Chapter 2
Prevalence of mental ill-health
Introduction
2.1
This chapter considers the extent and significance of mental ill-health
in Australian Defence Force (ADF) members, veterans, and the families of ADF
members and veterans.
Healthy soldier effect
2.2
When considering any occupational health study (and especially studies
of military populations) it is important to note the 'healthy worker effect', in
which people who are employed exhibit a lower mortality rate than the general
population. This effect is often primarily attributed to a selection bias
whereby people who are employed are, on average, healthier than the general
population, which includes people who are severely ill or disabled and
therefore unable to work. Military populations are, on average, far healthier
than other employed populations, which are in turn healthier than the general
population. The 2010 ADF Mental Health Prevalence and Wellbeing Study (MHPW
study) noted that:
The 'healthy worker effect' comes from the fact that, during
recruitment, the ADF takes steps not to enlist individuals with pre-existing
disorders. It then provides quality and accessible health services to all of
its members. In addition, there is an occupational health service in the ADF
that provides quality care at no cost to ADF members and, following deployment,
ADF members are extensively screened to ensure they receive treatment if they
need it. The ADF workforce should, therefore, be healthier than the general
community.[1]
2.3
Some occupational health studies of military cohorts refer to this as
the 'healthy solider effect'.[2]
A number of submissions highlighted the importance of acknowledging the
'healthy solider effect' when considering the prevalence of mental disorders
for current and former ADF personnel.[3]
The Australian Families of the Military Research and Support Foundation (AFOM)
asserted that 'research done in this area, which does not provide for the
Healthy Soldier Effect (HSE) does not reflect the true extent and significance
of the issues' and called for all future research to take the effect into
account.[4]
Prevalence of mental ill-health in the Australian Defence Force
2.4
The MHPW study was the first comprehensive investigation of the mental
health of an ADF serving population. The study examined the prevalence rates of
the most common mental disorders, the optimal cut-offs for relevant mental
health measures, and the impact of occupational stress factors. Nearly 49 per
cent of ADF members serving during the time of the study (April 2010 to January
2011) participated.[5]
2.5
The MHPW study obtained normative mental health data from the Australian
Bureau of Statistics (ABS) in order to interpret and fully understand the rates
of mental disorders reported in the ADF. The ABS data, derived from the 2007
ABS National Survey of Mental Health and Wellbeing, was adjusted to match the
demographic characteristics of the current ADF serving population (for age,
sex, and employment status).[6]
2.6
The study found that more than half of the ADF population had
experienced a mental disorder in their lifetime, a significantly higher rate
than experienced by the general Australian population. The study noted that
'this level of mental illness in the ADF suggests that, despite the fact that
the ADF is a selected and trained population that generally has better access
to health care (the 'healthy worker effect'), this population is affected by a
range of stress factors caused by the nature of their work'.[7]
Prevalence of mental disorders
2.7
The MHPW study found that 22 per cent of the ADF population (11,016) had
experienced a mental disorder in the previous 12 months and that approximately
6.8 per cent (760) of those who had experienced a mental disorder had
experienced more than one mental disorder at a time. The MHPW study noted that
while the prevalence of mental health disorders in the previous 12 months was
similar to the general Australian population sample, the profiles of specific
disorders in the ADF varied.[8]
Table 2.1 provides the estimated prevalence of lifetime and 12-month mental
disorders in the ADF and compares this to the ABS sample matched by age, sex,
and employment status.
Table 2.1–Estimated prevalence of
lifetime and 12-month disorders
|
|
Lifetime prevalence
|
12-month prevalence
|
|
|
ABS %
|
ADF %
|
ABS %
|
ADF %
|
|
Any affective disorder
|
14.0
|
20.8*
|
5.9
|
9.5*
|
|
Any anxiety disorder
|
23.1
|
27.0
|
12.6
|
14.8
|
|
Any alcohol disorder
|
32.9
|
35.7
|
8.3
|
5.2*
|
|
Any mental disorder
|
49.3
|
54.1*
|
20.7
|
22.0
|
* Significantly different
from the ABS study.
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xv.
2.8
The MHPW study found that the most significant difference between the
ADF population and the general Australia population sample was the prevalence
of affective disorders (also known as mood disorders) (See Figure 2.1). It
found that depressive episodes in both male (6.0 per cent) and female (8.7 per
cent) ADF members were significantly higher than the general community rates
(2.9 per cent and 4.4 percent respectively). There were no significant
differences, however, between ADF males and ADF females in the prevalence of
affective disorders.[9]
Figure 2.1–Estimated prevalence of
12-month affective disorders, ADF and ABS data
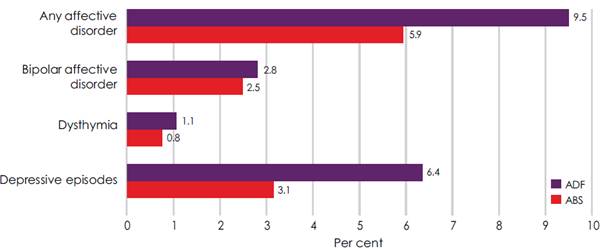
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xix.
2.9
The MHPW study found that the most common mental disorders in the ADF
were anxiety disorders, with the most prevalent anxiety disorder being
post-traumatic stress disorder (PTSD) (see Figure 2.2). The overall prevalence
of anxiety disorders was not found to be significantly higher than in the general
Australian population. The primary difference between the ADF and the general
Australian population was the significantly higher rates of PTSD in ADF males
(8.1 per cent compared to 4.6 per cent) and the significantly lower rates of
panic disorder in the ADF (1.2 per cent compared with 2.5 per cent). The study
noted that, as is the case in the general Australian population, female ADF
personnel rated higher than male ADF members on anxiety disorders and were
significantly more likely to have panic attacks or panic disorder.[10]
Figure 2.2–Estimated prevalence of
12-month anxiety disorders, ADF and ABS data
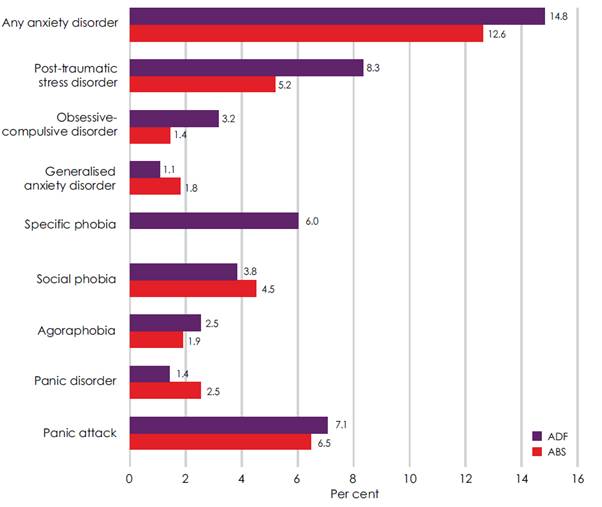
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xix.
