaHCSIA)
8.6
The FaHCSIA submission also outlined a range of programs that, while not
specifically focused on suicide prevention, also contribute collaterally to the
prevention of suicide through promoting resilience and protective factors. They
stated:
FaHCSIA programs play a crucial role in providing early
intervention services for individuals and families from high risk vulnerable
groups. Many FaHCSIA programs aim to build individual and community resilience,
which is core to suicide prevention. Programs also provide services that can
ultimately reduce suicide risk and increase protective factors. Research suggests
that being part of a cohesive and supportive family unit is an important
protective factor for children and young people, helping them to better cope
with any stressors or adversity they may encounter.[9]
8.7
In particular FaHCSIA funds Mensline Australia delivered by Crisis
Support Services, an initiative which offers a range of services and programs
to support men in managing family and relationship difficulties.[10]
Department of Veteran's Affairs
(DVA)
8.8
DVA provides training for the peer support of veterans at risk of
suicide through Operation Life offering ASIST to veterans or support provided
through Family Relationship Centres to help families manage and resolve
conflict.[11]
8.9
As part of an election commitment the Commonwealth Government committed
to conducting a study that examines the broad issue of suicide in the
ex-service community, including a number of specific cases of suicide over the
last three years. The Suicide Study report conducted by Professor David Dunt,
together with the Government’s response, was publicly released on 4 May 2009.
The recommendations cover a wide range of matters, including strengthening
mental health programs, including suicide prevention, the use of experienced
case coordinators for complex cases, and ensuring that administrative processes
are more ‘user-friendly’.
8.10
The Government allocated $9.5 million over four years to implement the
recommendations in order to strengthen and improve the range of mental health
services provided, particularly in relation to suicide prevention, to support
the veteran community.[12]
8.11
DVA outlined a number of suicide prevention and mental health projects
directed to the veteran community. These included Operation Life, a
framework for action to prevent suicide and promote mental health and
resilience across the veteran community. A major part of this framework
included suicide prevention workshops as well as the provision of information
on treatment services that are available to the veteran community. Also
mentioned was the Veterans and Veterans Families Counselling Service (VVCS), a specialised
national service that provides counselling and support to Australian veteran, peacekeepers,
their families and eligible Australian Defence Force personnel.[13]
Other
8.12
Other areas noted included the role of the Department of Education,
Employment and Workplace Relations (DEEWR) which administers a range of
services to assist people with mental illness and those at risk of suicide. Another
example was that Centrelink social workers referred 3,463 persons 'as a result
of being at risk of suicide' and 30,650 more broadly with 'mental health
issues'.[14]
States and Territories
8.13
The State and Territory governments have a range of suicide prevention
strategies and programs.
8.14
The Queensland Government stated that it planned to finalise the
Queensland Government Suicide Prevention Action Plan in 2010 following the
previous strategies Reducing Suicide: the Queensland Government Suicide
Prevention Strategy 2003-2008 (QGSPS) and Queensland Government Youth
Suicide Prevention Strategy 1998-2003. It noted that over the past 12 years
the Queensland Government has allocated an annual budget of $2 million directly
to cross-government suicide prevention initiatives.[15]
8.15
The NSW Government stated that it is in the process of developing a new
NSW whole-of-government 5-year suicide prevention strategy which will follow on
from the 1999 NSW Suicide Prevention Strategy: we can make a difference.[16]
8.16
The WA Ministerial Council for Suicide Prevention is an advisory body to
the WA Minister for Mental Health. The Council has been given a mandate to
oversee the implementation of the WA State Suicide Prevention Strategy
2009-2013 which has been committed $15 million over four years.[17]
8.17
The SA Government noted that SA Health is developing a statewide suicide
strategy '...that will focus on social justice, coordination, collaboration,
partnerships and building on existing programs'.[18]
The strategy will be released in late 2010.[19]
The SA Government also outlined recent funding for several suicide prevention
and support programs including to Beyondblue, SQUARE, Mental Health First Aid
(delivered by Relationships Australia SA) and to Centacare Suicide Prevention
Program ASCEND.[20]
8.18
The Victorian Mental Health Reform Strategy 2000-2019 Because mental
health matters states a goal of the strategy is to:
Renew our suicide prevention plan, Next Steps: Victoria’s
suicide prevention action plan, using the new national framework to
strengthen our ability to identify and respond to risk factors and emerging
trends in suicide behaviour and suicide prevention.[21]
8.19
In October 2009, the Tasmanian Government released Building the
Foundations for Mental Health and Wellbeing, a Strategic Framework and Action
Plan for Implementing Promotion, Prevention and Early Intervention (PPEI)
Approaches in Tasmania (the Framework). A priority under the framework was
the development of a Suicide Prevention Strategy for Tasmania. This has been
commissioned and is due for completion in June 2010.[22]
8.20
The NT Government noted that the NT Strategic Framework for Suicide
Prevention commenced in 2003. A NT Suicide Prevention Action Plan 2009
-2011 was launched in March 2009. The Plan provides a whole of Government
response to guide directions in suicide prevention over the next three years.
