Chapter 3 - Appropriateness of joint funding arrangements
Introduction
3.1
This chapter will examine the appropriateness or otherwise of the current
joint funding arrangements under the CSTDA and focuses on the overall structure
of the arrangements. Issues in relation to unmet need are discussed in Chapter
4.
3.2
Part 6 of the current CSTDA outlines the responsibilities of the parties
to the Agreement. All parties have continuing responsibilities under the
Agreement for funding specialist services for people with disabilities. While
funding responsibilities are shared between the levels of government, the CSTDA
divides the responsibility for funding specialist disability services from
their administration. The Commonwealth has responsibility for the planning,
policy setting and management of specialist disability employment services. The
State and Territory Governments have responsibility for the planning, policy
setting and management of specialist disability services except employment
services. These services include accommodation support, community access,
community support and respite care.
3.3
The Commonwealth, State and Territory Governments also share
administrative responsibilities for planning, policy setting and management of
advocacy services, print disability services and information services as well
as participating in and funding research and development.[1]
The current agreement expires on 30 June 2007; a fourth CSTDA is in the early
stages of negotiation.
3.4
As part of their joint funding responsibilities under the current CSTDA
governments have committed $17.1 billion over five years. There is roughly a
80/20 split between the funding contributions of the States and Territories Governments
and the Commonwealth for specialist disability services other than employment
services. For example in 2005-06 $3.552 billion was made available under the Agreement.
This was made up of $1.056 billion from the Commonwealth and $2.496 billion
from the State and Territory Governments. Of the Commonwealth's contribution, $450
million was spent on the provision of specialised disability employment
services and $605 million was transferred to the States and Territory Governments
for the provision of specialist disability services other than employment.
3.5
The Commonwealth makes CSTDA funding available as financial assistance
to the State and Territory Governments as a Specific Purpose Payment (SPP). In
the Agreement, this funding is described as the total amount required to meet
the Commonwealth's responsibilities for the management and administration of
all specialist disability services other than employment, 'a global amount to
be allocated on the basis of need' by the State and Territory Governments.[2]
The Commonwealth does not impose any requirements on the way funds are
allocated, except that they are used to fund services that are eligible for
funding under the CSTDA.
3.6
The Commonwealth's other contributions to people with a disability and
their carers are not included in the CSTDA arrangements. These include income
support payments such as the Disability Support Pension ($7.9 billion per annum),
the Carer Allowance ($1.1 billion per annum), the Carer Payment ($1.1 billion
per annum), the Mobility Allowance and the Disability Pension for Australian
Defence Force veterans. People with a disability may also be eligible to receive
Commonwealth-funded services through the Home and Community Care Program (HACC)
or other services and the Commonwealth Rehabilitation Service. Both these
programs are also not part of the CSTDA arrangements.
3.7
Table 3.1 is extracted from the CSTDA and provides the funding
contributed by each party.
Bilateral Agreements
3.8
The Commonwealth has signed individual bilateral agreements with each of
the States and Territories under the current CSTDA. Bilateral Agreements were introduced
under the second CSDA. The purposes of these Bilateral Agreements are to:
provide for action on strategic disability issues; provide a continuing
procedure for negotiation and agreement between the Commonwealth and individual
States/Territories on the transfer of responsibility for particular services
from one level of government to another; and to bring into the scope of the
CSTDA specialist disability services not yet included.[3]
3.9
In practice, the Bilateral Agreements provide the Commonwealth with a
level of influence over the provision of State and Territory disability
services. Bilateral Agreements also create a degree of flexibility to the joint
funding arrangements, providing the opportunity to address specific issues such
as increased access to respite care for older parents caring for their sons and
daughters with a disability or the transfer of services between the levels of
government.
Table 3.1: CSTDA funding
contributions by jurisdiction
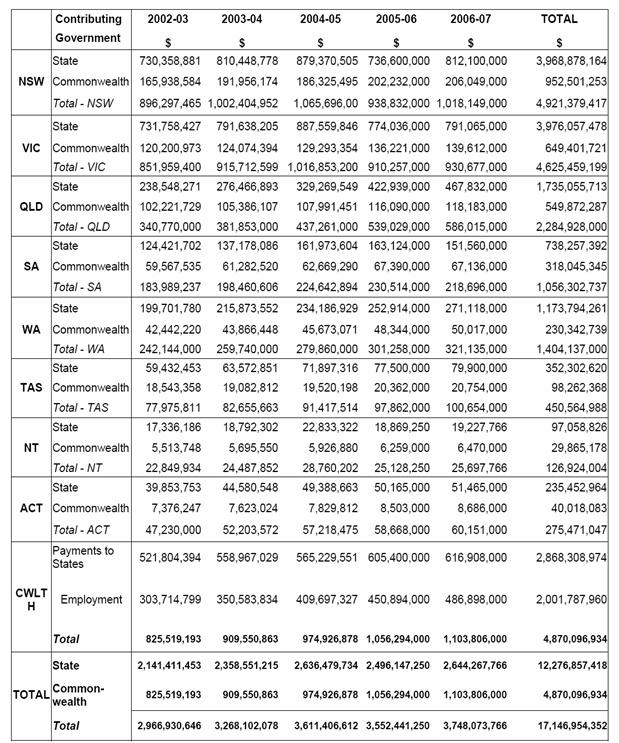
Source: Commonwealth State Territory Disability Agreement 2002 -2007, Schedule A1.
Joint funding arrangements
Responsibilities
3.10
The previous and current agreements have been recognised as clarifying
administrative responsibilities between the Commonwealth, State and Territory Governments.
However, many submissions identified problems with the joint funding
arrangements of the CSTDA, in particular the lack of clarity regarding the shared
funding responsibilities and accountability. The lack of clarity regarding
responsibilities for funding disability services was highlighted as enabling
both levels of government to shift responsibility for the inadequate funding of
specialist disability services.
3.11
The CSTDA arrangements divide responsibility for the administration (the
planning, policy setting and management) of disability services from
responsibility for their funding. However, for the purposes of accountability
for service delivery these roles are linked. The inadequate provision of
disability services can result from either inadequate administration or
insufficient funding. Submissions also noted concerns about where
accountability rests in the division between funding and administration
responsibilities in the CSTDA.
3.12
Consistently submissions and witnesses expressed frustration at the lack
of clear accountability in the CSTDA arrangements.[4]
Ms Di Shepard submitted:
The current bureaucratic split between State and Commonwealth
allows for endless 'argy bargy' about who is accountable. The States say they
are doing their bit, but the Commonwealth is falling short. The Commonwealth
says just the opposite. Frankly, I don't care about playing the 'blame game', I
just want the system to work. It can't work properly until there is a fixed
point of accountability.[5]
Mr Richard Deirmajer commented:
One of the biggest issues we have also had between the states
and the federal government is that, when we lobby the state government... the
states seem to blame the federal government because they are not getting enough
funding. So we go and see the federal government, and they blame the states.[6]
Ms Deidre Croft in her submission stated:
The States and Territories Governments have consistently
maintained that the Commonwealth/States and Territories Disability Agreement
was based on a commitment to joint funding of disability support services. The
Australian Government, on the other hand, continues to assert that the funding
of disability support services (other than employment services) is a State and
Territory responsibility.[7]
3.13
However, the NSW Minister for Disability Services the Hon John Della Bosca
noted the advantages of State and Territory government administration of
services in allowing a level of local accountability in the provision of
disability services.
I think that in general the states—and I am speaking for New South
Wales—are better placed to facilitate local planning and community engagement
and to make sure there is local accountability to provide those services
directly. We are the people—in the case of New South Wales—who are already
running significant public services and facilitating the non-government
organisations to participate in our programs.[8]
3.14
Many submissions and witnesses identified specific criticisms with
individual State and Territory governments in relation to specialist disability
services. Ms Brown of the National Carers Coalition commented on the 'shocking
performance' of the NSW Government in provided adequate funding for disability
services in the past.[9]
NCOSS cited the comparable information listed in the Report on Government
Services produced by the Productivity Commission to identify a number of areas
where NSW has low proportions of people with disabilities using disability
services.[10]
The Disability Advocacy and Complaints Service of South Australia described
their advocacy efforts for individuals who had severe shortages in their care
hours and urgently needed aids and equipment:
We sent 76 individual letters to the Minister, the Premier and
the Treasurer of South Australia. Three years on half of the urgent needs have
been picked up, the other half are still waiting.[11]
3.15
There was overwhelming evidence that there is not enough funding for
disability services but some witnesses commented that they believed that there
could be more effective delivery of services at the State and Territory level.
