Chapter 8 - Inpatient and crisis services
One thing I came to understand clearly over these years of
dealing with and talking to the crisis teams and the staff of the mental health
centres is that the system is so under-resourced that they must deal with the
life and death cases first and other cases necessarily come second. This is a
brutal reality which should not exist in a civilised society.[747]
8.1
Mental health inpatient and crisis services are under
significant strain. Witnesses to the inquiry despaired at the absence of
treatment or other interventions in all but the most immediate life-threatening
situations. There was a clear call for increased resources to meet current
needs, to improve service availability and standards of care.
8.2
The committee received many harrowing personal stories
from consumers, carers and others about inpatient treatment experiences and
mental health crisis situations, in some instances leading to tragic deaths.
Many expressed their frustration and anger. Others expressed despair. Some
submitters had seldom told their stories before, feeling alienated and
stigmatised because of their circumstances. The committee appreciates the great
effort and courage they showed in giving evidence to this inquiry.
8.3
Other contributors had told their stories before, many
times. They commented that the same issues have been presented over and again
in different forums.[748] The committee
appreciates the determination these submitters show by continuing to contribute
their experience, knowledge and ideas to help improve mental health services
and ultimately the lives of those experiencing mental health problems.
Mental health care in an age of deinstitutionalisation
8.4
Care for people experiencing severe mental illness has
undergone a revolutionary transformation over the last few decades. Australia
had around 30,000 acute care psychiatric beds in the 1960s. The number of
public beds had fallen to around 8,000 at the time of the development of the
National Mental Health Strategy (NMHS), and is
now around 6,000.[749] This decline was
driven by several factors[750]:
-
Changes in views about human rights, treatment
and care for people experiencing mental illness
-
Improvements in treatment for mental illness,
particularly through new pharmaceuticals
-
Effective antibiotic treatment of syphilis,
avoiding the need for psychiatric hospitalisation in advanced cases of the
disease
-
Evolution of specialised aged care facilities
that could manage geriatric illnesses, particularly dementia
-
Creation of specialised institutions for people
with intellectual disabilities, and
-
Audits and reviews of stand-alone psychiatric
institutions that were highly critical of the care they provided.[751]
8.5
The closure of stand-alone psychiatric institutions is
often referred to as deinstitutionalisation.[752]
Figure 1 shows the change in beds over the last decade, and demonstrates two
key trends: the shift in beds from stand-alone facilities to general hospitals;
and the decline in the total number of beds, as more care takes place in the
community.
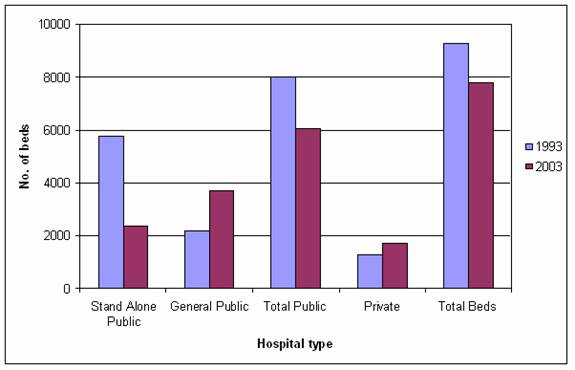
Figure 1: Number
of psychiatric hospital beds[753]
8.6
While deinstitutionalisation has meant closure of many
stand-alone psychiatric institutions, this closure has not happened in
isolation. It was meant to operate hand-in-hand with two parallel developments:
mainstreaming, involving the location
of acute psychiatric care facilities at general hospital sites; and the expansion of community care, ensuring
that people no longer in institutions have adequate care in their communities.
8.7
However, there is a general sense that mainstreaming
and community care have not kept up with the pace of deinstitutionalisation.
There are widespread problems with adequate accommodation, quality of care in
the new settings, and perhaps most clearly of all, problems for people in
gaining access to care in the new environment.[754] In this environment, it is not
surprising that the current policy direction is sometimes called into question.
The strong consensus that continues to exist around deinstitutionalisation may
be threatened if the policy is not fully and properly implemented and
community-based services significantly expanded. Much of the disenchantment
with the current system crystallises around experiences of acute care, but as
this report shows, the answer lies in improvements in every level of care and a
great deal more emphasis on community-based services than is currently the
case.
8.8
This chapter sets out the issues in relation to the
care people seek when acutely ill. People experiencing acute mental illness now
usually seek access to one of three types of service: hospital inpatient
services; emergency departments; or crisis assessment teams.
Inpatient services
Pressure on acute care places
8.9
Witnesses reported that unless a person experiencing
mental illness is considered to be a threat of immediate harm to themself or
others, there is little chance of their being admitted to hospital.[755] Some of the most devastating
evidence presented to the committee told the stories of those who knew they had
become unwell, had tried to seek hospital admission, been denied and
subsequently sought to harm themselves or others.