New funding of $330 000 has been allocated by the Department of Health and
Families from January 2009 to June 2010 to progress a range of new initiatives
including '...increased training programs in suicide prevention and self injury
and the development of suicide and bereavement support resources'.[23]
8.21
The ACT Government indicated it had recently launched a new suicide
prevention strategy Managing the Risk of Suicide: A Suicide Prevention
Strategy for the ACT 2009-2014 which '...was strongly aligned to the LIFE
Framework'.[24]
Coordination and collaboration.
8.22
A criticism of the NSPS was that it had resulted in fragmented services
for those at risk of suicide. The Suicide is Preventable submission argued that
'roles, responsibilities and accountabilities are poorly defined...there is no
agency at a national or state/territory level with the mandate to address
suicide and suicide prevention'.[25]
8.23
The Suicide is Preventable submission listed how responsibility for
suicide was distributed:
- Mortality data collection – this is distributed across an array
of organisations.
- Morbidity data – the AIHW and the Injury Surveillance Unit at
Flinders University.
- Funding for program initiatives – a person or small group of
public servants within health departments in the Commonwealth Government and in
some State and Territory governments. These staff are generally located within
the Mental Health Branches. They generally provide small scale grants and the
few national initiatives receive little funding.
- Research – some health departments program occasional grants for
‘research’. Other funds are provided on a competitive basis from the usual
national funding sources. Annual funding would be less than $10m, on the
available evidence.
- Services – crisis lines, support services, prevention,
intervention and bereavement activities are carried out by a range of non-government
organisations (NGOs) – many are parties to or supporters of this Submission.
- Advocacy – SPA
- Self-help groups and other support groups – small networks of
community groups. [26]
8.24
Similarly, Lifeline Australia stated that despite the significant
achievements of the NSPS, the 'execution of the strategy has often been
fragmented and lacks a clear vision for how all levels of government, community
stakeholders and consumers can work together in a co-ordinated way to think
strategically, plan effectively and achieve good outcomes'. Lifeline Australia recommended
the vertical integration of the NSPS by engaging all levels of government in
strategic development and implementation. It also noted the limited processes
or structures for developing systematic, cross sector collaboration. They
stated:
While entities like Suicide Prevention Australia do provide
forums for sharing of ideas, programs and research, more substantial
collaborative structures and mechanisms are needed to work with governments,
stakeholders, communities and consumers around planning, developing and
implementing suicide prevention strategy.[27]
8.25
Professor John Mendoza also highlighted problems with service
coordination between the programs funded by Commonwealth and the States and
Territories. He stated:
We have ridiculous overlaps and duplications of service, and
then we have massive gaps. As one consumer that I work with regularly describes
it, it is a lucky dip out there if you can get any access to mental health
services. It is a really lucky dip if you get access to quality mental health
services, ones that actually are effective. In this area, in relation to people
experiencing suicide ideation and suicidal behaviour, it is even a greater
lucky dip to actually score the sort of service that is going to work.[28]
8.26
Professor Graham Martin highlighted that there was the risk suicide
prevention activities could be subsumed into the mental health agenda and
'...lost as an issue'. He also commented on Commonwealth-State service provision
coordination:
Several programs in Far North Queensland were funded by the
Commonwealth but nobody at the state level seemed to know much about them—what
they were doing or how they were working. So there was then duplication, or
attempts at duplication.[29]
8.27
DoHA noted that alignment between Commonwealth, State and Territory
suicide prevention activities, coordinating investment and activities, was
being progressed through the Fourth National Mental Health Plan.[30]
This includes action to:
Coordinate state, territory and Commonwealth suicide
prevention activities through a nationally agreed suicide prevention framework
to improve efforts to identify people at risk of suicide and improve the
effectiveness of services and support available to them.[31]
8.28
DoHA stated that '...effort has gone into jointly planning Australian
