Chapter 2 - Health service delivery: Regional, rural and remote Australia
2.1
It was clear from the evidence received that the operation and
effectiveness of the travel schemes can only be understood within the broader
context of health service delivery in rural and remote Australia. A number of
supply and demand issues were presented to the Committee, which impact on the
efficacy of the current travel schemes and present future challenges for health
service delivery in rural and remote areas.
Regional, rural, remote: demography
2.2
There are three principal systems for defining non-metropolitan areas
(areas with less than 100,000 inhabitants) in Australia: the Australian
Standard Geographical Classification (ASGC), which defines an area's
'urbanness/ruralness'; the Accessibility/Remoteness Index of Australia (ARIA),
which defines an area's level of accessibility to goods and services; and the
Rural, Remote and Metropolitan Areas (RRMA) classification.[1]
2.3
The ASGC system was established by the Australian Bureau of Statistics.
Sections of the States and Territories are classified as follows:
- Major Urban: urban areas with a population of 100,000 and over
- Other Urban: urban areas with a population of 1000 to 99,999
- Bounded rural locality: rural areas with a population of 200 to
999
- Rural balance: the remainder of the states and territories
- Migratory: areas composed of offshore, shipping, and migratory
collection districts.[2]
2.4
The ARIA system was developed by the National Key Centre for Social
Applications of Geographical Information Systems (GISCA) at the University of Adelaide.
It has been summarised as follows:
Highly accessible: locations with relatively unrestricted
accessibility to a wide range of goods, services and opportunities for social
interaction.
Accessible: locations with some restrictions of some goods,
services and opportunities for social interaction.
Moderately accessible: locations with significantly restricted
accessibility of goods, services and opportunities for social interaction.
Remote: locations with very restricted accessibility of goods,
services and opportunities for social interaction.
Very remote: locations with very little accessibility of goods,
services and opportunities for social interaction.[3]
2.5
The following discussion draws extensively on publications by the
Australian Institute of Health and Welfare (AIHW), which uses the ASGC categories
of Major Cities, Inner Regional, Outer Regional, Remote and Very Remote. The
following map shows these classifications.
Figure 2.1: Australian Remoteness Areas
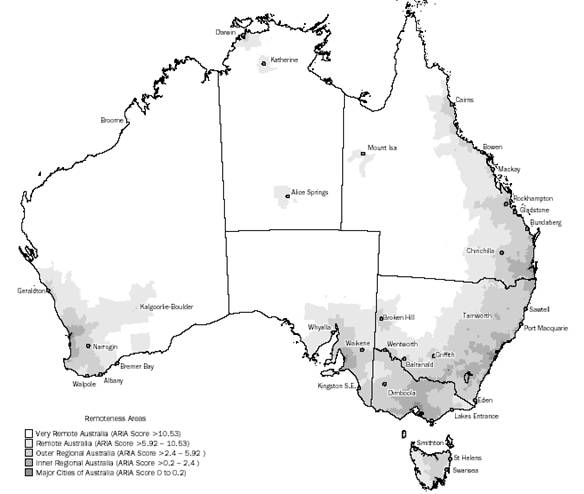
Source: http://www.abs.gov.au [accessed 31.8.07]
2.6
The regions outside Major Cities encompass an extremely diverse area
ranging from coastal or inland areas within commuting distance of Major Cities to
the sparsely populated, hot and dry
outback. Many areas outside Major Cities, predominantly on the coast, attract
older people in retirement. A significant proportion of the occupations in
regional and remote areas (for example mining, transport, forestry, commercial
fishing and farming) entail higher levels of risk than other occupations. One
in ten people in the non-metropolitan workforce is engaged in agriculture.
2.7
In Australia, two-thirds of the total population live in Major Cities,
with 21 per cent, 11 per cent, 2 per cent and 1 per cent living in Inner Regional,
Outer Regional, Remote and Very Remote areas respectively. The Indigenous
population of Major Cities is only 1 per cent (representing 30 per cent of the total
Indigenous population), increasing to 2 per cent and 5 per cent in Inner and
Outer Regional areas (43 per cent of the total Indigenous population), 12 per
cent in Remote areas and 45 per cent in Very Remote areas (27 per cent of
the total Indigenous population).[4]
2.8
Males outnumber females in almost all age groups in the more remote
areas. This is largely influenced by the non-Indigenous population. The number
of Indigenous males in each area is similar to the number of females.