2.10
The MHPW study also found that both male (3.1 per cent) and female (1.3
per cent) ADF members had significantly lower rates of alcohol harmful use
disorder compared to the general Australian population (5.5 per cent and 3.7
per cent respectively) (See Figure 2.3). ADF females were significantly less
likely to have an alcohol disorder than ADF males.[11]
Figure 2.3–Estimated prevalence of
12-month alcohol disorders, ADF and ABS data
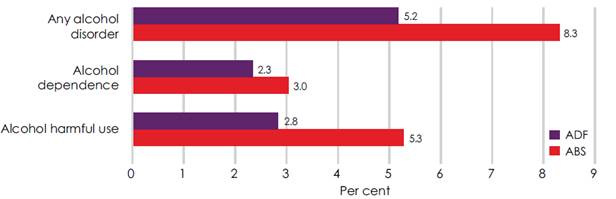
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xx.
Future research
2.11
The Departments of Defence and Veterans' Affairs are currently funding
the largest and most comprehensive study undertaken in Australia to examine the
impact of military service on the mental, physical and social health of serving
and ex-serving ADF personnel and their families. The Transition and Wellbeing
Research Programme, led by the Centre for Traumatic Stress Studies (CTSS) at
the University of Adelaide, consists of three studies: the Mental Health and
Wellbeing Transition Study, the Impact of Combat Study, and the Family
Wellbeing Study.[12]
2.12
The Mental Health and Wellbeing Transition Study will:
-
determine the prevalence of mental disorders amongst personnel
who have transitioned from full-time service between 2010 and 2014;
-
examine the physical health status of serving and ex-serving
personnel;
-
investigate pathways to care for serving and ex-serving
personnel, with a priority on those with a diagnosed mental disorder;
-
examine factors that contribute to the current wellbeing of
serving and ex-serving personnel;
-
investigate how mental health issues change over time, especially
once an individual transitions from full time service;
-
investigate technology and its utility for health and mental
health programs, including implications for future health service delivery; and
-
investigate the mental health and wellbeing of current serving
reservists.[13]
2.13
The research program will survey a cohort of approximately 24,000
transitioned service personnel, together with current serving personnel and
reservists (drawing from the Military and Veteran Research Study Roll)[14]
for the Mental Health and Wellbeing Transition Study and the Impact of Combat
Study. The Family Wellbeing Study is being conducted by the Australian Institute
of Family Studies and will survey family members nominated by the participants
of the other two studies.[15]
2.14
The research program is also actively following up with all participants
of the 2010 ADF Mental Health Prevalence and Wellbeing Study Report as well
as participants of the Middle East Areas of Operations (MEAO) Census Health
Study. This will allow the research program to conduct both a prevalence
study and a longitudinal follow up.[16]
2.15
Prior to its closing in December 2014, the Centre for Australian
Military and Veterans' Health conducted epidemiological studies that provide a
comprehensive picture of the health of serving members, veterans, and their
families following specific deployments including:
-
Rwanda Deployment Health Study (2014);
-
Middle East Area of Operations (MEAO) Health Study – Mortality
and Cancer Incidence Study (2013);
-
Middle East Area of Operations (MEAO) Health Study – Census Study
(2012);
-
Middle East Area of Operations (MEAO) Health Study – Prospective
Study (2012);
-
Timor-Leste Family Study (2012);
-
Bougainville Health Study (2009);
-
East Timor Health Study (2009); and
-
Solomon Islands Health Study (2009).[17]
Linking research to policy
2.16
Dr Annabel McGuire noted that whilst research studies have added to the
fundamental scientific understanding of the impact of military service on ADF
personnel and their families, 'the biggest flaw in this work was that the
Departments and the research teams failed to work together to translate the
findings into actionable policy and programs' and that the research was
generally not well received by the broader Defence community:
In general terms, the research has not been well received by
the broader Defence community, in part because scientific reports do not tell
people's story: reading that eight percent of the Defence Force has screened
positive for PTSD in the past year does not feel right when you look around and
can see four guys in your section are struggling. The answer to this problem is
not to commission new and bigger research projects aiming to be the panacea for
the failings of previous research. The disenfranchised ex-service community
does not respond well to another survey from which they see no outcome.
Research must be explicitly and overtly linked to changes in policy and/or practice.[18]
Heightened risk factors of service
2.17
The Chief of the Defence Force, Air Chief Marshal Mark Binskin AC, told
the committee that Defence 'acknowledge[s] that military service creates unique
stresses'[19].
DVA explained that the 'day to day stressors of military service can include
significant periods away from home, family and friends while on posting and
reduced access to social and family supports, including the impact on spouses
and children'.[20]
Impact of deployment on mental
health
2.18
As at January 2011, approximately half of all ADF personnel have been
deployed multiple times. In the MHPW study, 43 per cent of ADF personnel
participating reported being deployed multiple times, 19 per cent reporting
being deployed once and 39 per cent never having been deployed.[21]
Every year, approximately 12,000 ADF personnel are in the 'operational
deployment cycle', meaning that they are preparing, deploying or transitioning
home.[22]
2.19
Between July 2013 and June 2014, 896 ADF personnel were referred to the
ADF Rehabilitation Program with a primary diagnosis of a mental health
disorder. Of these, 33.6 per cent were identified as being 'deployment
related'. In this period, 206 of the 896 personnel were referred with a
specific diagnosis of PTSD, of which 84 per cent were identified as being
'deployment related'. Since 2000, 108 ADF personnel are suspected or confirmed
to have died as a result of suicide, of which 47 had previously deployed.[23]
2.20
The findings of the MHPW study indicated that there was no significant
link between deployment and an increased risk of developing PTSD, anxiety,
depression or substance abuse disorders, stating that 'deployed personnel did
not report greater rates of mental disorder than those who had not been
deployed'.[24]
However, the Chief of the Defence Force acknowledged that the risk of
experiencing a traumatic event increases during deployment and that exposure to
trauma increases the risk of poor mental health outcomes:
Our research clearly shows that exposure to trauma increases
a person's risk of developing a mental health condition or problem, as you
would expect. Some people will be exposed to trauma while on operations. Others
may experience traumatic events outside a deployment or military service.