Government suicide prevention investment with states and territories,
particularly under the COAG National Action Plan for Mental Health 2006-11 and work has begun
towards a single national suicide prevention framework'.[32]
However they acknowledged that efforts to align '...suicide prevention activity across
the Commonwealth and with state and territory government investment in suicide prevention
will continue to be both a priority and a challenge'.[33]
Governance and accountability
8.29
The Suicide is Preventable submission argued that the NSPS was not
actually a 'national strategy'. They commented:
It is not a national strategy in the way that other national
strategies are formal agreements signed by all Australian governments and, in
some cases, by community or industry stakeholders. The current strategy, which
carries that name, is the strategy of the Commonwealth Department of Health and
Ageing.[34]
8.30
Similarly the Suicide Prevention Taskforce argued the LIFE Framework had
served as a proxy for the NSPS. They said:
The NSPS is not a national policy or strategy endorsed by all
governments through COAG. It has never been endorsed by the Australian Health
Ministers' Conference or other inter-government forum. Nor is it a
whole-of-Commonwealth Government policy or strategy as it does not have the
engagement in development or deployment of a whole-of-government strategy. It
is a strategy developed by and deployed by the Commonwealth Department of
Health and Ageing.[35]
8.31
The ACT Government noted there was confusion within the community
concerning the status of the NSPS, specifically around whether or not there is
a national strategy. They stated:
Within the community, some view the Living Is For Everyone: a
framework for prevention of suicide in Australia as ‘the strategy’. However,
the Commonwealth refers to this as a ‘supporting resource’... The lack of clarity
concerning the content of the National Suicide Prevention Strategy is a
significant barrier to its successful implementation[36]
8.32
The ACT Government recommended that the Commonwealth provide greater leadership
and guidance surrounding strategies for national suicide prevention by
developing a clear strategy document which sets out actions to be implemented,
an implementation strategy and mechanisms for consistent data collection.
8.33
Some considered the role of government departments was limiting suicide
prevention activities. SPA commented that ...previous instability of
executive-level staffing arrangements within departments responsible for the
oversight of the NSPS has also produced an environment that has not been
entirely favourable to the development of a cohesive Australian suicide and
suicide prevention research agenda.'[37]
Similarly the Suicide Prevention Taskforce argued that 'changes in personnel,
machinery of government and policy frameworks have impeded progress and
outcomes'. They stated:
Health Departments have limitations in being able to provide
the leadership for a whole-of-government issue like suicide prevention and
bring about the structural and broader societal changes necessary to tackle
complex issues like suicide and they are limited in their ability to implement
whole-of-community programs.[38]
8.34
SPA commented that historically there had been broad support for the
NSPS objectives. However they stated:
In 2008, criticism was expressed by some suicide prevention
sector stakeholders towards national suicide prevention policy settings.
Feedback from the consultations undertaken as part of the independent
evaluation of SPA clearly indicated a growing sense of frustration and malaise
with regards to policy formulation and progress in Australia, including what
was perceived by some members to be a disregard of the informed advice of
experts, the evidence and/or the views of the sector and a continuing
marginalisation of the issue of suicide prevention more generally...[39]
8.35
The Suicide Prevention Taskforce submission proposed a new national
governance and accountability structure with four key organisations to
implement a 'coordinated multi-strategy approach to suicide prevention'. One of
the rationales for this approach was that suicide was not only a health issues
and there were a number of sectors '... private, public and community - with a
stake in suicide and suicide prevention'. In summary these proposed structure
would be:
- A new coordinating body which would monitor the performance of
subsidiary entities in the new structure and approve strategic priorities for
suicide prevention
- A peak advocacy body to advocate on behalf of service providers
and those affected by suicide.
-
A suicide prevention council and resource centre which would
develop information and resources for service providers, develop research
strategy, and develop standards and accreditation.