Inflexible interfaces
3.16
The nature of the division of administrative and funding
responsibilities for specialist disability services to each jurisdiction and
level of government has lead to different approaches to the provision of
services. In some cases it has created program silos leading to inflexible
interfaces between disability services at each level of government or
jurisdiction. NCOSS in their submission emphasised that this frequently did not
result in optimal outcomes for people with disability or their carers:
Government funding programs stream people into designated
service categories, eg disability services, residential aged care facilities,
community care etc. This streaming can serve to reduce the desired flexibility
of service provision thus promoting a system which is driven by the service
system and not by individual needs. Clients are accepted because they "fit"
the service provision, not the other way around.[12]
UnitingCare Australia commented:
The current demarcation between jurisdictional responsibilities
means that people wishing to transfer between options or undertake a mix of
options are required to negotiate their way through two different service
systems with differing policy and funding priorities.
A need exists to simplify the system to make it easier for
consumers to access and navigate. This means ensuring that improved pathways
between Commonwealth and State funded services are two–way thereby enabling a
smooth transition into and between programs and services according to people’s
changing needs at different times and life stages.
Cross jurisdictional approaches to service provision need to be
further developed to encourage people to experiment with new or a mix of
options without risking the security of their placement.[13]
Commonwealth services -
State/Territory services interface - transitions
3.17
The problems of inflexible interfaces in the current system were
highlighted by Jobsupport Inc. While the cap on the Commonwealth funded
Disability Employment Network can prevent those persons capable and willing to
work from attempting to enter open employment, the State funded Post School
Options program also discouraged people from attempting open employment by
making it difficult to return after leaving the program.[14]
Jobsupport stated:
Firstly, the Commonwealth program is capped, so everyone who
wants to work cannot work, even if they are capable of doing so and it would
save the taxpayer money and, secondly, the state government in turn tends to
want to shut the door behind people. In our view, there is an opportunity to
actually save money, to let the people who want to work do so, and all we
really need to get it together is a more flexible interface between the two
levels of government.[15]
3.18
ACROD also noted that this interface was 'problematic' and 'fraught with
risk' for people with disabilities involved in employment transitions such as supported
employees seeking retirement or people moving from post-school option programs
to open employment.[16]
State/Territory services interface
– portability
3.19
A concern repeatedly raised with the Committee was the portability of
disability services and benefits to other States or Territories. Witnesses
expressed their frustration at the lack of consistency and equity in the availability
of services between jurisdictions. For example Mrs Jean Tops of the Gippsland
Carers Association stated:
'You are not a citizen of Australia. You are only a citizen of
the state in which you live'...If you leave Victoria, you cannot take any of your
services with you. You will have to start again on the waiting list in the
place you are going to get a service back. That ties families to the state in
which they live, to the region in which they live and to the services that they
currently have.[17]
3.20
In July 2000 a National Disability Administrators paper 'Moving
Interstate: Assistance to People with Disabilities and their Carers' in
relation to the portability of funding for disability services was endorsed at a
meeting of Ministers responsible for Disability Services. These recommendations
provided that: individuals seeking to move interstate may access that State or
Territory's service through transparent demand management processes based on
relative priority of need; individuals may register their request for service
prior to any planned transfer; and where the move is urgent, unplanned or due
to circumstances beyond the control of the individual, the State of origin
agrees to give consideration to the transfer of funds for up to 12 months.[18]
3.21
In practice these provisions do not appear to have provided a real
choice for people with disability who wish to move between jurisdictions. Mr John
Nehrmann of the Department of Health and Human Services in Tasmania commented:
In terms of clients or consumers there is a huge level of
uncertainty if you want to move. As I said, initially all you are getting is 12
months and then you have to hope you are getting the same level of service at
the same time. The other issue is that you are not always able to get the same
type of service from one jurisdiction to another. You might have an individual
funding program in one jurisdiction that allows you to buy certain services
that include certain things and yet when you move suddenly there are different
business rules and different things covered. Even though the program is roughly
the same, it is not quite the same.[19]
3.22
Ms Raelene West also indicated the current CSTDA funding framework was
'highly problematic' for people wishing to move jurisdictions:
Service recipients are often forced to renegotiate an entirely
new system of programs and services, and receive differing and often only
entitled to reduced levels of funded services if living in another
State/Territory other than original 'jurisdiction'.[20]
3.23
However there were also links made between the level of unmet need for
disability services and the lack of portability of services. Ms Lois Ford of the
ACT Government commented:
The assessment of need is based on the level of need the
individual has and the resources that we have available—and I would say this is
true for most states and territories—to meet that need. I guess that it is more
about meeting demand and growth within disability services so that people with
disability can transfer or shift from place to place like any other citizen. I
would suggest that it is less about the portability of funding and more about
demand for and growth of services in each area.[21]
3.24
While the problem of portability has been recognised in the past, moving
between jurisdictions is still extremely difficult because of the complexities
of needing to negotiate new services within a different system combined with
differing limitations on resources arising from underlying levels of unmet
need.
Recommendation 1
3.25
That State and Territory governments provide a specific service that
assists people with disability transferring between jurisdictions to negotiate
programs and services to achieve a comparable level of support.
Dual diagnosis and multiple
disability
3.26
The Committee was also concerned about implications of the lack of
flexible interfaces in the provision of services for people with disability
requiring services in relation to other health needs. Brightwater Care Group
commented:
Dual diagnosis is a challenge whether it is somebody who has
palliative issues, mental health issues or substance abuse issues—even if you
are Aboriginal, basically. As soon as you have an issue that puts you with a
bit of a foot in both camps, you find that neither camp wants you and can find
strong reasons for you to belong somewhere else. It is the need to break down
those jurisdictional boundaries and get agencies and funding organisations
talking to each other to see how to address the issues.[22]
3.27
However Dr Ken Baker of ACROD highlighted the problems facing service
providers caring for people with disability who also had other care needs:
People can rarely be neatly slotted into one box and not others...I
think the main complaint from among disability service providers is that they
are expected as disability service providers to respond to the total needs of a
person, and that is not really what they are equipped to do. They would have to
respond to a person’s mental health or drug and alcohol issues as well as their
disability rather than getting easy access to another system. In a sense, it is
an institutionalised view of governments that, once you are in the disability sector,
that is the institution that has to take total care of you. I think that is a
flawed view, but it is also, in a way, a dangerous view because it is
preventing a person from getting access to other service systems which ought to
be responsive to their disability.[23]
3.28
Mr Arthur Rogers of the Victorian Government commented on the definition
of disability in the Disability Services Act 2006:
Certainly in our operational practice there is no impediment to
people, as long as they have a disability within the meaning of the Act. So if
they had a mental illness they would not get in, but if they had an
intellectual disability and a mental illness we would cover them for the disability.
Part of the difficulty around service provision is that where
people have multiple disabilities they have complex support needs and they do
not fit into some of the more generalist services. By 'generalist' I mean a
house catering for people with an intellectual disability. A person with an
intellectual disability and a mental health issue and maybe a physical
disability has quite specific needs. You need to make sure that the service
response is tailored to those needs, not just to intellectual disability. So I
think the issue is the complexity of their support needs rather than the
definition in the Act.[24]
3.29
There appears to be two problems emerging in relation to the recognition
and support of people with dual or multiple disabilities: the first is where
the interaction of multiple disabilities means that existing programs and
services are ill-equipped or unable to meet the complex, higher level needs of
a client; the second is the issue of 'handballing' where existing programs or
services are suggesting the existence of a second disability is an excuse to
pass-the-buck to another program or service and effectively deny support. There
is also a clear need to provide appropriate specialised services.
Recommendation 2
3.30
That the next CSTDA clearly recognise the complex and interacting needs
of, and specialist services required by, people with dual and multiple
diagnosis, and people with acquired brain injury.
Complexity and overlap
3.31
The division of funding and administrative responsibilities between the
Commonwealth, State and Territory Governments creates overlap and duplication
in bureaucratic and administrative arrangements for the provision of disability
services as well as a lack of uniformity and equity between jurisdictions. In
her submission Ms West commented:
Each of the States/Territories 'jurisdictions' continue to fund
disability services at different rates and with differing levels of
accountability. Each State/Territory is governed by differing legislation with
differing obligations and priorities to users. This is despite a national
population of only 20 million people and with only a relatively small
percentage of this population utilising some form of funded disability service.