There were many instances of death or injury that were easily
attributed to not being admitted. A patient in Nepean
Hospital was placed on leave, while
trying to settle over the weekend, and on returning to the hospital unsettled,
to his promised bed found it had been filled. He went home and killed himself
and others in the family.[756]
One parent for example rang in saying her son had gone three
times to the local community mental health service and was repeatedly sent
away. The parents took him once and the Doctor on duty asked him if he was
going to kill himself. When he answered no the doctor said there was nothing
wrong with him and sent him away. He then drove his car through the hospital
front doors and was subsequently admitted for three days.[757]
8.10
A number of state government submissions to the inquiry
acknowledged the pressure on inpatient mental health services. The Victorian
Government stated:
In Victoria,
the current operating environment is one of sustained demand pressure. There
are a number of inter-related issues that place pressure on the mental health
system including growing demand, and increases in complex and involuntary
clients. Their impact is most evident in two key aspects of the hospital
system: adult acute beds and hospital emergency departments.
Client growth of more than 7 per cent per annum over five years
has led to services operating over capacity, as evidenced by high community
caseloads and chronic acute bed blockages, with 9.6 per cent of patients
staying more than 35 days. This has resulted in crisis driven services
responses, difficulties with service and bed access, 'revolving door' clients
(15 per cent each year) and a significant impact on other social policy areas.[758]
8.11
In New South Wales:
The level of psychiatric distress and disability in the
community is rising. Reasons for this change are poorly understood but may
include broad social changes, changes in social supports and social capital,
increasing inequality, and changes in patterns of drug use. Available resources
have not kept up with increased demand. Across Australia
there are problems with access to acute care, continuity of care and the availability
of coordinated and comprehensive community support. A time lag exists between
recognition of increased demand and construction and commissioning of new units
and the development and implementation of community based programs.[759]
8.12
This analysis is supported by other reviews of mental
health services, such as the Not for Service
report,[760] the South Australian
Legislative Council inquiry,[761] and
the Western Australian Legislative Council inquiry.[762]
The impact of acute bed shortages
8.13
Denying admission can result in ongoing hardship for
consumers and their carers. Consumers have in some cases been abandoned to a
cycle of homelessness and abuse. The costs of not providing treatment and care
when sought, both in terms of quality of life and later need for services, is
significant.
8.14
Early discharge from hospital places a significant strain
on families, which in turn creates a need for services:
Discharge from hospital is frequently too soon because of the
pressure for beds and carers assume responsibility for the consumer in a state
of unwellness. Programs are needed to provide support, information and skills
development to enable carers to cope in this kind of situation.[763]
8.15
Individual submissions from carers demonstrated
ARAFMI's concern:
Severe shortage of hospital beds...results in clients not being
admitted to hospital when there is a real need, or being sent home too soon,
with no other options. I have been called on the day my son is to be
discharged, and without prior warning, been told that I am to come and collect
him. When I have show reservations because I felt that he was not well enough,
and that I couldn't ensure his safety, I have been given the only other option
of having him sent to a homeless men's shelter...[764]
8.16
Carers illustrated the significant cost incurred when
patients 'recycle' through the hospital system:
After being put into hospital, my daughter with schizophrenia
was given medication for a few weeks and released, despite the family all
pleading with the hospital to keep her a bit longer as it was quite clear to us
this medication was not reducing her psychosis. In fact she had to be taken
back to the hospital within a week. She was put on another medication and
stayed in hospital a while. Then, again, despite still having intense psychotic
episodes she was let out – despite our huge concern. Off the record hospital staff
told me the reason she was let out was due to a shortage of beds! She had to be
re-admitted for the third time around August.[765]
My son was increasingly unwell for three months. When I asked
for help because of the case workers heavy work load they said he wasn't ill
enough.
At the end of the three months he was hospitalized six times in
two months.
He was discharged TOO early everytime because there were 25 beds
for up to 600 patients. He suffered unnecessarily and stress on the family was
enormous.[766]
The causes of acute bed shortages
8.17
The lack of acute beds has several interrelated causes.
While insufficient bed numbers was one factor raised, inadequate
community-based facilities appeared to be the central issue. Without
intervention programs and accessible community treatment, assistance and
support, the symptoms of mental illness can escalate, leading to acute episodes
and increased demand for inpatient services.
8.18
Following episodes of inpatient care, a lack of 'step
down' rehabilitation services and community supports can make discharge
difficult, resulting in longer inpatient stays than necessary. Consequently,
patients whose needs could be catered for in a less restrictive community
environment are retained in hospital, 'blocking' bed availability for new patients.
In other cases a combination of insufficient inpatient beds and inadequate
community facilities means that patients are discharged too early into
inadequate circumstances.
8.19
The NSW Nurses' Association reported that premature
discharge was the most common response to pressure for acute beds. A survey of
their members in 2004 found that:
Prematurely discharging patients was the number one way of
dealing with the problem, with 29 per cent indicating this method. Next highest
scoring method was keeping them in emergency departments (23 per cent) or
general wards (6 per cent), refrain from admitting them (13 per cent), manage
them in the community (11 per cent), or transfer them around the state (8 per
cent). About 8 per cent also indicated they routinely had mental health
patients sleeping on couches or on mattresses on the floor.[767]
8.20
Dr Morris,
Executive Director of the Gold Coast Institute of Mental Health, expressed the
view that state mental health acts were being misapplied in order to deny
admissions, due to the shortage of acute psychiatric beds.[768]
8.21
Several states acknowledged that some admitted patients
could be better served within the community, if adequate supports existed. In Queensland:
A recent snapshot of mental health inpatient beds conducted in December
2004 indicated that 30 percent of patients did not need hospitalisation if
other options were available. Similar pictures occurred across most
jurisdictions which participated in the exercise. Difficulty in accessing
suitable support and accommodation was the key factor preventing discharge.