-
A national foundation in suicide prevention which would raise
funding from a variety of sources and promote awareness.[40]
8.36
Similarly Lifeline Australia recommended the creation of a national
organisation for suicide prevention independent of any specific government
department.[41]
Professor John Mendoza commented:
...we have to invest in new structures, new infrastructure and
invest in what is truly a national strategy, not one that has got the name 'National
Strategy’ but a national strategy that engages not only the other eight
governments in Australia but the sector, the industries, the stakeholders who
really want to see transformation in this area.[42]
8.37
The MHCA also linked better data collection in relation to suicide and
attempted suicide with better governance and accountability.
Robust accountability and transparency means removing the
process whereby governments assess their own performances and measures, and
giving this role to organisations that can provide genuine oversight and
accountability of progress in reducing suicide in Australia.[43]
8.38
Professor Peter Bycroft argued that there were too many vested interests
in control of the decision making process, in key positions of policy advice
and in co-dependency relationships with DoHA. He recommended that the advisory
bodies '... who are instrumental in decisions relating to priorities for policy,
service provision and funding should be arms length from the Department and
should not be dominated by either the medical/clinical professions or academics/researchers
who are major beneficiaries of those funding decisions'.[44]
8.39
Professor Patrick McGorry recommended that an aspirational target should
be set for the reduction in the rate of suicide in Australia. He noted this
target may not be quick to achieve but it would '...really put pressure on us as
a society to significantly reduce the suicide toll as we have been successful
in doing in reducing the road toll over the last couple of decades'.[45]
This is an approach that has been taken overseas. For example, Choose Life: the
national strategy and action plan to prevent suicide in Scotland includes a
target to reduce suicide by 20 per cent over ten years.[46]
8.40
Professor Graham Martin's comparison of national suicide prevention
strategies noted that some overseas jurisdictions have decided on specific
targets for reductions in suicide. He notes that this 'may be a two-edged
sword, on one hand leading to criticism of the government for not achieving a
goal, but it also may very well help with public perceptions, and the public
ownership of, and commitment to, suicide prevention'.[47]
Evaluation of the NSPS
8.41
In 2005 the Commonwealth engaged Urbis Keys Young to conduct an
independent evaluation of the NSPS. The evaluation found NSPS was '...widely
supported and perceived as an appropriate and necessary strategy that addresses
an ongoing community need'. However it also found that 'stronger evidence
regarding the impact and outcomes of NSPS funded projects is required'.
8.42
DoHA noted that a full independent evaluation of the NSPS is planned for
the 2010-11 financial year '...that will provide guidance on the currency and efficacy
of the strategy that will inform the department’s advice to government on any
changes of direction or amendments to the strategy'. [48]
The AISRP argued that evaluating the NSPS was problematic because of the
inaccuracy of ABS data on suicides.[49]
Funding issues
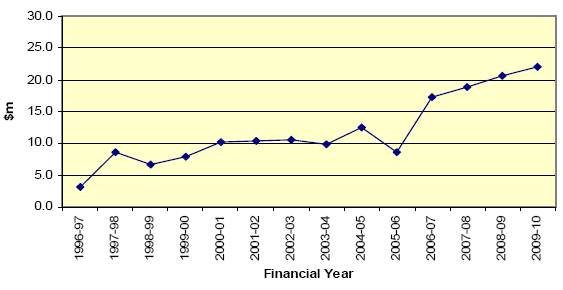
8.43
DoHA stated that the Commonwealth has increased its annual allocation of
funding for specific suicide prevention programs from $8.7 million in 2005-06
to $22.2 million in 2009-10 and that this forms part of a broader investment in
mental health services and programs of $1.9 billion.[50]
It stated '...investment by the Australian Government in suicide prevention has
increased significantly over the last decade, and that there has been no
reduction of effort despite the decline in official data on deaths by suicide'.[51]
Appropriations by Financial Year for National Youth
Suicide Prevention Strategy (1996-97
to 1998-99
and NSPP (1999-00
to 2009-10)[52]
8.44
However the lack of resources available to implement the NSPS was often
emphasised during the inquiry. For example Lifeline Australia stated that the 'financial
resources allocated to implementing the strategy are meagre in relation to the
scope of the problem...'.[53]
The funding available for suicide prevention was compared to other issues which
received greater levels of public funding such as road safety and cancer. RANZCP
recommended that funding allocated to suicide prevention should be equivalent
to that spent on events and/or illnesses with a similar mortality rate, for
example breast cancer.[54]
8.45
The Suicide is Preventable submission stated there was also a need to '...broaden
the funding base from non-government sources – that is, from community,
philanthropic, unions and other collectives and business sources – to
supplement the contributions made by governments'.[55]
8.46
The approach of the funding projects under the NSPS was also criticised.
