Chapter 1 - Introduction
Terms of reference
1.1
On 10 February
2005 the Senate, on the motion of Senator the Hon
Peter Cook,
referred the following matters to the Committee for inquiry and report by 23 June 2005:
- the delivery of services and options for treatment for
persons diagnosed with cancer, with particular reference to:
- the efficacy of a multi-disciplinary approach to cancer
treatment,
- the role and desirability of a case manager/case
co-ordinator to assist patients and/or their primary care givers,
- differing
models and best practice for addressing psycho/social factors in patient care,
- differing
models and best practice in delivering services and treatment options to
regional Australia and Indigenous Australians, and
- current barriers to the implementation of best practice
in the above fields; and
- how less conventional and complementary cancer
treatments can be assessed and judged, with particular reference to:
- the extent to which less conventional and complementary
treatments are researched, or are supported by research,
- the efficacy of common but less conventional approaches
either as primary treatments or as adjuvant/complementary therapies, and
- the
legitimate role of the government in the field of less conventional cancer
treatment.
Conduct of the Inquiry
1.2
The inquiry was advertised in The Australian and through the Internet. The Committee wrote to
interested individuals and groups inviting submissions. The Committee received 105
public submissions and 8 confidential submissions from a range of organisations,
individuals and Commonwealth and State departments. Many of the submissions
were from individuals describing their personal cancer journey of being
diagnosed with cancer and the impact it has had on their lives and that of
their families. A list of individuals and organisations who made a public
submission or provided other information that was authorised for publication by
the Committee is at Appendix 1.
1.3
The Committee held public hearings in Perth,
Melbourne, Sydney
and Canberra. In organising its
hearing program, the Committee endeavoured to hear from the major organisations
which made submissions to the inquiry, including all the groups who represent
or support individuals with cancer. A number of these individuals also gave
personal testimonies about living with cancer. The Committee also spoke via
teleconference with individuals from acknowledged best practice hospitals and organisations
in the USA and UK.
A list of witnesses who gave evidence at the public hearings is at Appendix 2.
1.4
Some important issues and questions arose from the
submissions and evidence received by the Committee. Professor
D'Arcy Holman,
Head, School of Population
Health at the University
of Western Australia, was
commissioned to provide a response to these issues. The advice and Briefing
Paper provided by Professor Holman
(Holman report) proved a valuable contribution to the Committee's inquiry.[1]
Background to Inquiry - Cancer in Australia
What is cancer?
1.5
'Cancer' is a broadly used expression. The Holman
report describes cancer as not a single disease but rather it is a diverse
group of diseases characterised by the proliferation and spread of abnormal
cells, which cannot be regulated by normal cellular mechanisms and thus grow in
an uncontrolled manner. These abnormal cells may then invade and destroy
surrounding tissue and spread (metastasise) to distant parts of the body via
the circulatory or lymphatic system. Cancer can develop from most types of
cells, with each cancer having its own pattern of behaviour and metastasis.[2] This description reflects that of the National Service Improvement Framework for
Cancer which notes that 'Cancer is a chronic and complex set of diseases
with different tumour sites. For some cancers, there is considerable knowledge
about their causes and optimal treatment. This varies for other cancers.'[3] These views are succinctly drawn
together by the Australian Institute of Health and Welfare (AIHW) which defines
cancer as:
...a diverse group of diseases in which some of the body's cells
become defective, begin to multiply out of control, can invade and damage the
tissue around them, and may also spread (metastasise) to other parts of the
body to cause further damage.[4]
The good news
1.6
Internationally, Australia
compares well with other developed countries in terms of its cancer survival
rates. The AIHW report Cancer in
Australia 2001, shows that Australia's
cancer mortality rate is low when compared with other developed countries. In
addition, over the past ten years, total cancer death rates declined by an
annual average of 1.9 per year.[5] Further
good news is that five-year survival rates for the most common cancers
affecting men (prostate) and women (breast) are now more than 80 per cent.[6] This indicates that cancer survival in Australia
is relatively very good and suggests our health system is performing
comparatively well in the areas of early detection and treatment of cancer.[7] Whilst this is welcome news it is no
excuse for complacency and one of the motivations of this report is to discover
if we can do better. Based on the international evidence provided, it is clear
that cancer treatment is dynamic and evolving with new aspects of medicine
continuing to provide new opportunities.