This represents substantial numbers of patients accommodated in inpatient care,
effectively blocking throughput and being accommodated, often at acute bed day
costs, placing further pressure on systems already operating at maximum level
and with finite resources.[769]
8.22
In South Australia:
The Homeless and Housing Taskforce of the Australian Health
Ministers’ Advisory Council (AHMAC) draft report titled Australian Mental
Health Inpatient Snapshot Survey 2004 indicates that there were 505 patients in
10 mental health inpatient units on Census day in SA for whom immediate
discharge would have been possible if more intermediate treatment, rehabilitation
support and accommodation services were available in SA.[770]
8.23
In Western Australia:
The key findings from the 2004 national survey are consistent
with the earlier two state surveys and include:
- 53
per cent of patients could have been discharged if appropriate alternative
services were available and, of these
patients, 56 per cent required both appropriate intermediate
treatment/rehabilitation, support and
accommodation services.
- 51
per cent could have been discharged if appropriate support and accommodation
services were available.[771]
Responses
to acute bed shortages
8.24
There was a strong call from witnesses for additional
acute care places, to respond to current shortages. However the Committee's evidence strongly
suggested that the key cause of acute bed shortages is the lack of appropriate
emergency responses; a rehabilitative focus in acute care; interventions at
other levels, particularly step up and step down and respite beds; clinical
services in the community; and housing and employment supports. Each of these
needs strengthening and expanding to reduce the need for acute care over the
longer term. The Australian Mental Health Consumer Network recommended:
That the call for
‘more acute beds’ be understood in relation to the lack of
alternative modes of service delivery.[772]
8.25
Dr Freidin,
President of the Royal Australian and New Zealand College of Psychiatrists
said:
Increasing the number of hospital beds is not the sole answer
either. We need to have an adequate number of outpatient and community services
across the public and private sectors and these need to be integrated with all
other forms of support. We say that most mental illness is treatable, as
demonstrated by the increasing body of evidence. The inability of people with
mental illness to get appropriate help is one of the main barriers to the
provision of treatment. The treatments are available—it is just that the
service system does not deliver them.[773]
8.26
Ms Sheelah
Egan said:
... one hears calls for more beds instead of calls for much better
treatment in the community and more appropriate accommodation in the community.
Inpatient services are expensive, but could be minimised if sufficient
resources were put into the more efficient and cheaper community care.
(Unfortunately, in the past, community care has been treated as a cheap option.
Good community care is not cheap, but it is cheaper, for obvious reasons, than
inpatient care.)[774]
8.27
The Mental Health Council of Australia acknowledged
recent mental health funding increases announced by the Australian Government,
but commented:
...the next step is the most important: to use this funding to
build and strengthen the community based primary and secondary care systems
which will then take the pressure off the acute and crisis care services.[775]
8.28
The Council submitted that funding for acute care
should be limited to 25 per cent of any new funding.
8.29
All state and
territory governments' submissions stated that their budgets included funding
to improve inpatient services in coming years. In some jurisdictions this
funding related directly to inpatient services, in others it related to increased
'step down' facilities, supported accommodation and intensive community support
which would relieve pressure on inpatient services.[776]
8.30
In the short term, one strategy being used to lessen
pressure on acute care places is increased collaboration between the public and
private sectors. The Victorian Government commented:
Where public mental health services are operating at capacity,
it should be possible to make arrangements to use private mental health
services. For example, Victoria
has purchased acute inpatient beds from private mental health services to
manage periods of bed shortage.[777]
8.31
Healthscope Ltd saw opportunities to increase
collaboration between the sectors:
Although the private sector is primarily committed to providing
psychiatric services to privately insured patients, the private sector’s
ability to increase its capacity could be utilised to improve access during
periods of bed block. This could be achieved in a number ways:
-
Temporary
placement of patients requiring acute admission until a public bed becomes
available
-
Decanting of more
stable patients into the private sector as a mechanism of freeing up more acute
beds
-
Temporary
purchase of beds pending capital works
The basic economics of this solution
is compelling. A patient cared for in the Emergency Department for 24 hours by
an agency nurse will cost $1500 per day, when a bed could be purchased in the
private sector for approximately $500 per day.[778]
8.32
The committee supports innovative practices and
collaboration between sectors to respond to the pressure on acute inpatient
mental health services. However, investment in community-based care is required
to provide earlier interventions and in the longer term reduce the need for
acute services. The committee notes that in Trieste,
where there is strong community care infrastructure, it is rare for all the
psychiatric beds in the general hospital to be occupied (see Appendix 3).
8.33
Expansion of community services is not simply an issue
of cost effectiveness. It recognises the need to increase people's experiences
of mental health and where possible reduce the severity of illness experiences.
Rather than investing only in responses to acute episodes of illness, resources
are required to, wherever possible, prevent people's mental health
deteriorating to a situation requiring acute care. Following acute phases of
illness, adequate rehabilitation and support services are required to help
promote stability and wellbeing, and minimise the need for readmission.