The Suicide Prevention Taskforce stated that:
The NSPS approach to funding small scale projects has been
likened to 'spreading confetti across the land'. While this approach of
investing through small grants has developed some capacity in communities to
respond to suicide, few projects have been sustained and even fewer evaluated.[56]
8.47
SPA recommended the funding priorities should be shifted '... from
short-term small scale projects to longer-term investment in projects that
derive sustainable outcomes and include a budget for evaluation of
interventions as an evidence base against which to measure the ongoing
effectiveness of the NSPS'.[57]
8.48
A number of organisations commented that the lack of certainty regarding
funding cycles created problems for the organisations in maintaining staff as
well as the credibility with clients to whom assistance was being directed. The
ACT Government also noted there was a history of mental health programs
developed on a pilot basis, where Commonwealth funding is withdrawn after an
initial period despite positive evaluations. They noted this can have a
significant impact on clients who lose services and for providers who become
disillusioned or are unaware of services because of ongoing changes.[58]
8.49
This view was shared by many organisations which operated suicide
prevention programs. The Integrated Primary Mental Health Service of North East
Victoria emphasised:
We cannot stress enough the need for long term funding for
mental health skilled community workers. Grant funding is inappropriate. Short
term projects are regarded cynically, ‘How long are you lot going to be
around?’. We have learnt that workers need months to years to successfully
be accepted and valued by a community.[59]
8.50
Mr Keith Todd from OzHelp stated:
We lose good, quality people because they have family
themselves. They are probably looking for another job nine months out. They
have families to support and they have to take care of their own
sustainability.[60]
8.51
Similarly, Ms Kerry Graham from the Inspire Foundation commented:
... three-year funding contracts, which are set at the
beginning, do not allow a great deal of flexibility to be highly responsive;
and then, when you are getting to the end of your funding contract, you are putting
most of your efforts into repositioning or demonstrating success, which is very
important, as opposed to being as forward-thinking as you can be...[61]
8.52
Centre of Rural and Remote Mental Health Queensland stated:
Sustainability presents a significant challenge for community
based suicide prevention strategies. Pilot and seeding programmes that do not
have a strategy for longer-term implementation often raise expectations and
needs within communities that are then not met... With short term funding
arrangements, many groups struggle to find new resources. Efforts to
institutionalise programmes may compete with the time-consuming task of
fund-raising during the later stages of projects...There is also a strong
likelihood of a loss of momentum and the departure of key project staff.[62]
8.53
The Urbis Keys Young evaluation identified several aspects of the NSPS
structure and processes that could be strengthened. This included understanding
in the sector of '...funding processes and mechanisms to advise on the progress
and outcomes of NSPS activities and projects (including evaluations of these
projects)'.[63]
During the course of the inquiry the Committee heard from some community
organisations who felt their locally-based and long running programs had been
excluded from consideration for public funding as they did not have the
capacity to write complex competitive tenders.
8.54
DoHA told the Committee that following the open tender process for local
community grants in 2006 'there was some concern from smaller organisations who
were not as good at writing submissions as bigger organisations... worthwhile
small projects felt they could not compete'.[64]
Conclusion
8.55
The Committee understands that work is being undertaken to produce a
single national suicide prevention framework and DoHA has indicated that an
independent evaluation of the NSPS has been scheduled for financial year
2010-2011.
8.56
In the opinion of the Committee the policy documents around the NSPS
(the LIFE Framework resources and the National Suicide Prevention Action
Framework) do not assist understanding of suicide prevention activities in
Australia, particularly given the different strategies being conducted or
developed by the State and Territory governments. There is an opportunity to
simplify these policy documents and promote understanding of the NSPS and
suicide prevention activities in Australia.