The increasing burden of cancer in
Australia
1.7
Given these achievements in decreased mortality and
increased survival, why was an inquiry into the delivery of services and
treatment options for persons diagnosed with cancer in Australia
needed? Firstly, cancer currently places a huge burden on the community and
this is set to rise in the coming years. Despite advances, cancer remains a
leading cause of death in Australia
accounting for 28 per cent of all deaths in 2003.[8] Cancer currently accounts for 31 per
cent of male deaths and 26 per cent of female deaths. In 2005 we can expect
that there will be around 36 000 deaths in Australia
due to cancer. Cancer also accounts for an estimated 257 458 potential
years of life lost to the community each year as a result of people dying of
cancer before the age of 75.[9]
1.8
In addition to the existing burden, the cancer
incidence rate has been increasing over the past 10 years. Recent trends in
cancer data produced by the AIHW indicate that the annual number of new cancer
cases diagnosed rose by 36 per cent between 1991 and 2001, compared with
population growth of 12.3 per cent. The AIHW noted that there is likely to be
an increase of similar magnitude over the next 10 years. Currently, one in
three men and one in four women will be diagnosed with cancer before the age of
75 years (see Figure 1.1).[10] In fact, the
sentiment that 'every Australian is likely to be affected by cancer, either
through personal experience or the diagnosis of a loved one'[11] was typical of that expressed in many
submissions.
Figure 1.1: Risk of being diagnosed with cancer in the
next 10 years
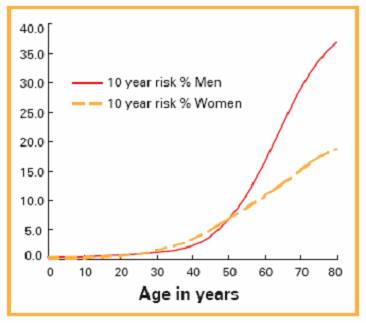
Source:
Cancer in Australia: An update for GPs, Australian Family Physician, v.34, January/February 2005, p.43.
1.9
The increase in the incidence of cancer is partly
explained by Australia's
ageing population as cancer incidence is lowest in late childhood and increases
with age. The most rapidly increasing age group in the population is aged 65
and over and the average age of first diagnosis for cancer is 66 years for
males and 64 years in females.[12]
1.10
Along with increased incidence of cancer we can also
expect detection, treatment and survival rates for cancer to continue to
improve, meaning that there will be more people living with cancer for longer
in the future but with relatively fewer taxpayers to support them. The
Australian Bureau of Statistics notes that 'currently more than 267 000
Australians are living with cancer, many with persistent and incurable forms'.[13] Professor
Holman noted that cancer patients living
longer 'is the single most important reason why so many of us are now in
contact with a relative or friend who is living with cancer'. He provided data
from the WA Data Linkage System which shows that 'in WA the prevalence of
active cancer (ie, people 'living with cancer' that requires ongoing clinical
management) increased from 5.1/1 000 to 7.4/1 000'.[14]
1.11
The growing number of people being diagnosed with
cancer and living with cancer for longer will inevitably increase the demand
for cancer resources and services. AIHW data shows that:
- there was a 31 per cent increase in
inflation-adjusted cancer expenditure from 1993-94 to 2000-01;[15]
- Average cancer expenditure per person was $146
for males and $135 for females in 2000-01. This was much higher in the older
age groups. In the 65-74 year age group, average cancer expenditure per person
was $641 for males and $389 for females while in the 75 years and over age
groups, the averages were $984 for males and $480 for females[16]; and
- New cases diagnosed in 2001 showed an increase
of 22 000 on 1991 figures.[17]
1.12
These trends will place added pressure on the national
health budget and will pose ongoing challenges to the delivery of optimal
cancer care in Australia.