Under the current form of CSTDA funding, each state continues to roll out their
own gamut of programs, services, strategies and policies, creating further
inequities in the system on a national level. Service delivery on the ground
therefore continues to be disparate, with real mapping and contrasting of
service delivery remaining difficult.[25]
3.32
The complexity in the arrangement under the current CSTDA also causes additional
burdens for disability services users. Ms Teresa Hinton of Anglicare Tasmania,
who had recently completed a research project on disability services, commented
on difficulties with the fragmented nature of services.
To receive personal care and support, somebody might be dealing
with three or four different agencies, each with their own assessment process,
different disability support workers and so on. Being able to coordinate that
for individuals was very problematic and difficult for them, for individuals
and also carers who might have been taking on the case management role.[26]
Cost-shifting
3.33
During the inquiry a number of issues regarding cost-shifting between
the levels of government were raised. Cost-shifting may occur where funding
arrangements allow responsibility for services to transfer to a program funded
by another party without their agreement. The complex arrangement of the
division between the levels of government of responsibilities in relation to
areas which overlap with disability such as health, ageing, employment and
education may provide opportunities and incentives to shift the costs of
service delivery. Cost-shifting between governments can also contribute to
problems such as accountability for disability services.
3.34
ACROD encapsulated this issue by stating in its submission that:
For governments, funding is clearly a contentious issue. In the
past, negotiations have been marred by suspicions of cost-shifting and
accusations from each level of government that the other provides less than its
fair share of funding for State-administered services.[27]
3.35
The Commonwealth pointed to an increased usage of services under the
Home and Community Care (HACC) program by people with disability.
People with disability are estimated to comprise over 24 per
cent of the total number of HACC clients. However, they are estimated to
consume 30 per cent of the funding because proportionately more people
with disability access higher levels of service.
The proportion of younger people (those under 65 years)
accessing HACC services has increased from 18.5 per cent in 1994-95 to over 24
per cent in 2004-05. Given that the percentage of young people in the general
population has declined over the same period, the growth in young people as
HACC clients suggest that outside of HACC, disability services delivered by the
states and territories have not grown in line with demand.
CSTDA data indicates that there has been significant decline in
the number of service users aged 60-64 years compared to those aged 55-59 years
across all CSTDA funded service types...There is a concern that this decline
reflects a trend for older people with disability ending up in inappropriate
aged care or hospital services due to a lack of appropriate disability
services.[28]
3.36
Ms West also identified that shortfalls in State and Territory disability
services had "forced" people with disability to utilise HACC program
services.
Ideally, a significant expansion and increase in funded
disability services could move people requiring disability services off HACC
funding and onto specific disability support programs and funding arrangements
alone, increasing clarity of service need and providing specialised disability
support.[29]
Whole of government coordination
3.37
The need for better coordination between Commonwealth, State and
Territory jurisdictions and departments was also raised with the Committee. The
responsibility for ensuring that Commonwealth and State/Territory programs are
having a complementary impact is shared by all the parties in the current
CSTDA.[30]
Ms Lyndall Grimshaw of Brain Injury Australia commented:
If we look at government policy and program development, what we
see is fragmentation and program silos...There is little evidence from our
perspective of interdepartmental cross-policy program collaboration, both
across and between the Commonwealth and state and territory levels.[31]
3.38
The point was made that despite the interrelationships in the services
covered by the CSTDA, such as health and employment, the only Commonwealth
Department a party to the Agreement was the Department of Families, Community
Services and Indigenous Affairs ( now FaCSIA). The Department of Health and
Ageing and the Department of Employment and Workplace Relations have not been
parties to the CSTDAs. ADFO for example commented:
A major barrier to the effective oversight of progress towards
the achievement of the aim of the CSTDA has been that no single agency has been
given the task and authority to do this. At a Commonwealth level alone, direct
services to people with disability are provided by at least seven departments
and most of these are not involved in the Agreement.[32]
3.39
In 2004 responsibility for administration of open employment services
operating under the CSTDA moved from the Department of Family and Community
Services (now known as FaCSIA) to the Department of Employment and Workplace
Relations. Supported employment services for people with disability continue to
be administered by FaCSIA. MS Australia commented that as a result of this
change:
FaCSIA remains the lead Agency at the Australian Government
level in regard to disability services despite being the smallest and least
involved agency in the delivery of disability services. This is a situation
that has definitely hindered development of the sector, due to its inability to
lead and champion disability issues across Australian Government portfolios
including employment, education and health.
This problem is mirrored in the States where key areas such as
infrastructure, transport and health are not directly included in the CSTDA
work of the lead disability departments who are CSTDA signatories, and where
the general policy response is limited.[33]
3.40
ACROD commented:
Governments are hierarchical entities. If a whole of government
approach is to be effective it needs to become a priority of central government
agencies and, ultimately, requires leadership by the heads of government.[34]
3.41
The Mid North Coast Disability Committee also suggested there is potentially
a greater role for local government in the delivery and co-ordination of
specialist disability services.[35]
3.42
Governments are working at improving the coordination of disability
services. At the July 2006 meeting of the Community and Disability Service's
Ministers' Conference, Ministers agreed on three priority areas of shared
concern that would likely benefit from national collaboration for a fourth
CSTDA. These were service improvement, demand management and interface issues.[36]
A national approach?
3.43
The argument was made to the Committee in a number of submissions that
problems associated with the CSTDA joint funding arrangements may be addressed
if the Commonwealth assumed sole responsibility for funding of services in
relation to disability.[37]
These arguments reflect long-standing and on-going debates regarding the
balance of Commonwealth, State and Territory responsibilities for Australia's
health care system and the issue of cost-shifting.[38]
3.44
A Commonwealth 'take over' of disability services was seen as broadly
addressing a number of perceived systemic problems with the current joint
funding arrangements. These included greater accountability, a uniform approach
service delivery, the more equitable allocation of disability services and
improved co-ordination across service systems. Ms West elaborated on the
advantages of a national approach in her submission:
Benefits would appear to be considerably improved
standardisation and uniformity in the level of funded disability service
programs, increased coherency and consistency of available services and clearer
expectations for clients as to available services and resources. In terms of
administration, a national approach would significantly reduce as previously
highlighted, difficulties with managerial assessment, contrasting accounting practises
and data collation and analysis.[39]
3.45
Submissions, particularly from the Commonwealth, State and Territory Governments,
while acknowledging problems existing in the current system, emphasised the benefits
of joint funding arrangements. They noted that the CSTDAs have been successful
in ensuring that all jurisdictions have specific funding available for people
with disabilities and that where jurisdictions are clear on their responsibilities
and sufficient funding is made available there have been significant outcomes
for people with disabilities.[40]
For example the Western Australian Government commented:
The CSTDA has allowed the Commonwealth, States and Territories
to maintain a focus on disability and direct resources specifically to meeting
the needs of Australians with a disability to an extent that was not occurring
before the existence of these agreements. While that in itself should not be
held as the only argument for the continuation of the multilateral agreements,
it is strong evidence in support of specific collaborative funding arrangements
for disability services.[41]
3.46
Similarly the National Ethnic Disability Alliance noted that 'Commonwealth
and State/Territory joint responsibilities in funding and providing disability
services should be maintained for better accountability and Commonwealth/State
coordination'.[42]
3.47
ACROD also noted the serious weaknesses in the CSTDA but continued to
support a joint arrangement. Dr Baker commented:
...we support governments negotiating a fourth Commonwealth
State/Territory Disability Agreement. We think that the original CSTDA was an
improvement on the system it replaced, and there have been some subsequent
improvements. Having said that, we believe that the fourth agreement ought to
be substantially reformed...[43]
Competitive federalism
3.48
An issue which was not discussed in many submissions was that of
competitive federalism. The decentralisation of responsibility for disability
services to the State and Territory Governments provides them with flexibility
to address local issues and increased opportunities for innovation in policy.
It also provides a competitive environment where the best policies once
introduced and tested by one jurisdiction can be adopted by other
jurisdictions. State and Territory Government policies in relation to
disability services are comparable which creates a competitive pressure on
underperforming jurisdictions to match the 'best practice'. NSW Minister for
Disability Services the Hon John Della Bosca commented:
I am a fan of competitive federalism. That might sound like a
very old-fashioned idea but I think there is some merit in the idea of six
different systems in a range of areas, provided there is a reasonable
harmonisation...[44]
A federal dilemma
3.49
In 2005 the Productivity Commission conducted a Roundtable on
'Productive Reform of the Federal System' which focused on issues associated
with the challenges of securing better policy outcomes from Australia's federal
system of government and included some examination of options for systemic
change in health reform.[45]
Some of the discussion is readily applicable to consideration of the CSTDA
joint funding arrangements.