2.9
Remote area populations tend to have proportionally more children and
working age males, and fewer elderly people than other areas. Regional areas
have proportionally lower numbers of people aged 25-44 years, higher numbers of
people aged 45-74 years and similar or slightly lower numbers of people older
than 75 years than other areas. In regional areas, children make up a higher proportion
than in Major Cities, but lower than in remote areas.[5]
Measures of health status in rural and remote areas
2.10
People in rural and remote areas generally do worse than other
Australians on a range of health status measures. There are higher mortality
rates, poorer dental health and higher levels of mental health concerns. This
is likely to be a result of a mix of behavioural, socioeconomic factors and
poorer access to health services.
2.11
The following is a brief overview of the findings of the AIHW's 2005 report
Rural, regional and remote health – Indicators of health which includes
measures of both health status and the determinants of health.[6]
2.12
The AIHW reported the following indicators of rural and remote health
status:
- Chronic disease: overall there was no significant difference
between the prevalence of self reported chronic diseases in regional areas and
Major Cities;
- Injury: people in regional areas were 1.2 times more likely to
self-report a recent injury and more likely to self-report a long-term
condition due to injury;
- Mental health: depression was more prevalent in regional areas;
- Dental health: children had more decayed, missing or filled teeth
in regional/remote areas;
- Communicable diseases: the rates of communicable disease
notification tend to increase with remoteness;
- Birthweight: very low birthweight babies were more prevalent compared
to Major Cities;
- Disability: disability was more prevalent compared to Major
Cities;
- Reduced activity because of illness: the average number of days
of reduced activity because of illness was greater in regional areas than in
Major Cities;
- Life expectancy: life expectancy was highest in Major Cities and
lowest in Very Remote areas likely due to the much lower Indigenous life
expectancy;
- Overall mortality: compared with their counterparts in Major
Cities males and females from regional and especially remote areas had higher
rates of death and death rates roses with increasing remoteness – this is about
3,300 additional deaths annually;
- Perinatal mortality: compared with their counterparts in Major
Cities rates of foetal and neonatal death were higher in regional and
especially remote areas which is at least partly a reflection of Indigenous
population distribution; and
- Causes of death: the leading causes of the higher death rates
experienced in regional and remote areas are mainly circulatory diseases (42
per cent of the excess deaths) and injury (24 per cent) with respiratory
disease and cancers contributing about 10 per cent of the 'excess' deaths
each.[7]
2.13
The AIHW also noted that rural and regional areas had poorer determinants
of health including less access to fluoridated water (only 30-40 per cent of
those in regional and Remote areas, and 25 per cent of those in Very Remote
areas have access to fluoridated water). Other determinants highlighted by the
AIHW included:
- higher unemployment rates in regional and remote areas compared
to Major Cities;
- lower after-tax household incomes in regional areas;
- the main sources of employment are agriculture, forestry, fishing
and mining with less employment in manufacturing;
- the three indexes of relative socioeconomic disadvantage (economic
resources, and education and occupation) outcomes were better in Major Cities
than in regional and remote areas;
- birth rates were higher for women in regional and remote areas
than for those in Major Cities, and increased with increasing remoteness;
- homicide death rates were substantially higher in Remote and Very
Remote areas (although the actual numbers of deaths were relatively small);
- there is more household crowding in Very Remote areas;
- food prices increased with remoteness – food prices in Very
Remote areas were between 14 per cent and 19 per cent higher than in the
Australian capital cities;
- fuel prices also increased with remoteness; and
- the cost of housing decreased with remoteness.