The need to ensure the best use of
cancer resources
1.13
Witnesses from the Australian and State governments informed
the Committee about the cancer initiatives being undertaken to improve
treatment and services. The Committee was concerned about the potential for
uncoordinated systems to emerge and how sharing information on the development
of initiatives between jurisdictions would occur. The Committee considers that
Cancer Australia should have a role to ensure the development of well coordinated
cancer initiatives in the various jurisdictions and provide a forum for
jurisdictions to report progress on their respective initiatives to facilitate
the sharing of information.
1.14
During the course of the inquiry the Committee was
advised that there were more than 100 government and non-government organisations
that contribute to cancer policy or are involved in cancer treatment or support
around Australia
(see Appendix 3). The Committee recognises the valuable role played by these
services, however, given the increasing burden that cancer will place on the
community in the coming years the Committee believes that there is a need to
ensure that cancer resources are well organised, used efficiently and
effectively and that any potential for duplication and overlap is addressed.
1.15
The large number of organisations involved in cancer
policy or support was also raised by some witnesses. Professor
Coates described the functions of various
bodies to the Committee but added:
I do have a PowerPoint presentation which I call 'the alphabet
soup', which goes through some of these myriad acronyms. It contains a diagram,
which looks rather like one that was put up to an ALP conference, of the
spaghetti connections between various bodies in the cancer universe.[18]
1.16
The Committee also noted the large numbers of tumour
specific support groups which, although filling a void for information and
support, may benefit from the promulgation of best practice models. Dr
Hassed spoke to the Committee about evidence
that not all cancer support groups seem to be as effective as every other. He
noted that effective cancer support programs significantly improve the mental,
emotional and social health of participants and are associated with
significantly longer survival.[19]
1.17
The potential for improved organisation of support
services was acknowledged by Mr Davies,
Department of Health and Ageing, who told the Committee that the Department has
commissioned The Cancer Council Australia to undertake a review of the cancer
support networks and also to examine overseas experience. The objective would
be to identify best practice models and promulgate these to be shared among the
organisations.[20]
1.18
The necessity for cost-efficient delivery of cancer
care services was reinforced by Professor
Holman:
...the increasing prevalence of active cancer has profound
implications for the planning, provisions and financing of health services. An
increasing proportion of health care resources will inevitably need to be
allocated to cancer care, and more cost-efficient ways of delivering that care
will become imperative.[21]
Increasing patient focus and empowerment
1.19
People being diagnosed with cancer are demanding more
information about their cancer, their treatment options and the role they can
perform. As Dr Gawler
noted: 'There is huge public interest in how much an individual can affect the
outcome of their illness'.[22] Cancer
patients are becoming more active participants in their treatment and there are
growing demands for:
- Patient-focussed, coordinated multidisciplinary
care to address the current cancer care lottery and provide best practice care
along the care continuum;
- Support throughout the cancer journey;
- Access to evidence-based quality care, including
clinical trials, and a willingness by medical practitioners to discuss
treatment options, including complementary therapies;
- Greater and easier access to understandable and
authoritative information, including complementary therapies, to assist
patients with making informed treatment decisions and to enable dialogue with
health professionals; and
- Equitable access to care for rural and
Indigenous Australians.
Patient-focussed,
coordinated multidisciplinary care to address the current cancer care lottery
and provide best practice care along the care continuum
1.20
This issue has been precisely described by Lance
Armstrong, one of the world's most
recognised athletes who challenged his cancer head-on:
From that moment on, my treatment became a medical
collaboration. Previously, I thought of medicine as something practiced by
individual doctors on individual patients. The doctor was all-knowing and
all-powerful, the patient was helpless. But it was beginning to dawn on me that
there was nothing wrong with seeking a cure from a combination of people and
sources, and that the patient was as important as the doctor.[23]
1.21
Cancer patients spoke to the Committee about the
'cancer lottery' starting at the point of diagnosis where they found the referral
process ad hoc, with many finding specialists through serendipitous connections
and word of mouth. Patients wanted more information to be able to choose a
specialist they felt comfortable with.