3.50
A key feature of the current federal system in Australia is that the
States have broad spending responsibilities but few revenue sources whilst the
reverse is true at the Commonwealth level. The difference between the relative
revenue and spending responsibilities of the Commonwealth and States is known
as vertical fiscal imbalance.[46]
In the CSTDA the State and Territory Governments contribute the majority of
funds for specialist disability services other than employment and have
administrative responsibility. However because of factors relating to vertical
fiscal imbalance and recent budget surpluses the Commonwealth was perceived by
some as having a greater financial capacity than the State and Territory Governments
to fund specialist disability services and swiftly address unmet need.
3.51
A number of possible options for health reform were identified by Mr Andrew
Podger. These options included: the States taking full responsibility for
health and aged care services; the Commonwealth taking full financial
responsibility for health care; the Commonwealth and States pooling their funds
as regional purchasers; and a 'managed competition' model where Commonwealth
and State funds are available for channelling through private health insurance
funds by way of 'vouchers' which individuals may pass to the fund of their
choice.[47]
3.52
Mr Podger's view was that it was feasible for the Commonwealth to take full
financial responsibility and identified a number of the possible benefits of
such a proposal. These included allowing a single Commonwealth minister and
department to control the national management and delivery of services. This
would increase accountability for services and operate to reduce cost-shifting
and duplication. Such an approach would also address the problems created by
vertical fiscal imbalance by having the revenue raiser as the primary purchaser
of services. It would also reflect a trend towards increasing Commonwealth
control over health care.
3.53
However, Mr Podger also noted costs and risks in a Commonwealth 'take
over' of health services. It would require significant expense and a lengthy
transition period for the Commonwealth to take over control of State and
Territory personnel and facilities as well as to establish new administrative
structures which allowed for regional and community flexibility and input. The
proposal would also involve complex renegotiation of current tax revenue
arrangements.
3.54
In 2006 the House of Representatives Standing Committee on Health and
Ageing tabled The Blame Game: Report on the inquiry into health funding
which also examined proposals for reforming federal arrangements in relation to
health care.[48]
A key recommendation from this report was that Australian governments
develop and adopt a national health agenda. Part of the proposed national
health agenda would be to identify policy and funding principles and
initiatives to: 'rationalise the roles and responsibilities of governments,
including the funding responsibilities, based on the most cost-effective
service delivery arrangements irrespective of governments' historical roles and
responsibilities'.[49]
Conclusion
3.55
The current and previous Agreements have demonstrated a commitment on
the part of all Australian governments to ensure that resources are specifically
allocated for the provision of specialist services to improve the lives of
people with disability.
3.56
The Committee supports a fourth disability agreement between the
Commonwealth, State and Territory Governments. The State and Territory Governments
continue to have the service delivery expertise and can be more responsive to
the needs of people with disability and carers within their jurisdictions.
3.57
However there is clearly a need for improvement in consistency, equity,
coordination of specialist disability services as well as accountability,
performance monitoring and reporting. In these areas the Commonwealth is best
placed to perform a leadership role. The Commonwealth also possesses the
capability through the Bilateral Agreements to achieve better results in these
areas.
3.58
The Committee notes that the ANAO audit of the administration of the
CSTDA found evidence that the Bilateral Agreements had improved coordination
with relevant State and Territory Government disability agencies and considered
the Bilateral Agreements have the potential to be an effective coordination
mechanism for the Commonwealth's lead agency to work with State and Territory
agencies.
3.59
The Committee notes that Bilateral Agreements between the Commonwealth
and State and Territory Governments for funding of disability services will
often necessarily affect the provision of other disability services as well as
other publicly funded services. Where possible Bilateral Agreements should not
skew or distort the broader objectives of the CSTDA.
3.60
The Committee also notes that the Commonwealth may potentially have more
capacity to control and co-ordinate disability services if it increased the
proportion of Commonwealth funding to CSTDA services. ANAO also noted:
The fact that the Australian Government only provides 20 per
cent of the funding for services administered by the States and Territory
governments limits its roles, and the amount of influence it has over the
delivery of those services.[50]
3.61
The Committee recognises that the present funding arrangements assign
the States and Territories the primary responsibility for funding specialist disability
services and the Commonwealth responsibility for funding disability employment
services, with some Commonwealth supplementation of the States and Territories'
role. However these arrangements are problematic, and have generated
considerable uncertainty within the disability community about where services
can be found, what criteria for eligibility apply and which government bears
responsibility for its proper funding. The next CSTDA must as a priority,
remove this uncertainty and create transparent lines of responsibility.
3.62
Options for large-scale reform to the current CSTDA joint funding arrangements
may offer more challenges than solutions. The Committee recognises that any
reform is not without cost or risk and that any new arrangement or division of
responsibilities will necessarily involve some service delivery problems. Any
major change to the structure of joint funding arrangements under the CSTDA
should be accomplished as part of a broader restructure of Commonwealth, State
and Territory health and community care responsibilities.
3.63
However despite these concerns the Committee agrees the CSTDA could be
utilised more broadly to improve the lives of people with disability. The
Committee supports the AFDO's comment that:
...the CSTDA is far from being a coordinated, high level strategic
policy document. Despite its broad aim and the priority placed on access to
generic services, the current CSTDA retains a narrow focus on service delivery,
particularly disability-specific services, to people with disability aged under
65 years. The CSTDA is crisis driven, with the result that short-term,
individually focussed interventions are prioritised over systemic reforms.[51]
3.64
A renewed national disability strategy could function to coordinate the
objectives of the Commonwealth Disability Strategy and the disability policy
frameworks which have been developed by many of the States and Territories,
such as Victoria's State Disability Plan. By providing a coordinating framework
for various policies, programs, legislation and standards the next CSTDA may
enable effective responses to be developed to the complex issues which people
with disabilities face.
Recommendation 3
3.65
That the next CSTDA should include –
- A whole of government, whole of life approach to services for
people with disabilities.
- A partnership between governments, service providers and the disability community to set policy priorities and improve
outcomes for people with disability.
- A clear allocation of funding and administration responsibilities
based on the most effective arrangements for the delivery of specialist
disability services.
- A clear articulation of the services and support that people with
disability will be able to access.
- A commitment to regular independent monitoring of the performance
of governments and service providers.
- A transparent and clear mechanism to enable people with
disability and their carers to identify and understand which level of
government is responsible for the provision and funding of services.
Recommendation 4
3.66
That in the life of the next CSTDA, signatories agree to develop a National
Disability Strategy which would function as a high level strategic policy
document, designed to address the complexity of needs of people with disability
and their carers in all aspects of their lives.
Assessment
Assessment and planning
3.67
The Committee was concerned at the apparent lack of connection between
assessments being undertaken and the planning by governments for the needs of
people with disability. Assessments would seem an appropriate method for
governments and service providers to budget and plan services as well as to
give people with disability and their carers a level of certainty. Mrs Franklin
highlighted the approach taken by the United Kingdom to lifelong assessment and
planning.
When the child is born or diagnosed with a disability, you are
assessed and they put a care package together. Then they reassess it when the child
is going to school and they either take some of that care package off them or
add to it, depending on the disability. Then at the end of primary school they
are reassessed. Two years before they leave high school they are assessed, and
what they look at there is accommodation and employment—all of that.[52]
3.68
This approach could be contrasted with the experience of many Australian
families. Ms Allen commented:
The maze to find services was an absolute nightmare and actually
was the most energy-zapping situation that you can imagine. Rather than having
that time to give to my child, I found myself fighting the bureaucracy almost
every minute of the day. There was no plan for us and there was certainly no
plan for Simon. We had to negotiate for everything that we got. We had to
emphasise the negative the whole time. We had to make it sound actually as bad
it was and it was very hard for people to actually realise what we were going
through.[53]
Application procedures
3.69
Another assessment issue raised was the procedures involved in the
applications for State and Territory disability services. While practices
differ between jurisdictions these application and eligibility procedures often
rely on people with disabilities or their carers filling out detailed forms
setting out their circumstances and needs in order to be assessed for eligibility
and access to disability services. These forms are then assessed on a
competitive or criticality of needs basis to determine who has access to disability
services.