Despite reports to the contrary, we fully accept that the risk of experiencing
a traumatic event increases during a deployment whether it be to a conflict
zone, during a humanitarian or disaster relief mission or in border protection
operations.[25]
2.21
Defence advised that for the majority of ADF members who have been
deployed on a warlike operation (81.7 per cent), their cumulative time on a
warlike operation equates to one year or less (see Table 2.2).
Table 2.2–Cumulative time on a
warlike operation
|
Time
|
1 year or less
|
Between 1 and 2 years
|
Between 2 and 3 years
|
More than 3 years
|
|
ADF members
|
40,959
(81.7 per cent)
|
8,367
(16.7 per cent)
|
737
(1.5 per cent)
|
56
(0.1 per cent)
|
Department of Defence, answer
to question on notice, 2 June 2015 (received 15 July 2015.
Exposure to traumatic events
2.22
The Australian Psychological Society noted that 'it is well known that
the unique occupational risks of ADF service include significant exposure to
potentially traumatic events'.[26]
The MHPW study agreed, noting that:
...members of the ADF are at risk of developing mental
disorders, as they are exposed to a range of occupational stressors – for
example, exposure to traumatic events and extended periods of time away from
their primary social support networks.[27]
2.23
Defence reported that the most common potentially traumatic event
reported by deployed personnel in the Return to Australia Psychological
Screening in Annual Mental Health Surveillance Reports has consistently been
'in danger of being injured', followed by 'in danger of being killed'. Defence
noted that this was different for Navy personnel deployed on Operation Resolute,
who reported in the Mental Health and Wellbeing Questionnaire that the most
common exposure was 'witnessed human degradation/misery on a large scale'
followed by 'in danger of being injured'.[28]
2.24
In addition to considering the number of traumatic experiences, the MEAO
report also considered the types of traumatic combat-related experiences
associated with PTSD symptoms. The MEAO study found that participants who
reported experiencing five or more types of traumatic exposure were
statistically significantly more likely to have adverse psychological health
outcomes.[29]
The MEAO study found that exposures such as 'threatening situation and unable
to respond', 'handling/seeing dead bodies', and 'being witness to human
degradation and misery' were strongly and statistically associated with PTSD
symptoms.[30]
2.25
The MHWP study also considered the proportion of those personnel exposed
to traumatic events that go on to develop PTSD (see Figure 2.5). The event associated
with the highest rates of PTSD was 'being kidnapped or held hostage', with 78.5
per cent of those who had experienced this event having PTSD. Other events that
were associated with very high rates of PTSD were rape (42.3 per cent), being
stalked (38.4 per cent), and domestic violence (31.1 per cent). The rate of
PTSD for serving as a peacekeeper (9.2 per cent) and combat experience alone
(10.4 per cent) were comparatively quite low. The
MHWP study commented that:
In summary, these results provide an insight into the fact
that certain aspects of military service such as combat or peacekeeping do not
per se present major risks to post-traumatic stress disorder. Rather, it is
likely that there are certain experiences within military service, such as seeing
atrocities or accidently injuring or killing another individual, which may be
particularly damaging to an individual's psychological health.[31]
2.26
DVA advised the committee that in addition to the risk of exposure to
potentially traumatic experiences during deployment, ADF members may also be
exposed to potentially traumatic experiences during peacetime service
activities, for example during disaster assistance or as a result of serious
training accidents:
Any military service involves risk of exposure to traumatic
experiences, such as trauma arising from disaster assistance or serious
training accidents. For instance, in 1996 two Black Hawk helicopters collided
and crashed at the High Range Training Area near Townsville, resulting in the
deaths of 18 personnel and injuries to a further 12 personnel. In 2005, a Sea
King helicopter crashed on Nias Island in Indonesia while on a humanitarian
support mission, with the deaths of 9 ADF personnel.[32]
2.27
The MHWP study commented on the difficulty of clearly differentiating
between traumas experienced during ADF service and traumas experienced in ADF
members' private lives, noting that for clear conclusions to be drawn regarding
the impact of ADF service 'traumas experienced during military service and in
the private lives of ADF members need to be separated'.[33]
Figure 2.4–Estimated prevalence of
lifetime trauma exposure in the ADF
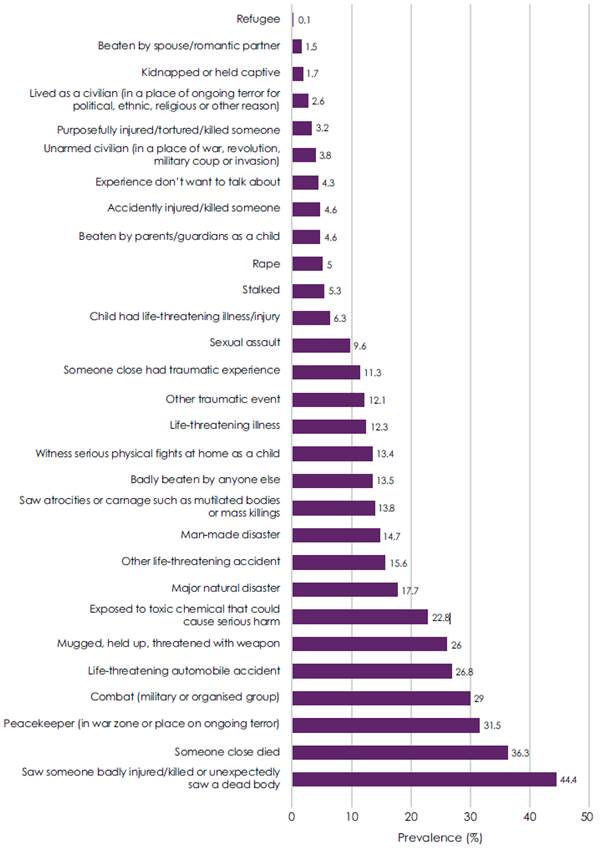
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. 49.