Long stay care
8.34
While much of the evidence presented to the committee
about inpatient services concerned the pressures on short-term acute beds,
submissions also canvassed the issue of long-term care for the relatively small
number of people who are severely and chronically disabled by mental illness.[779] Witnesses observed that keeping
long-stay patients in hospital, because of a lack of alternative services, only
contributed to the strain on acute care places.
8.35
In 1992, the National Mental Health Policy recognised
that long-term care would be required for some consumers:
It is recognised that too much resource emphasis is currently
given to separate psychiatric hospitals. In some cases it may be both possible
and desirable to close them and replace them with a mix of general hospitals,
residential, community treatment and community supported services. However, a
small number of people, whose disorder is severe, unremitting and disabling,
will continue to require care in separate inpatient psychiatric facilities and
these facilities will need to be maintained or upgraded to meet acceptable
standards.[780]
8.36
However, the committee was told the NMHS has failed to
make appropriate provision for the care of these consumers.[781] Dr
Simon Byrne
outlined the kinds of services needed for chronically disabled consumers:
...it is possible to foster and develop long-stay wards with a
rehabilitation focus. Such services should be co-located with acute hospital
wards, partly because of the economies of scale involved in providing the
necessary support services and partly because of the need to rotate staff for
training purposes and to maintain morale when working with a very challenging
group of patients. The long stay services should have a rehabilitation focus
and have continuing active links with a variety of community services including
community residential services; thus all patients should be regarded as
potential candidates for community living, although the work necessary to
achieve this may take very long periods of time and may not always be
successful.[782]
8.37
Dr Philip
Morris outlined a similar approach:
We are suggesting that we need a substantial build of supported
accommodation. This is not accommodation where someone pops in to see a patient
once a day or whatever else. This is accommodation that has 24-hour nursing and
an appropriate level of support—medical, nursing, occupational therapy and
social worker support for patients. If you start doing that, you are getting
back to needing clusters of homes. They can be in the community, but they need
to be together. You will need to have them together because you cannot have
individual services going out because it is not efficient. We will get to
something like having properly based facilities that look different to the old
mental hospitals but, nonetheless, the services will be brought back to bear in
a sophisticated and specialised way. That will take some time. That is where we
need to go and that is the glaring omission at the moment: the longer stay
accommodation for people who cannot get back to independent care in the
community.[783]
8.38
While some submitters vehemently criticised the
implementation of deinstitutionalisation,[784]
a return to institutional-based care was not generally considered an
appropriate or advisable course for patients requiring long-term care.
Witnesses pointed to the stigma, isolation and lack of resources associated
with institutional care in the past.[785]
Reports have highlighted the abusive practices, discriminatory cultures and
lack of accountability which occurred in psychiatric institutions. Rather,
witnesses to this inquiry described the need for specialised community-based or
co-located services designed specifically for the long-term rehabilitation of
people severely disabled by mental illness.
Quality and effectiveness of
treatment
8.39
The committee received some graphic and alarming
evidence about inpatient treatment experiences. Assault and abuse of people
with mental illnesses still occurs within hospital settings. Discriminatory and
stigmatising attitudes and procedures remain.
8.40
The committee acknowledges that this inquiry has not
systematically reviewed all inpatient experiences and that some positive
experiences were also reported.[786]
However, the committee is disturbed that after many years of reform, abusive
and discriminatory practices remain evident. The following contributions
reflect some such experiences:
Another occasion was when the young man's mother and brother
visited him and he asked his brother to look at his room. They reached the room
to find a large 6ft male lying on his bed. The patient got a shock and was
clearly disoriented and went to another room and kicked some blocks around. A
nurse brought him back to his room and he appeared very frightened when the
nurse ordered a syringe. His brother asked what it was and was told that it was
"like liquid valium". A
doctor and two security men stood over him either side of his bed. Staff asked
the mother and brother to leave the room but they chose to stay and in front of
those people the patient's pants were pulled down and he went into a foetal position
because it was invasive and he was scared, as he had been a victim of rape. The
inhumane treatment raises the question of how and what was being done when no
family member was present. The patient was then told he could go and have
lunch. He left crying.[787]
......
Seclusion and restraint are used inappropriately and without
proper regard to the person. A client of our service was stripped naked and
thrown in seclusion for 12 hours when she had a known history as a victim of
sexual abuse. Clients report experiences of seclusion, terrified and left alone
for long periods of time with frightening psychotic symptoms. Seclusion is used
far more on weekends when no programs are
available.[788]
......
Instead the two security guards who arrived jumped me, threw me
to the ground and proceeded to beat the living daylights out of me. I was
repeatedly punched to the left eyebrow and as I wear an eyebrow ring, punching
the metal onto bone was exceedingly painful. I was repeatedly punched to the
right cheek bone. One of the guards twisted my elbow as far as it could be and
then brought his fist down onto my elbow with maximum force. This was done
several times. Both guards also bent my hands back at the wrist as far
backwards as they would go. I thought they were going to break them. I was
kicked in the base of the spine several times...I was kicked in the legs repeatedly.
I was punched in the chest and stomach repeatedly. One of the guards grabbed my
hair and drove my face forward into the ground, hurting my nose. He then pulled
my hair back the other way and repeatedly smashed the back of my head into the
hard, vinyl floor.