3.70
These can be highly distressing for families members required to
describe a loved one negatively, focusing on how caring for their needs is a
burden to them.[54]
People with disability and their families are also forced to 'compete' for the
available disability services against other equally deserving families. Ms Croft
commented:
I think there are a number of consequences of having a competitive
or criticality of needs basis for service provision. One is that family carers
are required to portray the needs of their family member with a disability in
the worst possible light, as being a burden on them and their family, and I
think that has enormous implications. There is a risk of devaluing people with
disabilities. I think also it requires an enormous bureaucracy to supervise who
gets funding on whatever level of critical need, so providing services on the
basis of pitting people’s needs against each other consumes resources and has
an effect even in terms of simple human dignity. I hear so many parents
expressing views about having to compete against people that they recognise are
also experiencing great hardship. They feel guilty about that. But also it is a
matter of who can demonstrate that their crisis is worse than someone else’s
crisis, which is not a dignified way in which services should be provided. It
also means that we have lost sight of the rights and needs of people with
disabilities and instead we are focusing solely on how healthy or strong their parents
or their carers are...[55]
3.71
The Committee is also concerned that some assessment procedures for
access to disability services appear reliant on written applications. These
procedures disadvantage people with poor literacy or communication skills,
often the people in the most need of assistance. An example given by Mrs Franklin
from Committed about Securing Accommodation for People with Disabilities (CASA)
highlighted this concern:
I have been helping a family—a Vietnamese lady; she has a son
with severe disabilities, her husband is dying of cancer and another son has
had kidney transplants. Because she cannot articulate on a piece of paper and
because of her cultural background—she does not like to ask for help—she keeps
getting knocked back in the funding round. If a team had gone out and assessed
the child with the disability and looked at the family in general she would
have got funding a long time ago.[56]
3.72
The Committee was interested in the potential benefits of utilising
information technology and the internet to reduce the burden that people with
disability and their carers carry in relation to communicating their needs to
services providers. An Adelaide based disability organisation 'Life is for
Living Inc' are currently running a project 'What I'd Like You To Know About
Me!'[57]
The project created a CDROM resource kit for service providers that focused on
capturing holistic and positive information about people with disabilities. The
information collected by the resource could then be printed and shared with
others such as family and friends, teachers, therapists, health professionals
and community members.[58]
For example, "Who are the members of my family?" "When
I go to hospital, I need this," "This is how I like to be cared for",
and "These are my favourite toys." It is written from the perspective
of the person with the disability. It empowers the family and the person with
the disability to put their own story forward. It can be used by health
services and other service providers to talk to the child when they are in
hospital, for example.[59]
A National Framework
3.73
The ANAO audit of the administration of the CSTDA noted that:
The States and Territories, and the Australian Government, have recognised
that there: "is currently no one conceptual model adopted by jurisdictions
that assesses eligibility, support needs and priority for service at both a
systemic and individual level".
This situation has resulted in a lack of national consistency in
how individuals’ needs for services are identified and in determining priority.
The ANAO considers that, in this circumstance, there is a significant risk that
services provided under the CSTDA may not be provided to those recipients in most
need across Australia.[60]
3.74
Carers Australia also highlighted the need for national consistency in
assessments of eligibility, support needs and service priority.
Carers Australia believes that the new CSTDA should include a
national framework for the provision of services to meet the needs of people
with disabilities in Australia. Such a framework should take a holistic
approach to the needs of the person with a disability and their carer, and be
based upon person-centred assessment. It should also recognise that many people
have more than one disability and different services are often required to meet
these different conditions.[61]
3.75
The National Disability Administrators Research and Development Program
was undertaking a project National Assessment and Resource Allocation
Framework with the purpose of developing 'a flexible, nationally-consistent
system which ensures a fair, transparent, consistent and rationale-based
allocation of resources that will also assist in understanding and managing
demand for disability services.' The Committee understands this project has now
been cancelled.
A Disability Assessment Team?
3.76
A key issue for the Committee was the importance of assessing the needs
of people with disabilities. Without an accurate and comprehensive assessment
of the care and support needs of each individual it seems impossible to
determine which specialist disability services or other services they should be
able to access. This basic information also appears crucial to a number of the
other issues raised in the inquiry.
3.77
Accurate and comprehensive assessments of the needs of each individual
with a disability could assist in:
- tailoring available services to meet an individual's specific
needs rather than fitting people to services or programs;
- enabling governments to plan services and funding by clarifying
the needs of people with disabilities in their jurisdiction;
- preventing cost-shifting between the levels of government by
independently assessing the services a person should be able to access;
- informing people with disabilities about the services which they
are eligible to access and facilitating access to those services;
- determining eligibility and priority through an equitable process
to ensure resources are delivered to those in the most need as well as reducing
the burden on family carers in making applications for services
- collecting additional data concerning unmet need in each
jurisdiction as well as making governments accountable for inadequate funding
or provision of specialist disability services; and
- recognising and addressing the special needs of people with dual
and multiple diagnoses.
3.78
The approach of the Aged Care Assessment Teams (ACATs) involving
face-to-face comprehensive functional assessments of individuals was generally
supported during the inquiry. ACATs are multi-disciplinary and can include
health professionals such as medical officers, social workers, nurses,
occupational therapists and physiotherapists. The objective of the Aged Care
Assessment Program is to 'comprehensively assess the needs of frail older
people and facilitate access to available care services appropriate to their
care needs.' Proposals were raised for a similar approach to assessments for
people with disabilities and their access to services.
Recommendation 5
3.79
That the next CSTDA incorporate a nationally consistent assessment
process to objectively and comprehensively determine the support and care needs
of each person with a disability. These assessment processes should also assist
people with disability by making determinations of eligibility for services and
priority of need as well as facilitating access to appropriate services.
The burden of multiple assessments
3.80
The Committee was concerned to hear of the issues people with
disabilities and their carers had with assessment procedures for access to
disability services. A common complaint was the need to continually repeat
information regarding disability care needs to service providers and care
workers or to frequently attend assessments in order to access disability
services. This was particularly burdensome for people with permanent lifelong
disabilities and their carers. Ms Stagg explained to the Committee some of the
challenges of caring for her daughter Michelle:
All I want is a piece of paper that says, "Has anything
changed?"—"No," tick, the doctor signs it and you go. That sort
of stuff is frustrating all the time...Somebody who starts this from birth has to
go through that again and again...I really do not know how you are going to get
away from that, but there must be some way of facilitating people from day dot
to help them through the system...[62]
3.81
Mrs Griffin repeated these concerns regarding assessment procedures in
relation to her son Scott:
One of the things that I find most frustrating is being sent
forms continuously and having to restate that nothing has changed with Scott.
The fact is that nothing is going to change. He is not going to suddenly get
better. He has a genetic deletion that is there and will be there and is never
going to change, so his needs are always going to be as they are, if not worse
as he ages. It would be nice if some of that could be understood so that it was
broader than a particular disease. It needs to be understood so that once a
person is diagnosed with something like a genetic deletion that is never going
to change you do not have to spend your whole time begging for equipment or
begging for help. It should be on record that this child needs help ongoing,
long-term, until the day he dies.[63]
3.82
This issue appeared to be the result of the complexity of the
administration disability services as well as inefficient assessment procedures
and information sharing by disability providers and agencies. This is an issue
complicated by administrative requirements and by privacy laws designed to
protect the private health information of all Australians. The Committee agrees
that people with permanent lifelong disabilities and their carers should not be
required to repeatedly 'prove' their disability in order to obtain disability
services. Where possible they should be given the choice to consent to their
assessment information being shared and utilised in the most administratively
effective fashion.
Appropriate Assessment
3.83
The specialised assessment needs of people with chronic degenerative
diseases such as Motor Neurone Disease and Multiple Sclerosis were also raised
with the Committee. The degenerative nature of these conditions means the
assessment of current and future need for disability services was problematic.
Changes in their needs for disability services and equipment were often sudden
and unpredictable. Long waiting periods for assessment and access to services
was inappropriate for the changing nature of their conditions.
Recommendation 6
3.84
That the Commonwealth, State and Territory governments ensure that:
- administrative burdens of assessment procedures are reduced for
those with lifelong and permanent disabilities and their carers; and
-
flexible assessment options are available to people with
disabilities who have needs that may change rapidly.
Indexation of CSTDA funding
3.85
A number of submissions raised the issue of indexation of CSTDA funding,
particularly in relation to Commonwealth contributions.[64]
Indexation (or price adjustment) is intended to change funding to take account
of changes in the cost of services over time so that providers can continue to
offer the same services.