Figure 2.5–Estimated prevalence of
post-traumatic stress disorder from specific event types
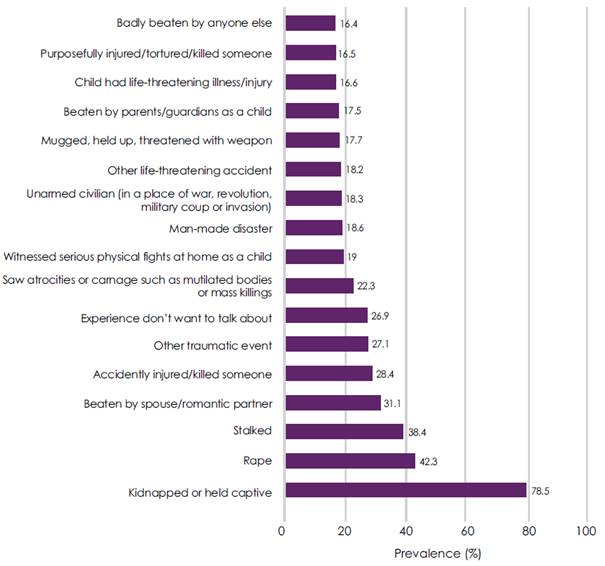
Department of
Defence, Mental Health in the Australian Defence Force: 2010 ADF Mental
Health Prevalence and Wellbeing Study Report, p. 50.
2.28
The committee received powerful evidence from veterans who described
the traumatic experiences that they were exposed to during their service and
the impact that it has had on their mental health. Slater & Gordon gave
numerous examples of clients' traumatic experiences on deployment. A veteran
solider and combat first-aider who was deployed to Afghanistan and suffers from
chronic PTSD stated:
I was a scout in my section and we were doing a cordon and
research mission. I was providing security when the IED went off...I first came
across Private [name omitted] who had his leg blown off, he had a tourniquet on
and was being treated; I was stunned for a split second. People were screaming
and shouting. I then realised my friend [name omitted] had been killed. There
were bits of his body, his body armour and kit strewn across the field. There
was a child that had his toes blown off from the blast that had begun running
away from us at that point. There were three Afghan civilians lying on the
ground who had major blast injuries and who I commenced treating. After the
first helicopter took the Private away and the second helicopter took the
civilians, the last helicopter came to get the last casualty and my friend's
body. As I loaded the last casualty onto the helicopter it hit me when I saw
his name written across his body bag, my heart sank as the realisation of what
happened set in. The helicopter took off and my sergeant asked me to help him
pick up some body parts that had been forgotten in the chaos.[34]
2.29
The following was conveyed by Slater & Gordon Lawyers from a
returned servicemen of the East Timor Peacekeeping Mission suffering PTSD and
depressive symptoms and who attempted suicide during deployment:
During my deployment there we were also stopped by distressed
locals during one of our patrols. The Timorese led our patrol section to a
burnt out building...towards the back of the building in one of the rooms, there
was a local woman. The woman was deceased and surrounding her was an evident
smell of fuel. I drew my own conclusion that she appeared to have been doused
with petrol, set alight and shot in the head. We carried her outside and once
in the open, I could see the poor woman was a mother.
Fused to her was the baby that she must have been holding at
the time of her execution...I see this woman and her child whilst sleeping and
often for no reason start to think of her during my day to day goings on. I
feel ashamed that I was not there fast enough to stop what happened. I feel
angry that a helpless woman and her baby were killed in such an inhumane
manner. I cannot seem to shake what happened to her and feel immense anger at
how an innocent child was burnt (most possibly whilst it was still alive). I am
haunted by this and often find myself getting teary. It just doesn't go away.[35]
2.30
Mr Matthew McKeever told the committee of his repeated exposure to
highly traumatic situations across five deployments during his 16 years of
service:
I killed my first person on 30 August 2010—retrieved the
body; you are required to fingerprint it and required to iris scan. I was
offered no mental support after that. I then had dealings with other dead
Taliban who were killed by other people where I was required to physically examine
them for bullet holes. On occasion when I would lift their arms up my fingers
would go through their wrists from the bullet holes. Because of that, I have no
sexual function. I have to inject myself with a needle; I can show you it. If I try to have sexual intercourse with my partner, I get
flashbacks from my fingers going into dead people. So I have to inject my penis
with a needle of the size I am showing you—it is quite large—which is not nice.
So I have no sexual life, and I have not slept with my wife for over 12 months
due to severe nightmares.
My second deployment to Afghanistan was totally different. My
first one was high activity with numerous contacts, numerous IED explosions and
handling numerous dead bodies. My second one was quite different. I knew I had
a problem, but then I was exposed to the handling of dead children. In one
instance with one child, I had to pick the little boy up by his ankles and
shake him to prove to his parents that he was deceased. Then when I returned
from Afghanistan I tried to commit suicide because I saw my child and that
brought back a lot of memories.[36]
2.31
Mr McKeever acknowledged that the risk of exposure to traumatic
experiences is inherent to deployment as an infantry solider but asserted that
the risk is poorly managed. Mr McKeever pointed to policies that increased
exposure to potentially traumatic experiences for soldiers who must 'process'
(iris and finger print scan) the human remains of those they have killed. Mr
McKeever called for specialised teams of medical officers to process human
remains to minimise this risk:
I know what an infantry soldier does. But there should be
people in specialised areas, as they had in East Timor and other places, so
that when you kill somebody and they have to be dragged out and processed,
there is a specialist team that comes out and does that—medical officers. I
told my soldiers, 'If you do not have to see the dead body, don't see it.'[37]
2.32
Defence advised the committee that the collection of biometric
information, as referred to by Mr McKeever, is authorised by and must comply
with Defence Instructions (General) Operations 13-16 which states, 'biometric
samples, including collection by invasive techniques, may be taken from human
remains but only if this can be done without mutilating or otherwise
maltreating the remains. The utmost respect is to be shown to human remains at
all times'. Defence noted that the approach and manner in which ADF members'
process human remains is shaped by the requirements of the operation as well as
the operational environment and tactical situation.[38]
Defence's policies regarding operational mental health and psychology support
in the pre-deployment, deployment, and post-deployment phases are discussed in
Chapter 3 of this report.