Throughout the attack I continued to scream and struggle, but
this was because I was in extreme agony. One of the guards put his hand around
my throat and squeezed to the point no air could enter or leave for at least a
minute. I was sure at that moment he was going to kill me. I could barely speak
for days afterwards.
The actual nursing and medical care I received ... was outstanding
so I have no idea why these nurses let the attack go on so long, although one
of the guards did lean over me at one point and whispered into my ear, “the
nurse can’t see what I’m doing from here and you’re fucking dead meat”. He also
laughed and smiled throughout the attack – he was clearly enjoying himself.[789]
......
On arrival [in the 'time out room'] I was ordered to strip all
clothes off. The situation was getting more and more bazaar [sic]. I thought I
was in hospital because I was sick and needed care. Is this the care that I
needed?
I told him "you've got to be joking".
He disappeared for a few minutes and came back with five other
nurses. They stripped me naked and put me into pyjamas. I can still see a big
guy with tattoos smiling all through the whole thing.
At no point did I abuse anybody or become violent. Why was I
getting such heavy-handed treatment when I don't think I deserved it.
After the nurse in charge pushed me into the back of the room
they locked the door and turned off the light. There was only a mattress on the
floor and the only window was in the locked door. If you have any iota about
psychosis you could imagine what was going through my head.[790]
8.41
Ms Isabell
Collins, Director of The Victorian Mental
Illness Awareness Council asserted
that damaging treatment experiences are common:
Having worked in the
public mental health care system for some 15 years, I am yet to meet a patient
of mental health who has not been damaged by the way he or she was treated and cared
for. Indeed, consumers will often say that it takes a good 12 months to recover
from hospitalisation just because of the way they were treated.[791]
Put simply, the current standard of practice is to contain
people with medication and then discharge them. That is all we do.[792]
8.42
Consumer
researcher Ms Cath Roper said:
I had 13 hospitalisations—all
of which were involuntary—yet I cannot look back and say that those were
healthy for me. There was extremely traumatic forced treatment involved in each
of those hospitalisations.[793]
8.43
The
Australian Mental Health Consumer Network recommended:
That government takes
seriously the consumer warning that some acute experiences leave people
psychologically scarred, sicker and more dependent in the long term.[794]
8.44
There have been some reviews of inpatient services and
changes that have been implemented to improve service standards.[795] The committee also heard the reality
of the complex situations hospital staff are required to deal with. For
example:
When he was again admitted to Maroondah Hospital psych ward my
son had a 3 week old untreated fractured leg gained after clinging onto and
being thrown from a car; he was taken to William Englis hospital emergency ward
after the incident but would not remain stationary for long enough for the cast
to be applied. There were several prior attempts seeking admission over
preceding months mainly due to violent and abusive behaviour.
During this stay in Maroondah hospital my son broke another
patients arm.[796]
8.45
Humane and professional responses are needed in what
can be complex and difficult situations. The personal experiences shared with
the committee show that in some areas inpatient service standards need to
improve.
8.46
Mr Graeme
Bond submitted that quality standards are
required:
When investigating my son’s treatment I sought to compare it
with any standards I could locate. I was able to locate very few publicly
accessible standards published by the Department of Human Services and resorted
to statements made by leading academic psychiatrists in a locally published textbook
of psychiatry.
There should be a comprehensive set of standards readily
accessible to carers and patients so that they can assess the care given
against an objective benchmark. Such standards should be the reference against
which actions of clinicians and services are judged, particularly in such forums
as the Coroners court.[797]
8.47
Observations by the Victorian Auditor-General are
pertinent:
The current set of mental health measures and key performance
indicators (KPIs) do not provide sufficient information to management and the
Government to measure the effectiveness of the services being delivered. Most
of the current measures and KPIs are not tied to departmental objectives and
relate to service delivery (i.e. outputs) rather than consumer outcomes.[798]
8.48
Acute care in hospitals needs to be guided by standards
of care that are focused on consumer outcomes, and which take a view beyond the
points of admission and discharge. This is important because issues raised with
the committee extended beyond acute care to the emergency departments where
admission took place and to discharge.
Emergency departments
8.49
While hospital emergency departments are one of the few
health services available to people with a mental illness on a 24 hour basis,
seven days a week, the environment is not necessarily therapeutic and treatment
may not eventuate. The NSW Nurses' Association commented that it was not
uncommon for mental health patients to wait in the emergency department for up
to five days before a suitable bed became available.[799]
8.50
The ARAFMI National Council Inc described the detrimental
impact of waiting in emergency departments:
The consequence can be that the consumer becomes acutely unwell
needing emergency treatment possibly though a hospital emergency service. If it
is then accepted that the consumer needs psychiatric care in a psychiatric
facility there are frequently no beds available and the consumer is kept in a
"holding" situation pending a bed becoming available, This is not
only detrimental to the consumer but also causes distress and anxiety to the
carer.[800]
8.51
Mrs Jan
Kealton described the void in emergency
departments services for psychiatric patients:
Once there you wait and wait and eventually you might get lucky.
... They take the person through to the triage area and tell them to sit in one
of the blue chairs. The chairs are near the reception area, and then there are
all the beds with curtains around them and so on. If you are a bit forceful,
like me, you say, ‘Excuse me, but I am going too,’ and then you, the mother,
are also allowed to sit on one of the blue chairs.