2.14
People in regional areas are more likely to smoke and more likely to
engage in risky alcohol consumption. Illicit drug use is more prevalent in
regional areas. The situation in remote areas is unclear. People in regional
areas are more likely to be sedentary and more likely to be overweight.[8]
2.15
The AIHW noted that people who live away from Major Cities and for whom
access to health services is restricted may be disadvantaged because of
different access to:
- preventive services such as immunisation and information allowing
healthy life choices;
- health management and monitoring;
- specialist surgery and medical care;
- emergency care, for example ambulance;
- rehabilitation services after medical or surgical intervention;
and
- aged care services.[9]
2.16
Evidence received by the Committee also emphasised the variation of
health outcomes in regional and remote Australia.[10]
2.17
The Australian Rural and Remote Workforce Agencies Group (ARRWAG) cited
the following statement from J. Dade-Smith in Australia's Rural and
Remote Health. A social justice perspective:
Australians living in rural areas have unique health concerns
that relate directly to their living conditions, social isolation,
socioeconomic disadvantage and distance from health services. They have death
rates that are double the urban rate due to injury, triple due to road
accidents and double due to falls in the aged. Hospital admission rates due to
diabetes are four times the urban admission rate. Yet rural people have lower
access to health care compared with their metropolitan counterparts because of
distance, time factors, costs and transport availability.[11]
2.18
Focusing specifically on breast cancer, a study commissioned by the
pharmaceutical company GlaxoSmithKline revealed that the higher mortality rate
of rural and remote women with breast cancer was due, in part, to 'later
diagnosis and less access to cancer screening and treatment services in
regional areas'.[12]
Other witnesses also noted that rural women are significantly more likely to
undergo mastectomy rather than breast-conserving therapy unlike urban women. It
was argued that rural women were less likely to travel to have breast-conserving
surgery at an urban treatment centre for adjuvant therapy.[13]
2.19
The Cancer Council Australia also pointed to poor outcomes for cancer
patients in rural and remote areas:
There is growing epidemiological evidence that cancer mortality
rates increase significantly in step with geographic isolation. A study
published in the Medical Journal of Australia in 2004 showed that people with
cancer in regional NSW were 35% more likely to die within five years of
diagnosis than patients in cities. Mortality rates increased with remoteness.
For some cancers, remote patients were up to 300% more likely to die within
five years of diagnosis.
A study published by COSA [Clinical Oncological Society of
Australia] in 2006 and editorialised in the Medical Journal of Australia mapped
the provision of rural/remote oncology services across Australia. The study was
the first national analysis to statistically demonstrate what has long been assumed:
that access to essential cancer care in all disciplines decreases nationwide as
communities became more isolated.[14]
2.20
There is also evidence on differences in the rate at which people from
major cities, regional and remote areas were admitted to hospital for a range
of surgical procedures in 2002–03. For example, rates of coronary artery bypass
graft and coronary angioplasty were lower among people from regional and
especially remote areas (and at odds with the pattern of death rates due to
coronary heart disease). Compared with residents of Major Cities, rates of:
- diagnostic gastrointestinal endoscopy and myringotomy were also
lower for residents of regional and especially remote areas;
- appendectomy and lens insertion were higher for residents of
regional and remote areas; and
- cholecystectomy, hip replacement, revision of hip replacement,
knee replacement, hysterectomy, tonsillectomy and arthroscopic procedures were typically
higher for residents of regional areas and lower for residents of remote areas.[15]
2.21
The Australian Medical Association (AMA) concluded that:
A driving factor behind these poorer health outcomes is the
difficulty people in regional and remote areas face in accessing specialist and
primary health care. Isolation and lack of services make it complicated for
these patients to receive preventive services and manage chronic diseases.
Consumers needing to travel long distances to access services can face considerable
disruption and personal financial cost.[16]
Access to services
2.22
Limited access to health services is a significant issue for people
living in rural and remote Australia. An inadequate supply of hospital and
other health services and workforce shortages in these areas were identified as
key factors.
Supply of hospital services
2.23
The provision of hospitals and hospital beds are concentrated in Major Cities
and regional areas. Some 22 per cent of public hospitals (but only 4.8 per cent
of the available beds) are located in remote and very remote areas (compared
with 6 per cent of the population).[17]
Most hospitals in remote areas are public hospitals. However, hospitals are
less likely to be accredited in regional and remote areas.
2.24
Most smaller rural hospitals are not equipped to provide the full range
of specialised services and people must be transferred to larger regional or
metropolitan centres. Some smaller hospitals operate as Multi-purpose Services
(MPSs) and provide a range of services such as emergency triage, hospital care
and aged and community care.
Workforce shortages
2.25
The supply of health workers in regional areas has long been an issue.
The AIHW reported that the supply of health workers declines with remoteness.
Table 2.1 shows the number of employed medical practitioners in 2003 by type of
practitioner and remoteness area.