Abuse
2.33
The ADF has had a long history of incidents of reported abuse and
harassment (including sexual abuse) within its ranks. The Senate Foreign
Affairs, Defence and Trade References Committee has previously conducted
inquiries which have addressed, or touched upon, abuse and sexual harassment in
Defence. These inquiries have included:
-
Processes to support victims of abuse in Defence (October 2014);
-
Report of the review of allegations of sexual and other abuse in
Defence, conducted by DLA Piper, and the response of the government to the
report (June 2013);
-
Inquiry into an equity and diversity health check in the Royal
Australian Navy – HMAS Success (September 2011);
-
The Effectiveness of Australia's military justice system (June
2005); and
-
Sexual Harassment in the Australian Defence Force (August 1994).[39]
2.34
A number of submissions commented negatively on 'ADF culture' and detailed
members' and veterans' personal accounts of abuse in the ADF and its effect on
mental health.[40]
Mr Ciaran Hemmings told the committee of his experience of abuse following a
physical injury and its impact on his mental health:
I have done six years in Defence. I did not deploy. I
sustained my injury whilst on rifle combat at Butterworth over in Malaysia on a
training exercise. I crushed my right arm whilst over there. Mental health
within Defence is—like [Mr McKeever] said, they do not care at the end of the
day. The names you get called—I have got a body suit because I have got severe
nerve pain. I also suffer from adjustment disorder with anxiety and depression.
And in the pack mentality of Defence that does not sit well, as [Mr McKeever]
said, and probably the others. As soon as you are injured, you are like a
dog—you are kicked out of the pack and there is no way of getting back into
that pack. I was injured in 2013. I tried my hardest to get better, but the
ridicule within Defence was phenomenal. Every time I tried to do something it
would be like, 'Don't do that—you might hurt your other hand' or 'Come on,
Michael Jackson, give us a moonwalk'. It is shocking. It just makes the
mentality worse. You can speak to hierarchy about it and you get ridiculed
also, like officers and so forth. You get to the point where you fear to even
speak up...It just came to the point where I had to go to the doctor on base
myself and ask for help because I was the same: I was at the point where I
would sit at home at night and think about suicide. It got really hard, to the
point where—I have got three children—it come down to being there for my kids.
I could not do this without help and seeing [Dr Niall McLaren, psychiatrist].
The way work treated you—I hated going to work. I would sit at the back gate
and struggle for half an hour to even drive into that place knowing that as
soon as you did you would just get ridiculed and picked on for your condition.
It is massive in Defence and it is not
looked at at all. I spoke up to mates, and stuff like that, and they would just
say, 'Harden up, princess. It's not that bad.' But once you have got an injury
and you are kicked out of the pack, and because you have got your brethren and
your mates and stuff, the next minute you are pushed off to the side,
literally. They will grab you and they will sit you in another building away
from all the non-injured personnel. That is where you sit until you are kicked
out.[41]
2.35
Although not the subject of this inquiry, it is important to acknowledge
the enormous impact that harassment, bullying, and abuse (sexual and otherwise)
may have on the mental health of both the subject of harassment, bullying, and
abuse as well as witnesses. Chapter 5 of this report will consider the stigma
associated with mental ill-health and its impact in greater detail.
Prevalence of mental health disorders in veterans
2.36
The Department of Veterans' Affairs (DVA) informed the committee that as
at March 2015, it was supporting 147,318 veterans with one or more disabilities
accepted by DVA and of these, 49,668 veterans had one or more accepted mental
health disabilities (See Table 2.3). DVA advised the committee that there are
two pathways by which veterans may apply to DVA:
-
the liability pathway: if they have mental health conditions
related to service in the ADF, in order to receive compensation and treatment;
and
-
the non-liability pathway: if they have certain mental health
conditions whatever the cause, in order to receive treatment only.
Table 2.3–Veterans with mental
health conditions accepted by DVA, March 2015*
|
Number of veterans with
|
Related to service
(liability)
|
For any cause
(non-liability)
|
Net total
|
|
One or more accepted
disabilities
|
143,652
|
34,451
|
147,318
|
|
One or more accepted
mental health disabilities
|
45,953
|
15,526
|
49,668
|
|
PTSD and other stress
disorders
|
28,875
|
11,705
|
31,501
|
|
Depression or dysthymia
|
11,649
|
4,102
|
13,976
|
|
Alcohol and other
substance use disorders
|
13,273
|
322
|
13,532
|
|
Anxiety
|
10,406
|
2,214
|
11,932
|
|
Adjustment disorder
|
1,911
|
N/A
|
1,911
|
* Note: This table is a count
of claims. Some individuals are counted multiple times.
Department of Veterans'
Affairs, Submission 35, p. 12.
2.37
Figure 2.6 sets out the top mental health conditions, as at March 2013,
grouped into conflict cohorts.
Figure 2.6–Top mental health
conditions as at March 2013, includes VEA, MRCA &SRCA
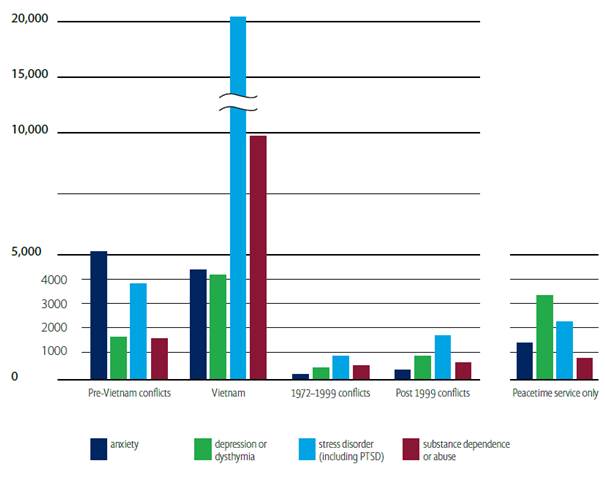
Department of Veterans'
Affairs, Veteran Mental Health Strategy: A Ten Year Framework 2013-2023,
p. 28.
2.38
Table 2.4 shows the number mental health claims accepted by DVA each
year over the past decade; a rate of between 3,100 and 5,350 claims per year.
Table 2.4–Flow of accepted mental
health claims accepted by DVA, January 2015
|
|
2004
|
2005
|
2006
|
2007
|
2008
|
2009
|
2010
|
2011
|
2012
|
2013
|
2014
|
|
Related to service (liability)
|
4,185
|
3,764
|
3,160
|
3,197
|
2,928
|
2,779
|
2,458
|
2,332
|
2,748
|
3,412
|
3,579
|
|
For any cause (non-liability)
|
1,158
|
1,228
|
1,146
|
819
|
841
|
880
|
786
|
758
|
956
|
1,149
|
1,680
|
|
Net total
|
5,343
|
4,992
|
4,306
|
4,016
|
3,769
|
3,659
|
3,244
|
3,090
|
3,704
|
4,561
|
5,259
|
* Note: some veterans are
counted multiple times if they have more than one condition.