3.86
Part 8(10) of the current CSTDA provides that indexation of Commonwealth
funds to be transferred to the State and Territory Government are calculated
each year by reference to the Commonwealth indexation parameter Wage Cost Index
2. The Commonwealth indexation of CSTDA funding based on Wage Cost Index 2 was
2.1 per cent for 2005/06 and 1.8 per cent for 2006/07. The decision about
which indexation rate is applied to Commonwealth CSTDA funding is made by the
Department of Finance and Administration. The State and Territory Government
indexation of their CSTDA funding varied.
3.87
Table 3.2 outlines the indexation rates applied to CSTDA funding by each
jurisdiction.
Table 3.2:
CSTDA indexation rates by jurisdiction 2005/06 and 2006/07
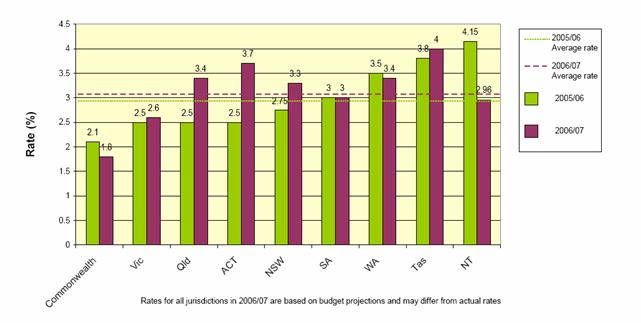
Source: Western Australian Government, Submission 3,
p.18.
3.88
Many submissions to the Committee argued that the Commonwealth's rate of
indexation was unrealistic and insufficient to keep up with increased costs
(particularly wages) in the disability sector. The consequences of indexation
rates applied to CSTDA funding which did not reflect increases in costs in the
provision of disability services were also highlighted. In particular an
inadequate rate of indexation applied to CSTDA funding could gradually erode
the real value of the base funding and affect the viability and sustainability
of disability services.
3.89
NCOSS stated in their submission:
Certainly, previous indexation rates have not compensated for
increases in costs, including wages, activities and overheads, as well as
external impacts such as insurance, workers compensation and fuel prices etc.
This has resulted in a pattern of consistent underfunding with the net effect
being diminished service capacity.[65]
3.90
Dr Baker from ACROD identified the problems that inadequate indexation
of CSTDA funding could cause for disability service provider staffing:
The cumulative effect of this gets worse and worse as time
proceeds and makes it more and more difficult for disability service providers
to recruit and retain staff. This has now reached quite critical levels within
the sector...we need first of all to provide service providers with enough
capacity to recruit, train and retain quality staff. That cannot be achieved
while they are having to manage what is in effect an annual funding cut.[66]
3.91
Some State and Territory Governments argued that the level of indexation
applied by the Commonwealth to CSTDA funding has operated to gradually shift
the funding burden to them. The Queensland Government also highlighted the
Commonwealth's application of different indexation rates in relation to other
social program funding.
The Home and Community Care Program, for example, has a range of
indexation rates varying between 2.1 per cent and 3.85 per cent applied
annually. The Supported Accommodation Assistance Program has an indexation rate
of 2.2 per cent, while the Australian Healthcare Agreement also has varying
indexation rates. Its general component is made up of two per cent wage-cost
indexation and 2.84 per cent population growth. Seventy-five per cent of the
general component comprises 1.7 per cent utilisation growth.[67]
3.92
However FaCSIA indicated that the Commonwealth was not merely seeking to
address increased costs in the delivery of disability services in setting the
indexation rate. Consideration of the Commonwealth's indexation in relation to
CSTDA funding should also take into account additional funding initiatives made
by government. Mr Stephen Hunter of FaCSIA commented:
The government does not seek, through indexation, to cover all
cost increases that might occur in the delivery of a service. If it were to do
that there would be very few incentives to seek to contain some of the costs.
What it seeks to do through indexation is to ensure that the forward estimates
broadly reflect the price basis of the year in which the expense is to occur
and the minimal realistic costs of delivering policy outcomes. So it does not
try to compensate for actual movements in costs but rather to, in the broad,
ensure that the forward estimates reflect the price basis of the units involved...I
think when you look at the issue of indexation alongside the other additional
funds that have been put forward in the context of the CSTDA, that is a
relevant consideration. If, simply, you just compensate for all the cost
increases that might occur, governments then to an extent rob themselves of the
capacity to make specific initiatives which might go to achieve specific
outcomes.[68]
3.93
The Department of Finance and Administration has also indicated that
Wage Cost Index 2 has been used as the indexation rate for Commonwealth CSTDA funding
as the relative weighting of wage and non-wage costs best reflects the balance
between wage and non-wage costs in the services supplied under the CSTDA.[69]
3.94
However in 2002, the Social Policy Research Centre (SPRC) conducted a
study for the National Disability Administrators which examined the issues of
indexation and demand in relation to CSTDA funding. It suggested that Wage Cost
Index 2 was not suitable for CSTDA indexation as the method of calculation was
not appropriate for the disability sector:
Wage Cost Index 2 is based primarily on the Industrial Relations
Commission Safety Net Increase together with a small component based on general
price inflation. This is so the index should not include any component of wage
growth that is intended to be offset by efficiency gains. However, this implies
assumptions about productivity growth that are not in accord with generally
accepted economic principles. Economic theory suggests that wage growth in
service industries and human services in particular, will run well ahead of
productivity growth in that sector.[70]
3.95
This view was supported by the Queensland Government which commented:
Indexation models adopted by the Commonwealth Government have
been based upon the assumption that there will be efficiency dividends or
productivity saving that result in reduced labour costs or efficiencies due to
technology or telecommunications improvements. However research has found that
industries such as human services are not able to make productivity gains in
ways that are available to other industries. This is due to the fact that they
are highly labour intensive, have limited opportunities for technology-based
productivity gains, experience significant flow-on pressures for wage increases
from allied sectors and are expected to meet prescribed service delivery
standards.[71]
3.96
Dr Baker commented:
There is an assumption built into the Commonwealth indexation
formula which is just flawed. It may be appropriate for a manufacturing sector
or a mining sector, where human resources can be replaced with technology and
productivity can be achieved like that, but that is not true within the
disability sector, where social interaction is the nature of the business.
Disability support workers cannot be replaced by machines. The assumption
within the Commonwealth indexation formula that any increase that is over and
above the safety net increase can be traded off against productivity or
efficiency increases is just not true.[72]
3.97
The Committee considers that the application of the efficiency dividend is
generally inappropriate in relation to the indexation of funding for specialist
disability services given the necessarily high proportion of total budget which
must be spent on staff wages in delivering personal care. Recognising that
limited efficiencies can be gained in the sector, the efficiency dividend
effectively acts to cut the level of funding for disability services.
Recommendation 7
3.98
Given the reality that a large proportion of costs in disability
services will always be wages and salaries of care providers, the Committee
strongly recommends that the Commonwealth consider removing the efficiency
dividend from the indexation formula for funds allocated through the CSTDA.
3.99
The SPRC study recommended an indexation rate based on actual movement
in wages that reflects a more realistic level of productivity savings in the
disability sector. It proposed a wage cost index be used based on the
Australian Bureau of Statistics Wage Cost Index (ABS WCI) combined with a
general Consumer Price Indicator (CPI) inflator to cover costs not related to
wages. It noted that over recent years the ABS WCI had grown at twice the rate
of the Wage Cost 2, currently applied to Commonwealth CSTDA funding.[73]
The SPRC study also noted the need for indexation of CSTDA funding to address
on-costs for service providers such superannuation and workers compensation
insurance.
3.100
The Committee notes the annual September quarter 2006 ABS Wage Price Index
seasonally adjusted increase for all employee jobs in Australia was 3.8 per
cent.
Recommendation 8
3.101
That the Commonwealth set an indexation level in line with the actual
costs of delivering services. This rate should be applied as a minimum
indexation rate by State and Territory Governments.
Demand funding
3.102
A number of submissions argued that the current CSTDA lacks long-term
strategic planning for increasing demand for specialist disability services. In
general demand adjustments to funding seek to ensure that the relationship
between the supply of services and the demand for services remain the same. For
example to adjust funding to account for increases in the population or in
prevalence of disability in the population which would increase demand for
services.[74]
Ms Felicity Maddison of the National Carers Coalition commented:
...the whole CSTDA is crisis driven as to the rollout of support.