One of the critical issues in terms of the health system in Australia
is that it is absolutely fragmented – the left hand does not know what the
right hand is doing.[24]
1.22
Witnesses also reported their care had been fragmented
and disorganised and individual support needs had not been met. The National
Breast Cancer Centre noted:
In Australia,
screening, diagnosis, treatment and supportive care for patients with cancer
are typically provided by different services, often with little coordination,
leading to fragmented care, sub-optimal management and high health care costs.[25]
1.23
Cancer patients wanted greater coordination of care
along the care continuum through a multidisciplinary approach and combined with
better support mechanisms. Cancer patients told the Committee how they
experienced feeling 'lost' in the current cancer treatment system which led to
additional personal distress and many reported stumbling over information which
should have been provided to them or readily available in a range of formats.
Support throughout the
cancer journey
1.24
The impact of being diagnosed with and living with
cancer was graphically described by many witnesses:
Cancer affects every aspect of a person's being if they are
touched by it. It affects the patient, friends and health professionals in
their physical life, their emotional life, their mental life and their
spiritual life.[26]
You are in a constant spin. There is
not one thing in your life that remains the same. It is a complete up-ending. I
had to deal with psychological problems, practical problems.[27]
1.25
The Committee heard that people diagnosed with cancer
want recognition that cancer is not just a physical disease but has an
emotional and practical impact on them, their family and carers and that referral
to support services should be standard practice from the beginning of their
cancer journey. This impact on life was vividly described by one cancer
patient:
A diagnosis of cancer brings with it so many other practical
problems and issues. Life on the home front had to go on. My marriage imploded,
my children struggled to cope with the diagnosis. Coping with this whilst
undergoing chemotherapy was a nightmare, but regular psychotherapy helped me to
keep my head above water. Then there were the medical bills, we have top cover
health insurance with Medibank but the gaps that I had to pay left, right and
centre (especially for the psychotherapy as I soon used up my annual allowance)
meant I could not pay my other bills.[28]
1.26
However, cancer patients told the Committee that access
to support in many cases was not automatic, most stumbled across support groups
and government assistance and most did not obtain the support they needed. One
notable exception was in the case of breast cancer where the amount of
information and support services was recognised and praised. Patients also
wanted assistance to navigate their way through the health and hospital systems
as for some it was their first time dealing with these areas. This aspect was
described by the following witness:
One day John was fit – he was
riding his bicycle and running – and the next day he was in hospital with a
brain tumour. I had never been in a hospital. If someone had given me a
brochure saying what a registrar is and what an intern is, I would have known.
I would have had a much better idea of how the hospital system worked. It would
have been brilliant. I just needed a map of the hospital on the very first day.[29]
Access to
evidence-based quality care, including clinical trials, and a willingness by
medical practitioners to discuss treatment options, including complementary
therapies
1.27
Witnesses were unanimous in their call for treatment to
be patient instead of disease focussed. Evidence indicated that cancer patients
were voting with their feet to find practitioners who were willing to take the
time to discuss treatment options, including the use of complementary therapies,
so that they could make informed treatment choices. The following illustrates
this view:
Our experiences with the 'system' were characterised by...a
complete unwillingness to discuss any potential action other than the medical
treatment being provided by the specialists...[and] a failure to provide any
advice that alternative sources of information existed – beyond the very
limited, and medically oriented handouts from the hospital – and that this
information might not only enhance the treatment, but make it more palatable.[30]
Parents of a cancer
patient described their experience:
We were not given options in respect of treatments. Medical
conventions knew best. We were patronised at every point. No choices. We
accepted that the radiotherapy and chemotherapy as presented was the only way
to go. Our daughter was very keen to do something for herself, although told
there was nothing that she could do.[31]
1.28
The Committee was advised that in comparison to
overseas cancer centres such as Memorial Sloan-Kettering in New
York, the number of cancer patients enrolled in clinical
trials in Australia
is very low and clinical audits are rare.[32]
These issues are discussed further in chapter 5.