Department of Veterans'
Affairs, Submission 35, p. 12.
2.39
The Returned & Services League of Australia (RSL) questioned the
numbers provided by DVA, asserting that the potential number of veterans with
service-related mental health problems could be significantly higher, noting
that it is estimated that only one in five veterans have DVA client numbers:
Senator Michael Ronaldson, Minister for Veterans' Affairs,
reports that DVA clients number approximately one in five of all Australians
who have service in the ADF. Using DVA's approximate current client numbers of
330,000, this means that the potential number of veterans suffering
service-related mental ill-health could be significantly higher than those who
have lodged claims.
As ex-serving members are not compelled to register with DVA
unless they want to claim for a service-related injury or illness, the extent
of mental ill-health among ex-serving men and women is unknown. Given the
typical presentation some eight to 10 years after discharge and the experience
following the Vietnam War of delayed onset of symptoms, it is highly likely
that there are significant numbers of veterans with service related mental
ill-health who are as yet unknown to DVA.[42]
2.40
Phoenix Australia noted that 'many mental health problems may not be
obvious while the person is still serving and may not become apparent until
months or years after serving'.[43]
The RSL commented that 'the lack of information in this area is concerning but
the sheer numbers of veterans seeking RSL support alone is enough to indicate
that this is a severe problem'.[44]
Soldier On also expressed concerns with DVA data, noting that 'once a person
discharges from the military there are no records kept of their on-going or
developing physical or mental health concerns, hospitalisation or deaths unless
the treatment is provided through DVA'.[45]
2.41
The record-keeping policies and processes for both Defence and DVA will
be considered in greater detail in Chapter 5 of this report.
Suicide
2.42
Suicide is a leading cause of death in Australia. In 2013, deaths due to
suicide occurred at a rate of 10.9 per 100,000 people. The median age at death
for suicide was 44.5 years for males, 44.4 years for females, and 44.5 years
overall. In comparison, the median age for deaths from all causes in 2013 was
78.4 years for males and 84.6 years for females.[46]
Of deaths due to suicide, 75 per cent are male, making it the tenth leading
cause of death for males in Australia.
Suicidality in ADF population
2.43
Defence advised the committee that since 2000, 108 ADF members are
suspected or have been confirmed to have died as a result of suicide.[47]
The MHPW study found that the rate of suicidality (thinking of suicide and
making a suicide plan) in the ADF was more than double that in the general
community; however the number of suicide attempts was not significantly greater
than in the general community and the number of reported deaths by suicide in
the ADF were lower than in the general population when matched for age and sex.
The study noted that there is a gradation of severity of suicidality in the
ADF, ranging from those with suicidal ideation (3.9 per cent) through to those
making a plan (1.1 per cent) and those actually attempting suicide (0.4 per
cent) (see Table 2.5).
Table 2.5–Estimated prevalence of
12-month suicidality, by sex, ADF and ABS data
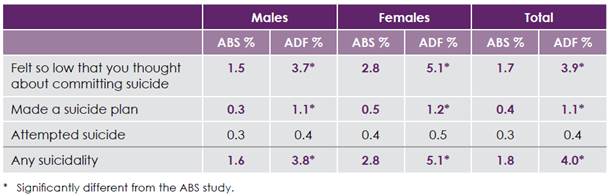
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xxi.
2.44
The MHPW study commented that although ADF members are more symptomatic
and more likely to express suicidal ideation than people in the general
community, they are only equally likely to attempt suicide and less likely to
complete the act, and that this suggests that 'the comprehensive initiatives on
literacy and suicide prevention currently being implemented in Defence may, in
fact, be having a positive impact'.[48]
Suicidality in ex-service
population
2.45
DVA informed the committee that it has determined 85 claims relating to
death by suicide over the last ten years (to 31 December 2014). Of the 85
claims, 57 were accepted as service related; and of the 57 claims, 22 veterans
were aged 55 years or under at death. DVA advised that it is only made aware of
a death by suicide when a dependant lodges a compensation claim:
Generally, DVA only becomes officially aware of a death by
suicide of a veteran through the dependant's compensation claim process. This
occurs when a claim for compensation is lodged by a dependant in respect of the
death of that veteran and a cause of death must be investigated to establish a
link to service.[49]
2.46
A number of submissions highlighted the difficulty of accurately
estimating suicidality of veterans and expressed concern about the lack of data
regarding veteran suicide.[50]
Some submitters called for the government to monitor and maintain a public
record of suicide, suspicious death, single vehicle accidents and other deaths
by misadventure.[51]
The RSL also noted that suicide data is further complicated by deaths that are
not definitively confirmed to be suicides:
When death occurs as a result of self-harm in association
with existing mental health difficulties, unless it is very clear, e.g.
self-inflicted injury or overdoses, then the cause of death is very often left
open by the coroner. This action produces inaccurately low figures with regard
to suicide figures particularly when substance abuse, motor vehicle accidents
and cliff falls are involved. In addition there may be no mention of a mental
health history on the death certificate at all.[52]
2.47
Soldier On stressed the importance of accurate and transparent data
regarding veteran suicide noting that without accurate data it is impossible
for both government and non-government support providers to properly address
the issue:
...very little is known about how many veterans are taking
their own lives. Community groups are gathering anecdotal data, but without any
reliable sources collecting the information, it is impossible for any support
provider (government or non-government) to truly understand the extent of the
issue...it is our recommendation that data around the ongoing health implications
among serving and ex-serving members over the past five to 10 years is collated
as a priority by the Department of Veterans' Affairs. It is also important this
information is gathered regularly and made available to the public in a
de-identifiable format, in order for the issues to be quantified and a reasoned
response and solution be prioritised.[53]
2.48
DVA advised the committee that in November 2014 it commissioned the
Australian Institute of Health and Welfare to carry out a data matching
exercise between deceased military superannuants from ComSuper and the National
Death Index for reported incidents of suicide from 2001 onwards. DVA advised
that it expects to receive the findings from this work in late 2016.[54]
DVA has also commissioned the Australian Institute for Suicide Research and
Prevention (Griffith University), to conduct a literature review to examine
suicide amongst veterans in Australia and internationally, and how this
compares to the general population.[55]
2.49
Recent research into suicidality in Australian Vietnam veterans and
their partners found that suicidality was higher in veterans than in the
Australian community. The study assessed the lifetime suicidality of a cohort
of 448 Australian Vietnam veterans during in-person structured psychiatric
interviews that permitted direct comparison with age-sex matched Australian
population statistics finding that:
Relative risks for suicidal ideation, planning and attempts
were 7.9, 9.7 and 13.8 times higher for veterans compared with the Australian
population ...PTSD, depression, alcohol disorders, phobia and agoraphobia were
prominent predictors of ideation, attempts and suicidal severity among
veterans.[56]
2.50
Similarly, the 2005 Australian National Service Vietnam Veterans:
Mortality and Cancer Incidence report found that there was a significant
increase in the relative rate for suicide for veterans:
There was a significant increase in the relative rate for
suicide, based on 129 deaths observed amongst the National Service veterans and
115 deaths observed amongst non-veterans. This gave a relative rate of
1.43...this relative rate was higher than that noted in the previous study of
this cohort.[57]
2.51
Dr Kieran Tranter pointed to the Veterans Line statistics as a possible means
of providing insight into veteran suicidality, noting with concern the
increasing number of clients identified as at significant risk of suicide or
self-harm:
The Veterans Line also provides a call-back service for
clients who may present as being at significant risk of suicide or self-harm.