Table 2.1: Employed medical
practitioners, by type of practitioner and remoteness areas
|
|
Major
Cities
|
Inner
Regional
|
Outer
Regional
|
Remote
|
Very
Remote
|
Total[a]
|
|
Type
of medical practitioner
|
|
|
|
|
|
|
|
Clinicians
|
39,389
|
7,074
|
2,948
|
468
|
212
|
51,819
|
|
Primary
care practitioners
|
15,132
|
3,901
|
1,740
|
301
|
152
|
21,919
|
|
Hospital
non-specialists
|
4,561
|
659
|
359
|
69
|
42
|
5,915
|
|
Specialists
|
14,580
|
2,164
|
665
|
79
|
15
|
18,093
|
|
Specialists-in-training
|
5,116
|
350
|
185
|
20
|
3
|
5,892
|
|
Non-clinicians
|
3,621
|
372
|
205
|
30
|
18
|
4,388
|
|
Total
|
43,010
|
7,446
|
3,154
|
498
|
230
|
56,207
|
|
No.
per 100,000 population
|
326
|
179
|
155
|
154
|
130
|
283
|
|
Percentage
female
|
32.6
|
27.4
|
30.3
|
31.5
|
35.0
|
31.9
|
|
Average
age (years)
|
45.7
|
46.8
|
45.1
|
44.7
|
43.4
|
45.9
|
|
Average hours worked per week
|
44.2
|
44.8
|
46.2
|
47.8
|
50.0
|
44.4
|
[a] Includes 1,870 medical practitioners who did not
provide information on the location of their main job.
Source:
Australian Institute of Health and
Welfare, Australia's Health 2006, p.325.
2.26
The AIHW noted that to some extent, the decrease in supply of medical
practitioners was countered by patterns of average hours worked by medical
practitioners which increased from 44.2 hours per week in Major Cities to 50.0
hours per week in Very Remote areas. The AIHW also noted that, consistent with
the placement of the large teaching hospitals near population centres, Major Cities
and Inner Regional areas together accounted for 84.3 per cent of specialists
and 92.8 per cent of specialists in training.
2.27
ARRWAG commented on access to primary health care providers,
particularly GPs and noted that in 1998 the Australian Medical Workforce
Advisory Committee (AMWAC) estimated the shortage to be in the region of 1240
GPs. Four years later, in 2002, the AMA commissioned a report from Access
Economics which estimated that there was a shortage of between 700 and 800 full
time equivalent GPs in rural and remote areas.[18]
2.28
The nursing workforce is more evenly distributed across regions than
medical practitioners, and shows a smaller variation in number per 100,000
population. Nurses in regional and remote Australia are older than in Major
Cities and tended to work longer hours per week in Remote and Very Remote
areas. Table 2.2 show employed registered and enrolled nurses in 2003.
Table 2.2: Employed registered and enrolled nurses, by
remoteness areas of main job, 2003
|
|
Major
Cities
|
Inner
Regional
|
Outer
Regional
|
Remote
|
Very
Remote
|
Total[a]
|
|
Number
|
147,670
|
48,440
|
22,719
|
3,870
|
1,936
|
236,645
|
|
No.
per 100, 000
|
1,120
|
1,167
|
1,115
|
1,193
|
1,095
|
1,191
|
|
Percentage
female
|
91.2
|
90.9
|
93.9
|
93.3
|
89.7
|
91.4
|
|
Percentage
registered
|
83.3
|
75.0
|
71.5
|
73.4
|
79.1
|
79.9
|
|
Average
age (years)
|
42.5
|
44.2
|
44.3
|
44.2
|
44.3
|
43.1
|
|
Average hours worked per week
|
32.8
|
31.7
|
32.3
|
34.1
|
37.8
|
32.5
|
[a] Includes 12,009 nurses who did not provide information
on the location of their main job.
Source:
Australian Institute of Health and
Welfare, Australia's Health 2006, p.327.