The blue chair is not in the treatment area and it is not in the
triage area, so you just hope that someone notices the person if they are
becoming distressed. You can walk straight out the door—if you do not have your
mother with you being nice to you and begging you and bribing you to stay—and
not get any treatment at all. Nobody would probably even notice. They are too
busy handling all the blood and gore, the heart attacks and those sorts of
things to go to somebody who looks perfectly normal, sitting there fidgeting ...
We have sat there for seven hours on a number of occasions...[801]
8.52
The NSW Nurses' Association described the hectic
environment of hospital emergency departments. They noted that it is not
possible in this environment to establish rapport with patients and initiate
preventative interventions. The Nurses' Association also pointed out that the
'excessive stimulus generated by the chaos and pressured atmosphere in the
department' itself can contribute to escalating behaviour. They stated:
Given that security personnel are engaged to provide supervision
for such volatile patients, it is clear that restraint and sedation are the
likely and foreseeable outcomes... This is an untenable situation for all
concerned.[802]
8.53
The committee heard that people with acute mental
illnesses are particularly vulnerable to breaches of their privacy and dignity
within the emergency department environment. Dr Georgina Phillips said:
Their ED management is usually
carried out in a high acuity, highly visible cubicle in the central part of an ED
work area (so that medical and nursing staff can closely monitor them). Many in
the ED usually overhear their conversations:
staff, security officers, other patients and their relatives. Many observe their
appearance and behaviour, and if containment and restraint is required then
this is usually carried out in full view of the rest of the ED.
This affects not only the mentally ill patient, but can cause distress and
potential physical harm to other patients or relatives in the ED.
These are daily occurrences in EDs, however few would have space or resources
to devise appropriate strategies to provide better and safer care.[803]
8.54
A report by the South Australian Ombudsman points to
some of the underlying resource issues creating strain on emergency
departments:
It appears that neither the existing mental health system or
supporting resources were sufficient to accommodate the significant changes
undertaken in this State, in line with the National Mental Health Strategy...
Moreover, there was overwhelming evidence during my inquiry from medical
practitioners and others that there has been a significant increase in numbers
of mental health patients presenting at emergency departments. This clearly,
has placed undue strain on junior medical and nursing staff who are left to
manage the increasing numbers of patients in crisis in emergency departments.
A common consumer and staff concern was the need to provide a
safe and stable environment for mental health patients in crisis and in the
community. It was apparent that in most emergency department environments staff
face difficulties in separating highly agitated patients and there is an
abundance of evidence that has shown that enormous pressure has been created at
times when there has been an acute shortage of available beds in psychiatric
wards and on discharge for either the emergency department or an inpatient
facility, with a distinct lack of support in the community.[804]
8.55
Several submitters recommended specialised emergency
departments for people experiencing mental illness.[805] Dr
Philip Morris
told the committee:
...patients that have been sent to emergency departments do not
get the best of care because the facilities are not providing unique services
for patients with mental illness. What we advocate now is a parallel—not a
separate but a parallel—program of emergency departments located in the setting
of the general health sector for patients with psychiatric illness. Some of
these things are now starting to happen in Australia.[806]
8.56
The New South Wales Government described a trial of
such services:
Psychiatric Emergency Care Centres (PECCs) have been
successfully trialled at Liverpool and Nepean
Hospitals. These PECCs have
resulted in a reduction of the average length of stay in Emergency Departments
for psychiatric patients. The PECCs are dedicated services, situated adjacent
to the Emergency Department, staffed 24 hours a day, 7 days a week by mental
health specialists for emergency assessment and treatment of people presenting
with serious mental illnesses.[807]
Discharge processes
8.57
Discharge from hospital can be as abrupt as admission
can be slow. Submitters told the committee about a lack of discharge planning
and continuity of care after discharge from hospital or the emergency
department. Poor discharge planning and insufficient community-based services
can leave consumers in inadequate environments without appropriate therapeutic
care, resulting in increased symptoms and possibly re-admission. Following an
acute episode of illness, the risk of suicide is highest in the first weeks
after discharge.[808] Where families
and carers are contacted and available, early discharge increases their burden
in providing care and support.