In 2012-13 the service identified and made 52 call-backs to veterans who
presented such risks compared to only 21 call-backs in 2011-12. The number of
call-backs made in 2013-14 rose significantly again to 122 clients being
identified as requiring the call back service...these figures are alarming, as
the numbers of clients who have been identified as at significant risk of
suicide or self-harm have doubled each year since 2011-2012.[58]
Prevalence of mental ill-health in families of ADF members and veterans
2.52
A number of submissions highlighted the impact ADF members and veterans
struggling with mental ill-health can have on their families.[59]
The War Widows' Guild of Australia told the committee that 'veterans with
PTSD/mental ill-health issues have impacts on the entire family', explaining
that the mental health of the families of ADF members and veterans are impacted
as a result of the ADF member or veterans' service:
There is anecdotal evidence that many War Widows have
suffered forms of abuse, be it physical, emotional or psychological as a result
of their spouse/partner/significant others service in an area of conflict.
These women have been reluctant to discuss their issues for fear of social
rejection, isolation, embarrassment, feeling that this violence is 'their
fault' rather than as a symptom of their spouses/partners mental ill-health.[60]
2.53
The committee received evidence from ADF members' and veterans'
partners, describing their experiences living with and supporting partners
struggling with mental ill health.[61]
Miss Alanna Power detailed her experiences supporting her partner Mr Ryan
Geddes, during an incident in which he was engaging in dangerous self-harm:
Ryan [her partner] was deployed to Afghanistan as a combat
engineer in 2010 on MTF1 and again in 2011 in a non-combat role...As a combat
engineer, Ryan experienced many traumatic events, some of which I know he will
probably never tell me about. In 2014 he was diagnosed with PTSD, anxiety and
depression, although his first symptoms appeared in early 2012...Some of the
symptoms that Ryan experiences include major anxiety about being in public or
meeting new people, hypervigilance, night terrors, self harming, serious
depressive episodes, anger control issues, lack of empathy and the inability to
sleep without medication.
In October 2014 I came home from work to find Ryan with a
large hunting knife engaging in a serious self harming incident. I was on my
own and could not get the knife off him and so the police and paramedics were
called to diffuse the situation. The knife was only handed over once the police
pepper sprayed Ryan in the face...I was informed by the hospital that Ryan was in
a dissociative state when he was self harming. This episode was triggered by
the air conditioning blowing up in Ryan's car while he was driving. Essentially
he was transported back to a traumatic event which occurred in Afghanistan.[62]
2.54
Mr Geddes told the committee of his struggle identifying his mental
illness due to the pressure and stigma associated with mental ill-health as
well as the impact that this had on Miss Powers:
I knew that there was something wrong. I did not know what it
was. I was angry. I was drinking a lot, and I was taking a lot of it out on
Alanna. Yes, I did know that there was something there, but I did not want to
admit to it...It was a weakness, and up until early this year I still thought of
it as a weakness. Until all my friends told me, my partner told me, my parents
told me, and I just told them to get you know, that I was fine. I did not want
to process; I did not want to go through that way because I wanted to still be
able to work. I thought if I do say anything about this, then that is me, I am
never going to be able to get a job doing what I want to do again.[63]
2.55
Mrs Catherine Lawler told the committee about her experience supporting
her husband, Mr John Lawler, describing herself as 'worn out and worn down' and
'angry too'. Mrs Lawler explained that she disengaged emotionally from her
husband to cope with the situation and even contemplated suicide to 'stop
[herself] from sharing his pain':
John has withdrawn from involvement in the day to day tasks
of our domestic lives, and I undertake all household chores, inside and outside
the house, and financial dealings. I generally liaise with doctors, government
departments, his RSL advocate, etc. on John's behalf. We will often go for long
periods where I also do all of the driving. All of this has had an impact on my
physical health, and I am constantly fatigued. I have gradually withdrawn from
the workforce to be John's fulltime carer.
The anger and rage that engulfed John increased the tension
between us to unbearable levels. I tried to be supportive, I tried to
understand, but I was struggling. I was worn out and worn down. There were many
times when I was angry too. I know I could not be his wife and his psychiatrist
too.
I found myself in a position where the best thing to do was
disengage from John, go about my daily business and pretend I did not care. But
I did care, and his pain was my pain. I eventually found myself thinking that
if I killed myself I could stop myself from sharing his pain. But I couldn't
kill myself because I knew my family would never forgive him. Then I realised
that if I was to drive my car into a tree no-one would know it was deliberate...[64]
2.56
The Vietnam Veterans' Federation of Australia asserted that the children
of Vietnam veterans 'have had a 300 per cent higher suicide rate than their
equivalents in the general community, a statistic resulting from veterans'
families becoming dysfunctional because of veteran fathers' war caused
psychological illnesses'.[65]
2.57
Recent research into suicidality in Australian Vietnam veterans and
their partners found that relative risks for suicidal ideation, planning, and
attempts were 6.2, 3.5 and 6.0 times higher for partners of Australian Vietnam veterans
compared with the Australian population.[66]
Significance and impact of mental ill-health
2.58
The committee received considerable evidence from individuals sharing
their experiences with mental ill-health and the enormous impact that it has
had on their career, families, and overall quality of life.[67]
Phoenix Australia outlined the enormity of the impact on the individual's
quality of life and on society more broadly:
A large body of data attests to the substantial functional
impairment and reduced quality of life associated with mental health diagnosis.