2.29
The distribution of dentists in Major Cities is more than three times
that in Remote and Very Remote areas with the rate dropping from 57.6 to 18.1 per
100,000 population.[19]
2.30
The Rural Doctors Association of Australia (RDAA) also commented on the
discrepancy between the levels of ill health that people in rural and remote areas
and the health dollars spent in those areas:
Even though rural and remote Australia has a more aged and a
'sicker' population there is less spent on their health needs compared to their
city counterparts. Medicare figures provided by the Department of Health and
Ageing also show that if you lived in a capital city that the average general
practitioner benefit paid per capita was $195 but if you lived in a remote area
of Australia that this figure falls to $120...Many specialist services are also
not available or viable in rural areas either because of workforce shortages,
low concentrations of patients or because they require the facilities of a
large hospital.[20]
2.31
While the analysis of rural services and workforce gives an indication
of the general limits to access, there are differences between jurisdictions
and within regions. The Australian Rural Nurses and Midwives (ARNM) explained:
There are considerable differences between states with regard to
the geographical spread of services. Remoteness factor cannot only be measured
by geographical location or distance; regional health services for example are
in much greater numbers in rural New South Wales, Victoria and Queensland as
opposed to Western Australia and South Australia. As such specialist services
in these states are only available in the capital cities.[21]
Diminishing services in regional,
rural and remote areas
2.32
Many witnesses noted that there has been a continuing diminution of
services in rural and remote areas with a decline in GP numbers and a downgrading
of hospital services. The Country Women's Association of NSW stated that:
With the down-grading of country and regional hospitals it is
now necessary for patients to travel greater distances. In the past it was not
unusual for specialists to regularly visit country and regional hospitals which
meant that patients were able to access locally many of the services for which
they now need to travel vast distances.[22]
2.33
The Shire of Sandstone provided an example of the decrease in access to
general practitioners:
In Mount Magnet the situation has become quite dire, in that,
from having a full-time general practitioner a couple of years ago, the town of
700 people is now serviced once a month by a visiting medical practitioner from
Geraldton who sees between 60 and 70 clients for one day a month. The nursing
posts have gone down from four nurses to one. It is a town which is
experiencing significant social and health problems in terms of drug and
alcohol abuse, which of course precedes child abuse.[23]
2.34
The Australian Nurses Federation (ANF) raised concerns about access to obstetric
services:
Access to health care also means access to services to assist
with normal life events, such as maternity and birthing services; the ANF is
very concerned that people in rural and remote Australia are being denied
access to birthing services with over 130 birthing services in country areas
closed in the last decade.[24]
2.35
The RDAA also commented that half of the obstetric services had closed
in the last 10 years which meant 'that many GP obstetricians and obstetrician
gynaecologists who want to provide services are unable to provide those
services in their community'.[25]
2.36
ARRWAG also reported a reduction in services being offered by GPs:
...there has been a decline in the proportion of GPs providing
procedural services – down from 24% in 2002 to 21.5% in 2005. Rural GPs have
traditionally been more likely to undertake procedures than their urban
counterparts because of a lack of specialists in rural and remote areas. A
decline in GPs undertaking this work may be a major factor in people living in
rural and remote areas having to travel to visit a medical specialist in
addition to an on-going decline in proceduralist GPs.[26]
2.37
WA Country Health Services indicated that workforce issues were impacting
on the delivery of services to the extent that a regional 'hub and spoke' model
had been introduced in an attempt to maintain service delivery levels:
Obstetric services are becoming harder to deliver. Anaesthetic
services are harder to deliver. General surgeons are in scarce supply; they
threw away the mould and they are not making generalist positions. Procedural
trained GPs that are willing to go out into the bush, which are the backbone of
our country hospital system, are not being made any more. I would contend, that
is just going to be the way the rural health service delivery is going to be.
That is why we have introduced a regional hub-and-spoke model because it is the
only way we think that you can try and maintain at least some services in a
region in the face of those workforce difficulties.[27]
2.38
However, witnesses commented that the hub and spoke model does not
always take into account the transport problems of the area. The Shire of
Ashburton WA stated:
The issues are: hub and spoke does not work because there is no
spoke in the sense that there is no public transport; there is no commercial
link or integration of any type whatsoever between any town in the Pilbara at
the air level; there is absolutely no land service of a commercial public
nature; and, all interaction is through private travel. We are talking about
extremely long distances and times. Most one way distances are 400 to 500
kilometres or more. This puts great pressure on patients because, the way the
system works, carers do not get a great deal of support through the PATS
system. Also, the road systems, the distances travelled, the safety risks from
animals on the road, the sheer heat and such types of things mean that it is a
test for an able-bodied, healthy person, let alone someone who is suffering an
illness.[28]
2.39
The Department of Health and Ageing (DoHA) cited two reasons for the centralisation
of services. Firstly, evidence shows that sufficient patient 'throughput' is
required to achieve 'safe and appropriate clinical outcomes'. To put it simply,
specialists need the opportunity to practice. Secondly, advances in medical
technology have resulted in the development of sophisticated procedures and
(often highly expensive) medical equipment. Due to the cost and degree of
specialisation, treatments are restricted to a few health centres:
Because of the needs for cost effective utilisation of expensive
equipment and/or to achieve and maintain clinical competence in complex and
costly procedures, it may be feasible to have only a limited number of
health-care establishments, such as hospitals, providing certain specialised
health services.[29]
2.40
Haematology services in Western Australia are an example of centralised
services:
Throughout regional Western Australia there are extremely
limited haematology services available. There is limited low level care
available in Bunbury and in Albany. These treatment areas provide only simple
administration of chemotherapy. They are not resourced for admissions of an
un-well immunised compromised patient.