Because of the lack of the bulk of funding that is available, funding is
rationed and it is coming out—it is being rolled out—on the basis of crisis
intervention rather than in a well-constructed forward planning process. There
is no evidence of long-term planning for the future and you are getting a lot
of flavour-of-the-month-type initiatives coming through...[75]
3.103
In the current CSTDA demand adjustment and growth funding is dealt with
in Part 8 (8):
Commonwealth, States and Territories acknowledge demand management
requires regular annual growth in funding levels to continually improve the
level and quality of services and the efficiency of systems for specialist
disability services. The States/Territories will provide annual funding growth
at a level agreed between each State/Territory and the Commonwealth over the
life of the Agreement for services they are directly responsible for
administering under the Agreement.
3.104
The CSTDA arrangements do not require multi-year budgetary planning
based on demand growth. Some submissions proposed population-based benchmark
funding similar to that used for the funding of aged care services would be
more appropriate for funding calculations for disability services.[76]
ACROD commented:
Aged Care uses a needs-based planning framework that seeks to
achieve and maintain a national provision level of 108 residential places and
Community Aged Care Packages (CACPs) for every 1,000 of the population aged 70
years and over. While there is some debate about the formula, its aim is to
ensure that the growth in the number of aged care places is in line with growth
in the aged population and that there is a balance of services, including
services for people in rural and remote areas.
The disability sector has nothing similar to guide the provision
of residential and community care places to people with disability. We know
that only 48 of every thousand persons in the comparable population (broadly,
people under 65 years with a severe or profound core activity restriction)
receive a CSTDA-funded disability accommodation support service.[77]
3.105
The Committee notes that the Disability Policy and Research Working
Group (formerly the National Disability Administrators) is conducting research
into Demand Management due for completion in June 2007.
Recommendation 9
3.106
That the next CSTDA incorporate appropriate benchmarks and annual
targets in relation to identified unmet need for specialist disability
services.
Growth Funding
3.107
Several State and Territory submissions noted that their CSTDA funding
contributions for specialist disability services were growing at a faster rate
than those from the Commonwealth. The Queensland Government noted that:
The Queensland Government has made significant additional
investments in disability services in recent years representing a commitment at
the State level to respond to needs of people with a disability. A
commensurable effort by the Commonwealth Government has not been realised.[78]
3.108
However, a larger proportion of new Commonwealth funding has gone into
the disability employment services which it directly administers. Over the
course of the current agreement annual Commonwealth funding of disability employment
services has increased from $303 million to $486 million while funding to the
States and Territories for special disability services has increased form $521
million to $616 million.[79]
3.109
ACROD suggested the following reasons for this trend:
This reflects the Commonwealth's view that:
- implementing
the ambitious raft of disability employment service reforms required additional
spending on those services;
- States are
insufficiently accountable for the expenditure of funds they receive from the
Commonwealth;
- State-administered
services are principally the responsibility of the States; and
- higher-than-expected
GST revenue should reduce the States' call on Commonwealth specific-purpose
transfers.[80]
3.110
The State and Territory Governments also expressed concern that increases
in the level of CSTDA funding were not being reflected in requirements set in
the Bilateral Agreements.
The Australian Government applies a "matched funding"
requirement as a part of most bilateral agreements, but there is no structure
in place to acknowledge additional funding efforts made by the States and Territories.
A further shortcoming of the Commonwealth’s introduction (as
part of a regime of input controls) of a ‘matched commitment’ at the time of
signing an agreement is that this does not recognise previous efforts of States
and Territories. This can create a disincentive to states in making additional
efforts in growth funding during an agreement as this additional effort becomes
effectively locked-in to areas that may not be reflective of need in the State
or Territory.[81]
Recommendation 10
3.111
That the next CSTDA ensure 'matched funding' commitments do not provide
a disincentive for governments to provide additional funding for specialist
disability services.
Equity of funding distribution
3.112
A number of State and Territory Governments argued the Commonwealth
funding for specialist disability services was not distributed equally amongst
the jurisdictions in relation to their proportion of people with disabilities.[82]
For example the Victorian Government commented:
Victoria receives less than its equitable share of Commonwealth funding,
which results in an estimated shortfall of some $40 million over the life of
the current CSTDA.[83]
3.113
The Western Australian Government provided a graph, reproduced as Table 3.3,
to illustrate what it suggested was a lack of equity in the distribution of
Commonwealth CSTDA funding in relation to potential population.[84]
The Australian Institute of Health and Welfare (AIHW) estimates 'potential
population' in each jurisdiction to broadly indicate the number of people with
the potential to require specialist disability services at some time. The potential
population for each jurisdiction is calculated from population disability
survey estimates and is constructed for comparative purposes and to provide indications
of relative need.[85]
Table 3.3:
Funding equity in relation to potential population
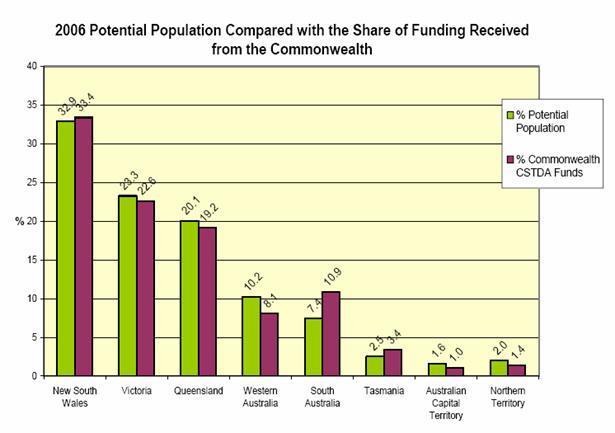
Source: Western Australian Government, Submission 3a,
p.23.
3.114
The current distribution of Commonwealth funding is based on historical
arrangements present during the first CSDA. During the negotiations for the
current CSTDA parties considered solutions for a more equitable distribution of
Commonwealth funding. The Western Australian Government commented:
...Ministers considered options for an accelerated equity formula.
The Commonwealth Minister took the position that they would allocate their
growth funds on whatever equity funding formula agreed to by States/Territories.
Ultimately, agreement was not reached, and the overall distribution of funding
to the States and Territories has remained inequitable. The Commonwealth was
not prepared to provide additional funding to address the equity issue.[86]
3.115
The Northern Territory Government also identified funding equity issues
in relation to other factors, such as the costs of service delivery:
29% of the Northern Territory population are
Aboriginal...Australian Institute of Health of Welfare (AIHW) estimates indicate
the Aboriginal people are 2.4 times as likely to have a severe or profound
disability as non-Indigenous Australians...The Northern Territory also has the
largest population of people living in extremely remote settings...The highly
dispersed nature of the population, particularly for those with the greatest
need, substantially increases the cost of service delivery in the Northern
Territory.[87]
Possible solutions
3.116
The Western Australian Government argued that certain principles should
be adhered to in any solution to address inequity in the distribution of
Commonwealth CSTDA funding:
The core principle underlying a move towards equity must be to
recognise that this is funding used to provide services to individuals and that
no Australian with a disability should be disadvantaged on the sole basis of the
jurisdiction they reside in.
The second principle is that no state or territory should
receive a lower proportion of funds than is appropriate for their population.
In the case of South Australia and Tasmania this may mean that the level of
funding they receive may be the level necessary and thus should not be reduced.[88]
These principles suggest a solution of the 'making the pie
bigger', by providing an increased proportion new funding to States and
Territories currently receiving less than the proportion indicated by their
potential population. However there were also concerns raised about this
approach. The Tasmanian Government noted there was a risk that jurisdictions
may 'increase the number of clients that they provide a service for by simply
allowing people into the system who have very low levels of support'.[89]
We are not against anyone getting their fair share, but you can
build that into future growth components and then simply try to equalise it
over the next five years.[90]
3.117
An argument also discussed was that providing additional Commonwealth
funding to States and Territories which are providing inadequate levels of
disability services or which have historically provided inadequate funding could
be perceived as rewarding underperformance. An alternative model raised also discussed
which would match additional funding for disability services by State and
Territory governments over a base funding level. This would reward
jurisdictions which provided additional funds for specialist disability
services. For example Dr Baker of ACROD commented:
Ultimately I would not want to see any service user in any state
disadvantaged by that process, but at present I think the situation is
inequitable... it reinforces low performance by state governments because the
Commonwealth is providing proportionately more funding to states where state
government funding is low. I think the Commonwealth should be doing the opposite.