That is, these disorders substantially impair the person's ability to function
in social relationships, including with partners, children, friends, and other
loved ones. Rates of separation and divorce are high. Mental health disorders impair
the person's ability to function in their normal role (e.g., in employment,
study, or parenting).
...veterans with mental health problems showed higher rates of
unemployment, social dysfunction, martial separation, reduced engagement with
productive activity and poorer quality of life...The number of disability and
incapacity claims associated with mental health problems that are accepted by
DVA is further testament to the impairment associated with these conditions.
The human cost in terms of distress, poor quality of life,
family breakdown, and suicide, as well as the financial costs in terms of lost
productivity, health care, and benefits, are enormous.[68]
2.59
The significance of mental health on ADF members and veterans was also
highlighted by KCI Lawyers, which specialise in assisting veterans seeking
compensation, which noted that:
The significance of psychological conditions is substantial
given the effects on the Veterans' capacity to not only remain in the ADF, but
to function at a reasonable level within the Defence community and to coexist
harmoniously with their family, with their peers and friends. Their ability to
find and maintain civilian employment is also a major issue for those suffering
from PTSD.
Unlike a 'physical' injury that, at least can be explained
and the impact self-evident, PTSD is devastating to the individual with respect
to their self-esteem, motivation and outlook on life. A Veteran cannot simply
'explain' why they are unable to work, or spend large amounts of time in
relative isolation and medicated to treat and intangible condition. Their sense
of self-worth is degraded, their relationship with their spouses or partners
suffers, often irreparably, their confidence to deal with their families,
friends, peers and strangers gradually erodes.[69]
2.60
One submitter told the committee of their experience with PTSD and Depression
and its impact on their life following medical discharge for mental ill-health.
The individual told the committee of the profound impact that mental ill-health
has had on their relationships with family and friends and explained its impact
on their ability to live and function in society, highlighting the compounding
nature of the impacts of mental ill-health and their feelings of hopelessness
and despair:
You see when you suffer from mental illness you become like a
deer in headlights. Anxiety and stress sinks in and seemingly simple tasks
become complex and distressing.
At this time my relationship with my parents began to break
down. My behaviour was erratic and I also become involved in alcohol related
incidents in town. This is not good in a small country town and before things
got out of hand, I moved to my grandmother's house on the South Coast...unfortunately
my behaviour in civvy street had not improved...my time at my Grandmother’s had
deteriorated along the same lines as they had with my parents.
Poor behaviour and confrontations with friends and family
made my time there untenable. This was particularly distressing for me; as for
my entire life I’d had an extremely close relationship with my grandmother.
There was only one option and that was for me to leave. I had nowhere else to
go. I was burning bridges wherever I went leaving a trail of anger and
resentment. I had to be away from everyone for their sake and my own.
I was in a very dark place. I had very little money, I’d
ostracized myself from all my family and friends, I had no one to turn to. I’d
hit rock bottom. I literally went bush and went through the worst period of my
life. I hated everyone and I hated myself and I was just on my own having
nightmarish conversations with myself. I was broke, any claim outcome was at
least 3 more months away but it didn’t matter. I wasn’t going to make it.[70]
Committee view
2.61
The committee expresses its deep respect for those Australians who serve
and protect our country, putting their life, as well as their physical and mental
health, on the line. The committee commends Defence and DVA's ongoing
commitment to improve the understanding of the prevalence of mental ill-health
and the impact that ADF service can have on the mental health of its members
and veterans. The committee acknowledges the unique stressors of ADF service.
During their service, ADF members must manage various day-to-day stressors
including significant periods of time away from home, family, and friends in
addition to the increased risk of exposure to potentially traumatic experiences.
2.62
The committee notes the difficulty of clearly differentiating between
traumas experienced during ADF service and traumas experienced in ADF members'
private lives, and that for clear conclusions to be drawn regarding the impact
of ADF service 'traumas experienced during military service and in the private
lives of ADF members need to be separated'.[71]
To this end, the committee supports the Transition and Wellbeing Research
Programme and looks forward to the publication of its findings.
2.63
The committee also appreciates that mental ill-health in veterans will
often go unrecognised and undiagnosed many years after leaving the ADF. This
creates real challenges for policy makers and mental health practitioners who
are focusing on strategies for the early detection and treatment of mental
ill-health.
2.64
The committee understands that DVA is limited in its ability to measure
the prevalence of mental ill-health in veterans to those veterans who have
sought assistance or made a claim with DVA. The committee notes that the number
of veterans who have made claims may represent only a small proportion of those
veterans who have or are struggling with mental ill-health. The Transition and
Wellbeing Research Programme will provide invaluable data regarding the
prevalence of mental health in veterans as well as highlighting which areas
still need to be investigated.
Suicide
2.65
Since 2000, more than 100 ADF members are suspected or have been confirmed
to have died as a result of suicide. It is a terrible tragedy whenever any ADF
member loses their life during their service; however, when a member dies as a
result of suicide it is particularly devastating for the family, friends, and
colleagues of the deceased member.
2.66
A number of submissions called for the introduction of a government maintained
public record of ADF members and veterans who have died as a result of suicide.
The committee agrees that accurate data regarding the rate of suicide among ADF
members and veterans is an important element of addressing suicidality and
formulating policy to address it. The committee has carefully weighed the
arguments in favour of a public record of ADF members and veterans who have
died as a result of suicide against the risk to ADF members', veterans', and
their families' right to privacy. On balance, the committee is not in favour of
recommending the creation of a public record of ADF members and veterans who
have died as a result of suicide.
2.67
The committee is satisfied that current pathways for scrutinising the
deaths of ADF members, and (through civilian pathways) veterans, are adequate. Defence
currently records the death of members during their service, including those
suspected or confirmed to have died as a result of suicide. It is much more
difficult, however, to determine the number of veterans who have died as a
result of suicide. The committee notes that DVA has commissioned studies from
the Australian Institute of Health and Welfare and the Australian Institute for
Suicide Research and Prevention to investigate the prevalence of suicide among
veterans. The committee looks forward to the publication of its findings.
Navigation: Previous Page | Contents | Next Page