Greater and easier
access to understandable and authoritative information, including complementary
therapies, to assist patients with making informed treatment decisions and to
enable dialogue with health professionals
1.29
Australians are becoming better informed about health
issues thanks to greater access to medical and health information on the
Internet and national preventative health campaigns. There is a growing trend for
people wanting to take responsibility for their health and well-being. As a
result, when a disease like cancer is diagnosed, many patients wish to be
active participants in their treatment plans to feel a greater degree of
influence and control. Cancer support organisations in Australia
and overseas support and promote the view that knowledge is power for cancer
patients, as exemplified by the comments of Mr
Ulman from the Lance Armstrong Foundation:
We believe that in your battle with cancer knowledge and
attitude is everything. We really strive to not only inspire but also empower
those people with cancer so that they have the tools and information they need
to live with a very high quality of life.[33]
1.30
Cancer patients are requesting more information in
order to better understand treatment options and to be an active participant in
decision making. Patients wish to engage in a dialogue with their medical
practitioners and are seeking the information to do so. Witnesses told the
Committee that they struggled to find authoritative information and more often
than not just stumbled across information on the Internet and through talking
to people.
I had to constantly ask for information, and I still found out
so much by accident and from other people making a comment.[34]
1.31
This call for greater information has resulted in
publications such as the Directory of
Breast Cancer Treatment and Services for NSW Women produced by the Breast
Cancer Action Group NSW in association with the NSW Breast Cancer Institute.[35] However, the call for more information
from cancer patients is relevant for all stages of the cancer journey.
Equitable access to
care for rural and Indigenous Australians
1.32
The Committee heard evidence of inequalities in the
health system for rural and Indigenous Australians. Mr
Gregory from the National Rural Health
Alliance referred to data that people in country areas who are diagnosed with
cancer are 35 per cent more likely to die within five years than cancer
sufferers in the city. Mr Gregory also provided alarming statistics for
Indigenous Australians where evidence from the Northern Territory and South
Australia shows that Aboriginal and Torres Strait Islanders with cancer are
twice as likely to die from the disease as non-Indigenous people with the
disease.[36]
The Call
for Reform of Cancer Care in Australia
Cancer services in Australia
are in what are probably the early stages of a major paradigm shift. I think
this shift in the approach to treating cancer has been fuelled primarily by the
interest of the public and by their interest in the better outcomes that have been
achieved in recent years. It is supported by a great deal of research...it is
also being driven by progressive universities providing more graduate training
and postgraduate training...and it is starting to show up in progressive
hospitals.[37]
1.33
The consumer needs outlined above have been recognised
and a number of recent reviews and publications by consumers, practitioners and
cancer care providers have recommended the reform of cancer care in Australia.
They acknowledge that some improvements are occurring but suggest that cancer
care is now at a crossroads and that the next step to improve cancer treatment
and services in Australia is the development of a national, evidence-driven
approach, involving greater coordination of the cancer patient's journey and
recognising the need for a consumer-focussed approach to cancer care.
1.34
These publications include: Optimising Cancer Care in Australia,
produced by the Clinical Oncological Society of Australia, The Cancer Council
Australia and the National Cancer Control Initiative. The key issue highlighted
in the report is the failure of the health system to provide integrated cancer
care.[38] Other reports, Priorities for Action in Cancer Control
2001-2003 and the National Cancer
Prevention Policy 2004-06, have identified priorities for new developments
in cancer control and made recommendations on how Australia
can enhance its achievements in cancer prevention. National Breast Cancer
Centre publications, the Report of the
Radiation Oncology Inquiry, A Vision for Radiotherapy 2002 (the Baume Inquiry)
as well as Cancer Council Reports and consumer forums have also called for
reforms to the funding, operation and integration of cancer services.