It should be, if anything, rewarding high-performing or high-funding states.[91]
3.118
The Committee's view is that there should be a balance in the next CSTDA
between providing a base level of funding for specialist disability services
and allowing governments a measure of flexibility to make agreements to provide
additional funding for priority areas. The Committee is sympathetic to the
principles outlined by the Western Australian Government as applied to based
funding, however there should also be opportunities for governments to
establish incentives for other jurisdictions to provide additional funding for
specialist disability services, for example by seeking matched funding for
specific initiatives of that government. Matched funding agreements have been
an efficient mechanism to provide incentive for governments to commit additional
funding to services.
Recommendation 11
3.119
That the Commonwealth have responsibility in the lead up to the next
CSTDA for developing an equitable distribution formula of Commonwealth base funding
which takes into account differences between States and Territories in terms of
potential population and costs of service delivery.
Recommendation 12
3.120
That, in addition to that funding "platform", arrangements be
put in place to allow specific services or programs to be initiated on the
basis of cost-sharing or matched funding between the Commonwealth and
particular State and Territory governments which commit additional funding for
specialist disability services.
Performance monitoring and reporting
3.121
There are three main performance reporting arrangements under the CSTDA:
- the CSTDA National Minimum Data Set (NMDS) and associated data
collection arrangements;
- annual reporting between governments on funding spent and
progress and achievements in implementing strategies to address national policy
priorities; and
- the CSTDA Annual Public Report commissioned by the National
Disability Administrators listing the progress and achievements in implementing
national policy priorities.[92]
3.122
Schedule A3 of the CSTDA provides for the form of performance reporting
against the major areas of disability services being provided – accommodation
support, community support, community access, respite, open employment and
supported employment – see Table 3.4 for an example of the performance data
required. The performance indicators are largely similar for each area of
disability services and consist of efficiency measures and equity measures.
Table 3.4: Example of CSTDA performance data requirements
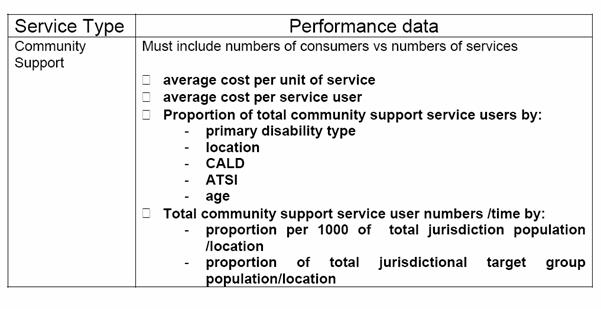
Source:
Commonwealth State Territory Disability Agreement 2002-2007, Schedule A3.
3.123
In 2005 the Australian National Audit Office (ANAO) undertook a
performance audit of the (then) Department of Family and Community Services'
role in the CSTDA. The audit report noted that the objective of the CSTDA to
'enhance the quality of life experience by people with disabilities through
assisting them to live as valued and participating members of the community'
was not reflected in the performance management framework.
...the performance information framework contained in the CSTDA
includes no indicators of the quality of life of people with disabilities,
their participation in the community, their value in the community, or any
related parameters, despite the objective directly aimed at enhancing quality
of life. Therefore, the performance information framework contained in the
Multilateral CSTDA does not require the collection of data that can clearly
indicate whether, or to what extent, the CSTDA is meeting its
objective.[93]
3.124
This criticism was repeated in a number of submissions the Committee
received. For example, the Australian Federation of Disability Organisations
commented on the limitations of the current performance management model.
If you think about the way that the CSTDA is currently assessed,
it is a real counting exercise: how many people have you seen? It is supposed
to assess the objective of the CSTDA, which is: have we made the lives of
people better? There is nothing about counting how many people who have access
to services that tells you anything about whether people’s lives are better.[94]
3.125
The ANAO audit made five recommendations focusing on improvements in
performance measures and reporting requirements all of which were accepted by FaCSIA.
However FaCSIA has stated that while there has been progress in implementing
the ANAO's recommendations 'because states and territories are responsible for
the delivery of specialist disability services other then employment,
improvements in performance reporting will require input and agreement from
state and territory governments.' FaCSIA have indicated that these issues will
be part of the negotiations for next agreement.[95]
The ANAO Report noted long-standing problems in reconciling State and Territory
commitments under the CSTDA with State and Territory Budget appropriations and
reporting in annual reports.[96]
The challenges in relation to obtaining performance data comparable between the
jurisdictions are well recognised.[97]
Input controls
3.126
State and Territory Governments raised concerns that the structure of
the CSTDA was too focused on input controls reducing the flexibility of
governments and service providers to address local issues.[98]
3.127
The current CSTDA defines the specialist disability services funded
under the agreement into a number of categories, such as community support
services. Services with a specialist clinical focus and non-specialist services
are outside of the agreement.[99]
Funds made available may only be utilised for the provision of specialist
disability services covered under the Agreement or a Bilateral Agreement.[100]
However other specialist disability services may also be included under the
agreement where the Commonwealth and States/Territories agree.
3.128
The Queensland Government commented:
The input control process requires the matching new funds to
programs, resulting in a service system that is rigid and requires people to
fit the programs instead of providing services that are needs based...Given the
five-year term of the CSTDA, flexibility is needed to promote service
improvement and innovation in relation to local priorities, and to promote the
capacity to develop responses to emerging issues. The CSTDA was developed in
such a way as to "rope" all funds into expenditure on six service
types only. This is proving limiting to Queensland's ability to be more
responsive and innovative.[101]
The burden of accountability
3.129
The Western Australian Government noted that performance monitoring and
accountability regimes also need to appropriately balance the relative size of
both parties' contributions.
An acceptance of shared responsibilities by the States and
Territories should not be taken by the Australian Government as an invitation
to exercise disproportionate control over policy direction in the disability
services sector. As this submission has shown, the proportion of the Australian
Government contribution to the sector, particularly in Western Australia, has
shrunk. Despite this, the Australian Government has sought ever higher levels
of control over both administration and policy of the State’s and Territory’s
disability services.[102]
3.130
The NSW Government highlighted that while the current CSTDA does not
include incentives and targets, it does contain potential penalties for the
State and Territory Governments whereby the Commonwealth Government can
withhold payments if reporting requirements are not met.[103]
The NSW Government commented:
The move to include incentives, sanctions and targets in SPP
Agreements needs to recognise the recommendations by the Australian
Parliament’s Joint Committee of Public Accounts and Audit that financial
accountability requirements for SPPs should be as streamlined as possible, to
improve administrative efficiency and to avoid duplication between Commonwealth
and State and Territory Auditors–General.[104]
Outcomes and quality based
performance framework
3.131
The current CSTDA NMDS does not include measure or indicators of
individual outcomes or quality of life. The Committee noted broad support of an
increased role of outcomes and quality based performance measures in the next
CSTDA.[105]
These changes appear to be a priority for governments going into the
negotiations for the next agreement. FaCSIA noted that:
...despite advances in transparency and accountability under the
current CSTDA, further work is needed to augment the current input controls and
output reportings with an outcomes reporting framework. An outcome reporting
framework will enable us to look at performance in a meaningful way and assess
what outcomes are being achieved for people with a disability.[106]
3.132
There appear to be challenges in developing a realistic outcome and
quality framework which gathers meaningful performance data and does not impose
administrative burdens on service providers. [107]
Nonetheless ACROD commented:
Quality monitoring has focused more on processes and systems
than on quality-of-life outcomes for service users. This should change...While
measuring quality of life outcomes for service users poses challenges (and
invites scepticism from some commentators), there are several existing designs
which claim to do it well. Measurement systems should include subjective and
objective dimensions, be administratively simple for governments and service
providers and closely involve service users[108]
3.133
AIHW noted the methods for collecting data on measures or indicators of
individual outcomes and quality of life were the subject of extensive work during
the redevelopment of the CSTDA NMDS in 1999-2000. A proposed participation
module was designed to collate information collected from service providers and
users into a common framework for national comparison. The AIHW commented:
Improved information about outcomes for service users would
inform the objectives of the CSTDA itself. For example, it would be possible to
explore the extent to which CSTDA service users participate in a broad range of
life areas such as recreation, communication with family and friends,
employment or education and how they (and their carers and advocates) rate
their satisfaction with this level of participation.[109]
Recommendation 13
3.134
That realistic outcomes based performance reporting requirements be
added to the CSTDA.
Recommendation 14
3.135
That the Commonwealth take the lead in developing consistent cross-jurisdictional
performance monitoring and reporting of specialist disability services to
promote greater coordination and accountability between jurisdictions.
Navigation: Previous Page | Contents | Next Page