Recommendation 37
8.57 The Committee recommends that following extensive consultation with
community stakeholders and service providers, the next National Suicide
Prevention Strategy include a formal signatory commitment as well as an appropriate
allocation of funding through the Council of Australian Governments.
8.58
The Committee is sympathetic to the views of many organisations and
individuals who supported the joint Suicide is Preventable submission and the
proposal that a new governance and accountability structure would assist the
delivery of suicide prevention programs in Australia. However the Committee is
also cautious to support the creation of several interrelated organisations
which may divert resources from suicide prevention activities and programs.
8.59
The Committee was interested in the recent changes to responsibility for
suicide prevention in WA. In that jurisdiction a Ministerial Council for
Suicide Prevention has been charged with overseeing the implementation of the
WA State Suicide Prevention Strategy which would be delivered by a
non-government organisation.[65]
The Committee considers that a greater role could possibly be taken by ASPAC
and the various State and Territory Ministerial Councils for suicide prevention
in developing policy and programs under the NSPS.
Recommendation 38
8.60 The Committee recommends that an independent evaluation of the National
Suicide Prevention Strategy should assess the benefits of a new governance and
accountability structure external to government.
8.61
The Committee accepts the recommendations made in many submissions that
funding for suicide prevention programs, projects and research in Australia be
substantially increased. The Committee recognises that many other public
programs and welfare expenditure operate to limit or decrease the incidence of
suicide and attempted suicide in Australia. In particular, a broad range of
mental health services and programs which function to prevent or treat mental
illness significantly contribute to reducing suicide and attempted suicide.
Similarly many other government services and programs can also be seen as promoting
recognised protective factors and limiting risk factors for suicide.
8.62
Nonetheless the funding for programs which could be described as at 'the
pointy end' of suicide prevention is relatively limited ($22.2 million in
2009-10) when considered against even some of the lower financial cost
estimates of suicide in Australia. Additional public funding directed to
effective programs and projects in this area can literally be considered to be
lifesaving. It is clear to the Committee that the public funding made available
for suicide prevention is not proportionate to the personal, social and
financial impacts of suicide in Australia.
8.63
The Committee also recognises the need to diversify the funding sources
for suicide prevention. In the view of the Committee there is merit in the Suicide
Prevention Taskforce proposal to establish a foundation to encourage other
sources of funding for strategic priorities in research, advocacy and service provision.
Recommendation 39
8.64 The Committee recommends that the Commonwealth government double, at a
minimum, the public funding of the National Suicide Prevention Strategy, with
further increases to be considered as the research and evaluation of suicide
prevention interventions develops.
Recommendation 40
8.65 The Committee recommends that the Commonwealth, State and Territory
governments should facilitate the establishment of a Suicide Prevention
Foundation to raise funding from government, business, community and
philanthropic sources and to direct these resources to priority areas of suicide
prevention awareness, research, advocacy and services.
8.66
The short term funding of programs and projects is an issue with which
the Committee is familiar from previous inquiries. Clearly this approach to
funding cycles allows government some flexibility to change priorities. However
short term funding cycles can be enormously detrimental to the establishment
and ongoing success of projects and programs. Short term funding cycles usually
create additional administrative burdens for projects, disruption for clients
and uncertainty for project employees.
Recommendation 41
8.67 The Committee recommends that, where appropriate, the National Suicide
Prevention Program provide funding to projects in longer cycles to assist the success
and stability of projects for clients and employees.
8.68
The most important measure of the effectiveness of the NSPS is whether
it has reduced the number of suicides in Australia over the period of its
operation. Unfortunately this measure has been obscured by changes to data
collection and uncertainty regarding the underreporting of suicides. The
situation will become clearer as revised data from the ABS is released over the
coming years and trends will be identified. The Committee feels that an
explicit and ambitious target for the reduction in the annual number of suicides
should be included in the NSPS. This target would function to focus the
attention and resources of government and the community on suicide prevention
initiatives.
Recommendation 42
8.69 The Committee recommends that the Commonwealth government as part of a
national strategy with State, Territory and local governments for suicide
prevention set an aspirational target for the reduction of suicide by the year
2020.
Navigation: Previous Page | Contents | Next Page