1.35
Key aspects of the recommendations in these reports are
that cancer care should focus on the patient not just the disease and that
emotional and practical support should be included as standard components of
care. They highlight the differences in the public and private systems and also
identify inequalities in the system where cancer outcomes and services for
regional and rural patients and particularly Aboriginal and Torres Strait
Islanders are far from optimal and must be improved.
Conclusion
1.36
Australia
can feel justifiably proud of its internationally recognised achievements in
the areas of decreased mortality and increased survival for people with cancer.
However, the increasing numbers of people being diagnosed with cancer and
living longer with cancer will present further challenges to the delivery of
optimal cancer care services in Australia. The increasing number of people
being diagnosed with cancer will mean that there will be a need to ensure that
resources for cancer treatment and support are organised efficiently and are
directed to areas of most need to improve outcomes.
1.37
These future consumer needs are being recognised by
cancer organisations, practitioners and care providers. Recent reports have
called for reform of cancer care in Australia
to develop a national, evidence-driven approach, involving greater coordination
of the cancer patient's journey and recognising the need for a
consumer-focussed approach to cancer care.
1.38
Based on the submissions and evidence presented during
the inquiry the Committee was pleased to note that the areas of consumer need
have been recognised by the Federal and most State and Territory Governments.
Early steps are being taken to address the calls for reform with a focus on
building national service frameworks at the Commonwealth level and
implementation strategies at the State and Territory level, though some
jurisdictions are more advanced than others. The different role and responsibilities
of the Commonwealth and the States and Territories and the strategic framework
that has been developed for the delivery of cancer treatment and services are
discussed in chapter 2.
1.39
However, despite some achievements and advances in
treatment, there remain inequalities and serious gaps in the system and not all
Australians have access to best practice cancer care. This is true even in some
outer metropolitan areas but particularly for rural and Indigenous Australians.
Achieving improved equality in cancer treatment and services for rural and
Indigenous Australians is a key challenge for the health system and is
discussed in chapter 3.
1.40
The gaps in the system include lack of data relating to
the incidence and treatment of Indigenous Australians; a poor record of
clinical audit, especially in the private sector, including poorly organised
hospital based cancer registries (in both public and private settings); poor
access to psychosocial support and systemic rejection by conventional health
professionals of complementary therapies or integrative medicine.
1.41
People diagnosed with cancer are becoming more active
participants in their cancer treatment and are demanding greater coordination
of care through multidisciplinary teams, access to authoritative information to
assist them in making treatment decisions, assistance to navigate their way
through the health care system and more emotional and practical support for
them and their families and carers. These issues are discussed in more detail in
chapter 3.
1.42
The Committee also heard evidence from hospitals,
organisations and support groups who are challenging themselves to meet the
needs of cancer patients using more innovative models of care, sometimes
despite the health system surrounding them. These successful models, as well as
the barriers to their further implementation, are also discussed in chapter 3.
1.43
The trend towards taking more responsibility for one's
health is also evident in the increased use of complementary medicines and
therapies. Chapter 4 discusses the issues of efficacy and safety and moving
towards integrating the best of mainstream treatments with evidence-based
complementary therapies. Integrative medicine and the use of complementary
therapies as practiced overseas at leading cancer institutions and in Australia
are also discussed in chapter 4.
1.44
The Committee acknowledges that improving cancer
outcomes is a multifactorial field that extends far beyond the scope of this
inquiry. While the Committee's investigations were necessarily focussed by the
terms of reference, other specific issues relating to cancer treatment and care
including early detection through screening, the special needs of adolescents, research
and clinical trials, data collection and palliative care were also raised
during the inquiry. These issues are considered in chapter 5.
1.45
The important aspects of cancer prevention or risk
reduction, including ongoing public health programs addressing issues such as
tobacco control, skin cancer and diet, were not part of this Inquiry but recognised
by the Committee as highly relevant to Australia's
health system.