8.58
Dr Philip
Morris said:
Because of the pressure on bed numbers, patients are being
discharged before they are ready to go home. That leads to harm both to them
and to their families and the general public. If we had more resources,
patients could stay in hospital for longer and be treated to a point where they
were much more ready to be discharged. I am not just talking about discharge
from acute services. There is no opportunity at the moment to put many patients
into longer term facilities where they can be rehabilitated and recover further
so they can then go back into the community in a decent state.[809]
8.59
Dr Morris
also suggested there is evidence that some practitioners are having patients
placed under involuntary treatment orders as the only way to obtain follow up
treatment in the community after discharge.[810]
8.60
Mr David
Webb shared his discharge experiences with
the committee:
On the strength of that assessment, the psychiatrist judged that
I suffered from what he called existential depression and that I did not need
to be there. I had attempted suicide just a couple of nights before. He told
the social worker and the charge nurse to arrange for my discharge. That was
it. The psychiatrist spoke to me about where I would go on discharge and
whether I had somewhere to go. I did not have a place to go as I did not have a
home in Melbourne at the time. He spoke to the social worker and said, ‘Help
him find somewhere to go.’ I left that hospital with the phone number for the
emergency accommodation of the Salvation Army. That was the discharge support
that I got a couple of days after a suicide attempt. People tell me that would
not happen these days, but I am not sure. I am one of the fortunate ones. There
are a lot of people that have been through that experience and they have gone
straight to the nearest railway line to jump under the first train.[811]
8.61
Carer's also described the lack of services post
discharge:
Another issue in regard to the post acute-care situation is that
in the case of our son’s first psychosis, I had to initiate post-hospital case
work. No-one offered me access to services. I had to seek these out and despite
my best efforts to have a case worker assigned while our son was still in
hospital to facilitate a smooth transition on his discharge, it proved a
fruitless exercise. I knew nothing about mental health services and no-one
offered me any help or information. It concerned me enormously that if our son
had not had an active advocate in me, then he would have been discharged, unwell,
and having to fend for himself, with no accommodation and with no knowledge or
ability to access social welfare let alone any mental health services (as inadequate
as these turned out to be).[812]
8.62
Ms Isabell
Collins commented on the ethical dilemmas
facing staff who make discharge decisions:
Certainly psychiatrists have said to me that they are constantly
in this ethical dilemma where they have somebody who is really sick and needs
admission to hospital and they have somebody in hospital who is still sick but
not as sick as the one who needs to come in. They have to juggle and take these
risks. What happens is that they do take the risk. They send them out into the
community where there are no supports for them.[813]
8.63
Reviews of service standards indicate that the personal
anecdotes shared with the committee are illustrative of systemic failures. A
file audit by the Auditor-General in Victoria in 2002 found that 89 per cent of
consumers reported that they were discharged while still acutely unwell, with a
high level of need for ongoing support. Yet none of the discharge plans
reviewed met all required standards.[814]
8.64
Among the disturbing findings, the Auditor General
reported:
-
30 per cent of discharge plans reviewed showed
no evidence that consumers had been linked into appropriate community-based
services for ongoing treatment following discharge;
-
In 80 per cent of cases there was no evidence
that consumers were consulted in the formulation of the discharge plan. Family
or carers collaborated in discharge planning in only 15 per cent of reviewed
cases;
-
In only 16 per cent of the reviewed plans was
the consumer given emergency contact numbers; and
-
In only one per cent of cases reviewed was a
copy of the discharge plan actually provided to the consumer.[815]
8.65
Even where services specifically focus on discharge
planning with dedicated resources, evidence suggests that actual follow up remains
limited. A study of the emergency department of a Sydney hospital, which has a
dedicated Mental Health Liaison Nurse, found that 86 per cent of consumers felt
that adequate arrangements had been made with them before they left emergency
and 71 per cent were referred to a community mental health team on discharge.
However, only 63 per cent actually had contact with the community mental health
team after leaving emergency.[816]
8.66
The committee suspects that the lack of discharge
planning and support, at least in some cases, reflects the fact that acute
service providers know there is nowhere for the person to go. The Mental Health
Council of Australia submitted:
Consumers are often discharged without any rehabilitation plan
or even reference to appropriate places because the discharging services knows
these services have no capacity to accept further referrals.[817]
8.67
This situation reinforces the concern, expressed
throughout this report, that the mental health sector in Australia
currently lacks a full spectrum of care.
8.68
One possible consequence of inadequate discharge
planning, follow up treatment and care is the deterioration of a person's
mental health, which results in readmission. This is an unsatisfactory
situation for all involved, with consumers carrying an increased burden of
illness, carers suffering increased strain, and services sustaining repeated
costs. Even in Victoria,
a state with above average investment in mental health services and one of the
highest per capita investments in community-based care,[818] readmission rates remain high. In
2005 the Victorian Auditor-General reported that although initiatives had been
implemented since 2002 to increase community-based care, and more patients were
being contacted in the community before and after admission for acute care, an
increasing proportion of patients were being readmitted within 28 days of
discharge.[819] In the June
quarter 2005, 17 per cent of mental health patients were readmitted within 28
days of discharge.
8.69
This level of readmission suggests that community
supports remain inadequate to stabilise and support people with a mental
illness following acute episodes. However, the data might also suggest that at
least hospitals remain an accessible service for people requiring further care,
with people being readmitted rather than turned away.
Crisis services
8.70
Crisis services refer to services designed to respond
to mental illness related emergencies in community settings. Such services can
save lives and are particularly valued by carers. Crisis assistance needs to be
timely to be effective, and achieving prompt crisis response is a challenge
facing these services, which appear to be constrained by resources as well as
perceived safety issues.