No haematology patient diagnosed within regional WA would be
able to avoid multiple trips to Perth as is evidenced by the following list of
diagnostics and treatment that are not available elsewhere:
- all haematologist appointments.
- scanning and radiology
appointments.
- any nuclear medicine scans.
- chemotherapy regimes – either
preformed as inpatient or outpatient.
- admission to treat neutropenia
infections post chemotherapy.
- access to specialised physio;
dietetics; rehabilitation and psychological health professionals.[30]
2.41
While there may be sound reasons for centralisation, the lack of
services places greater pressure on rural GPs to provide more specialised
services and manage more highly complex cases:
Clearly, if patients do not have access to specialist care in
their community and they do not have access to, say, the Alfred or Prince of
Wales hospital, those patients end up being managed by the GP in their
community often without being able to get support from their specialist
colleagues. There are some money issues involved, but it is broader than that.
There are training issues as well. I think that we really have to make it
attractive for GPs to train in procedural specialties, that is, anaesthetics,
obstetrics.[31]
ARRWAG also concurred that work intensity was a problem with
attracting and retaining rural GPs.[32]
An increasing demand for PATS
2.42
Witnesses argued that the demand for PATS will continue to increase over
time as services in regional, rural and remote areas continue to decline, the
population ages and other issues such as more sophisticated and more expensive
medical technologies are introduced.
Future pressures on PATS
2.43
DoHA identified 'future pressures' that could impact on patient transport,
with more patients needing to travel to receive treatment:
- increased health needs of the ageing population;
-
increase in the number of patients with chronic conditions and,
consequently, complex health needs;
- advances in medical technology:
-
patient expectations of treatment available to them grows as
treatment becomes more effective and previously untreatable conditions become
treatable;
- highly specialised and expensive equipment is provided in limited
hospitals/specialist centres requiring patients to travel for treatment; and
- possible rationalisation of hospital and health services by State
and Territory governments.[33]
2.44
State and Territory Governments concurred with the majority of DoHA's observations,[34]
with the impact of the drought also identified as increasing demand. The Victorian
Government commented that the lack of access to Commonwealth-funded medical and
allied health services was also contributing to demand pressures, while South
Australia argued that 'the level of growth [in demand for PATS] is causing
increasing pressure on SA resources while the Australian Government
contribution has grown more slowly'.[35]
2.45
The Rural Doctors Association of Australia similarly noted that the
ageing population will impact on demand:
Chronic disease (conditions likely to persist for at least six
months) constitutes about 80% of the burden of disease in Australia today, a
figure which will rise with demographic ageing.[36]
2.46
At the same time, the ageing population is impacting on the medical
workforce with more than 50 per cent of the GP workforce in rural and remote Australia
aged over 45 years.[37]
As demographic ageing continues, there will be a relatively smaller pool of
professionals to attract to rural and remote areas.[38]
A changed operating environment
2.47
Witnesses argued that PATS as it was envisioned in the 1980s is no
longer sustainable. The environment in which PATS operates has changed
significantly. As discussed above, people in regional, rural and remote areas
have poorer health status than other Australians; there are significant
workforce shortages which are exacerbated by the need to centralise services
due to cost and technology imperatives; and ageing is impacting on both the
general population and the medical professional population. The WA Country
Health Service commented:
The difficulty I think for us is that we are losing ground. We
have had quite a lot of success in recent years but we are losing ground with
that strategy at the moment because the workforce shortages that we forecast
five years ago are now with us and they are getting worse. So we have lots of
vacancies, we have lots of services where the skills mix is skewed and out of
plumb; we have lots of services that are completely failed and we have some
that are so fragile they work some days and not on others. The Pilbara region
is absolutely in tremendous difficulty at the moment with fragile services. We
have enormous numbers of overseas trained doctors who are not familiar with the
Western Australian system and who have varying skills mix, so our services have
never been so challenged.[39]
2.48
The WA Country Health Service went on to comment that to try and operate
PATS in the same old way, 'where the services that would ordinarily be
available locally are sometimes there and sometimes not, is starting to create
some more tension'.[40]
2.49
The South Australian Government also commented on the changes in health
care delivery since the introduction of patient assisted travel schemes:
The schemes started from a base where they focused on access to
medical specialist services. Health care delivery has changed over the last 20
years and it is critical that PATS look towards expanding to include access to
primary and allied health care services. The cost implications of expanding
need to be considered and the Australian Government needs to provide its fair
share of funding support.[41]
2.50
In addition, the schemes have not evolved as advances in treatments and
care have evolved. A case in point is the treatment of cancer where access to a
multidisciplinary team increases survival rates and decreases adverse outcomes.