Acknowledgments
1.46
The Committee is grateful for the many submissions
received from institutions, professional associations, government and
non-government organisations, support groups and particularly individuals. The
patients, families and carers provided the Inquiry with extremely valuable
information in submissions and at the hearings which enabled the Committee to
better understand a patient's cancer journey and where improvements could be
made.
1.47
The Committee recognised that cancer treatment and care
is an area where there is enormous goodwill, outstanding dedication and where
everyone involved is working towards the same goal to improve the cancer
journey, eliminate the cancer lottery and achieve the best possible outcomes
for cancer patients.
1.48
The Committee acknowledges the work already undertaken
in the government and non-government sectors to develop strategic direction and
a national framework for cancer care in Australia.
The significant work and consultation undertaken to produce documents such as Optimising Cancer Care and the National Service Improvement Framework for
Cancer has meant that the existing cancer care system has been the subject
of recent review and that many areas for improvement have been identified and
remedial action recommended. It is timely that these reports and plans for
action be built upon by the Committee's report.
1.49
The timeframe for the Committee to inquire and report upon
this very important subject was especially tight and the Committee acknowledges
the assistance received from many individuals and organisations, but
particularly from Mr Clive
Deverall. The Committee
also expresses its thanks to Professor D'Arcy
Holman and Rachael
Moorin, School
of Population Health at the University
of Western Australia, for their
detailed response to issues and Briefing Paper that provided a valuable
contribution to the Committee's deliberations.
Barb's story -
Informing choice in her cancer journey
In the last days of December 1988, at the age
of 30, I was taken to hospital with a very painful and bloated stomach and a
fever that my GP could not get under control. The day after some exploratory
surgery I was told by a young intern doing his ward rounds that I would need
further treatment - chemotherapy or radiotherapy. That was the first
information I was given post surgery. The doctor delivered the news, pulled the
curtain back around my bed and disappeared on his rounds again. I was in shock.
At no stage during my stay at the hospital or, indeed, afterwards was I offered
any kind of counselling or given any acknowledgment that I might be upset or
need help. I was diagnosed with adenocarcinoma of the peritoneal cavity...My
surgeon and, subsequently, the initial oncologist I consulted told me that I
had better do everything I wanted to do before next Christmas and that there
was no treatment to be had that would help me. Wanting another opinion, I
consulted another oncologist a few weeks later. This one told me that probably
nothing would work but, if I liked, he could try some extremely aggressive
chemotherapy that would make me very sick and that anything else I tried to do
for myself - in particular, any changes I made to my diet - would be useless
and a waste of time...
I had found a copy of Ian Gawler’s book, You Can Conquer Cancer, and had read most of it. Everything he
said in there made sense to me and, besides, I obviously had nothing to lose by
taking on an approach in which I took an active and positive role in the
recovery I hoped to make. I did not dismiss what the doctors had to say; I used
it as a starting point and did heaps of research on my cancer and the exact
types of chemotherapy drug treatments that had been tried in the past. I found
yet another oncologist who was prepared to try the slightly unorthodox chemo
that I had uncovered in my research... My doctor was sceptical but, with no other
real options, he decided there was nothing to lose and he got on with it...I also
enrolled in the Gawler Foundation’s 10-day course at the Yarra Valley Living
Centre. What I learned and how deeply I changed during those 10 days changed
not only the length of my life - I am totally convinced of that - but also the
quality of my life. In particular, I realised that there were things that I
could do that could change not only the course of the disease but the quality
of the journey along the way...
After the course, I had tonnes of information
- and I knew how to go about finding tonnes more - about how to maximise my
chances of healing through eating well. Although one of the first doctors I saw
told me that fresh juices were a waste of time and that all that would happen
was that my skin would turn orange from the carrots, which it did a bit, it
just made total sense to me that every nutrient or toxin I put into my body
would have some influence on my immune system and my outcome. I also grew to
love and value my time out while meditating. Again, I am absolutely certain
that it influenced my outcome.
Committee
Hansard 18.4.05, pp.55-6 (Ms
Barb Glaser).
Navigation: Previous Page | Contents | Next Page