The NRHA stated that:
Complete cancer care often includes care coordination and
planning between medical, surgical and other cancer care specialists,
specialist investigative procedures, surgery, radiation therapy and
chemotherapy, with a range of frequencies and intensities, and monitoring
requirements. This is necessary for some conditions, in order to match a
subsequent therapy with the patient's response to an earlier treatment. Often,
acute side-effects are debilitating for the patient. A secure home-like
environment, whilst experiencing unpleasant side effects of some treatments
away from home, with support from relevant carer/s, will assist treatment
compliance and maximise benefit. The failure of the schemes to genuinely cover
essential care for many cancer patients probably contributes to poorer survival
rates in cancer among people in rural and remote areas.[42]
2.51
Other examples include access to coordinated treatment and support for
chronic conditions such as epilepsy, kidney disease and Parkinson's disease
where access to a range of allied health services can decrease the adverse
impact of the disease through physiotherapy, specialised nursing care and
occupational therapy.
2.52
At the same time, witnesses commented that it was short-sighted for
governments not to provide adequate access to health services as in the long-term
costs incurred were greater through health complications and economic loss and could,
in fact, undermine other health initiatives.
2.53
The RDAA argued that there was a 'compelling case' for increasing the
level of benefits because country people are 'just not getting the access that
they used to get'. Not providing good transport assistance schemes is a false
economy as the likely outcome will be additional health system costs being
incurred in both Federal and State funded areas. This is due to late treatment
of conditions and increased costs to the community associated with an increased
burden of illness and even avoidable and premature death.
In the long run, one would think, one would achieve better
outcomes. But it would be a lot less expensive for
the Commonwealth in the long run...if we were able to assist people to access
preventive care and screening in antenatal care and so on, thus saving money on
acute healthcare in the long run.[43]
2.54
The RDAA also noted that other initiatives could be undermined by the
lack of patient transport. For example, the Commonwealth Bowel Cancer Screening
Program – which enables people in any part of the country to be screened – is
not coordinated with follow-on care. People in rural and remote areas with a
positive test result still face enormous access issues in securing further
tests and treatment. RDAA research showed that following a positive screening
test a rural patient may have to wait six months or more to get a colonoscopy
which is 'a disaster for those people'.[44]
2.55
Dr Eduard Roos of the Southern Queensland Rural Division of General
Practice concluded that 'prevention is better than cure' and told the Committee
that:
...there is a cost saving if we can get the patient to see the
specialist sooner rather than later. So for us it is very important to make
sure that our patients can access the services.[45]
2.56
However, NSW Health argued that other factors such as 'access to carers
for children' and 'potential loss of income' impact on people's decisions about
how, when and if to travel to receive health care, as well as the adequacy of
the travel schemes. As such, NSW Health concluded:
[I]t would be extremely difficult to draw solid connections
between improved travel and accommodation support and clinical outcomes for
patients given the number of variables that affect a patient's clinical
outcomes.[46]
Conclusion
2.57
The health outcomes of people living in rural, regional and remote communities
are poorer than those in major cities in Australia. As discussed above, the
reasons for this are multifaceted and include a range of socioeconomic and
behavioural factors.
2.58
It is evident that rural, regional and remote communities are facing considerable
disadvantage in accessing services that those in major cities take for granted.
While the Committee acknowledges that many factors contribute to decisions to
travel (or not to) for treatment, the schemes that have been put in place to
assist with access should not themselves form a barrier to that access.
2.59
The Committee considers that, although there are considerable challenges
in providing services to a dispersed population, it is imperative that access
to services be improved. The failure to do so means health priorities are
undermined; costs to government may increase in the long term and most
importantly, the health status of those living in rural, regional and remote
communities will not be improved.
Navigation: Previous Page | Contents | Next Page