8.71
A key issue regarding crisis services is the need for
services to attend and assist crisis situations out of business hours. Ms
Sharon Ponder
remarked on this need:
Apparently acute episodes of schizophrenia occur at the most
"inconvenient" times for our system, It needs to be told that an
acute schizophrenic episode is rarely "convenient" for the sufferer,
never mind the system.[820]
8.72
The lack of after hours mental health services means
that hospital emergency departments and emergency services (police and
ambulance) are often the only available services out of business hours. These
services are not necessarily trained or equipped to deal with mental illness
crises, and can create further distress for people experiencing mental illness:
The response from the mental health services to after hours
crisis is that the refuge phone an ambulance to take the young person to
accident and emergency or call the police, this of course creates a scene in
front of other young people and neighbours, not to mention the trauma for the
young person involved.[821]
8.73
In some areas, after hours phone calls to psychiatric
units are simply referred to Lifeline.[822]
Lifeline commented that its services are over stretched:
Lifeline...has become a defacto after hours mental health service
with volunteers answering call after call from people with a mental illness
that have been referred to Lifeline from other mental health services unable to
cope with high levels of demand. Lifeline is not adequately equipped, resourced
or developed to fulfil this role appropriately. Many of our traditional crisis
callers have not been able to access our service because of the dominant usage
of some mental health callers. With over half a million calls per annum being
answered by Lifeline volunteer telephone counsellors it is clear that this is a
significant community problem.[823]
8.74
Lack of services after hours for people experiencing
acute mental illness therefore impacts not only on mental health consumers and
their carers, but also on wider service providers and their clients.
Crisis assessment and treatment
teams
8.75
One service designed specifically to assess and
intervene during episodes of mental illness are mobile acute assessment and
treatment teams. These teams are 'medical health services which provide
home-based assessment, treatment or intervention primarily for people experiencing
an acute psychiatric episode and who, in the absence of home-based care, would
be at risk of admission to a psychiatric inpatient service'.[824] The services are known by different
titles across jurisdictions, including 'psychiatric crisis intervention' services,
'community assessment and treatment' services and 'crisis assessment and
treatment' (CAT) services.[825]
8.76
The National
Mental Health Report 2005 describes the essential characteristics of these
services as their 24 hour, 7 day per week availability and focus on short-term
intervention. However, carers lamented how often they were unable to obtain
assistance in crisis situations. Several submissions commented that the poor
response record of the Crisis Assessment and Treatment teams had earned them
the nicknames 'Can't Attend Today' teams or 'Call Again Tomorrow' teams.[826] If the CAT teams are to be effective
and supported by consumers and carers there is a need for better resources and
training.
8.77
One submitter described the frustration of the lack of
service, as follows:
...if they are contacted it means that the client or family, or
both, needs some help. Instead, you often get this indifferent response, trying
to get you to go away as your crisis doesn't fit their criteria. I have even
been told that I couldn't be helped because they were too busy with other more
urgent matters. This was before I was even listened to...In fact, they have never
made a trip for us. The only times I have received help was if my son could be
calmed down enough to let me drive him to hospital. If all else failed, I had
to call an ambulance.[827]
8.78
Mr Graeme
Bond reported his experience with the CAT
team:
Even when I have called reporting the most alarming behaviour
which posed a threat to my wife or, on occasions to me, I have been unable to
have a CAT Team attend. Indeed, in my area, I believe that after about 7:00pm the CAT Team is one person accessible by
a paging service.
The standard advice offered, in response to a request for a CAT
Team, is 'call an ambulance' or 'call the police'.[828]
8.79
The Victorian Mental Illness Awareness Council
presented strong criticism of CAT services:
Crisis Assessment and Treatment teams (CATT)
are probably the best example of what happens when governments fail to
adequately fund services.
From the consumer perspective CATT would be the
most disliked and criticised service in mental health.[829]
8.80
However, the CAT team model is effective when
adequately resourced:
Whilst living in the ACT, we experienced excellence from the
local CATT which attended our home when our daughter was in a
prodromal state and had locked herself in her room late at night. As a result
of the CATT dedication, a humiliating and extremely
distressing family situation was brought under control without need for
hospitalization or the stigma of well-meaning but untrained police presence in
our neighbours' presence.[830]
8.81
Even with well resourced prevention and intervention
programs, the severe and episodic nature of some mental illnesses means that
crisis situations can occur. Without ready access to personnel adequately
trained and experienced in intervention and de-escalation, crisis situations
can end in tragedy:
I have just been involved in a coroner’s inquest. A young
23-year-old man had been shot dead by the police. He had an agreement with his
parents, before becoming unwell, that should he become unwell they would ring
the CAT team. He became very unwell and that was not the case. He had knives
and he hurt his father. The location was secured and his mother was terrified
her son would be shot. She told the police: ‘He is all right. He will be able
to talk. Please be careful of him.’ The police did everything in their
endeavours to get the CAT team. The duty person for the CAT team on the evening
of that night, when the police called, did not perceive that they were being
asked for assistance. They gave the response: ‘Yes, this person has been in
this hospital. Yes, this person does have a diagnosis of schizophrenia.’ But
they did not then go on to say, ‘And this person, in fact, has asked before to
be killed.’ So the police, acting as they believed they should, managed this
situation. Something really unfortunate occurred: the young man appeared behind
the house and came at a police officer with knives and the consequence was he
was shot.
At the coroner’s inquest, the CAT team thought that the
provision of the information I have just provided to you was enough to give
instructions to the police in how to take control of the situation and the
young man. The police do not have effective training in de-escalation; their
training is in control, not de-escalation. My submission is that when you have
the police ineffectively prepared, and when you have the CAT team not
perceiving that they need to attend and, further, saying that they would not
attend if their health and safety were in danger, then even if the police could
make their health and safety secure we either have to do something about the
function of the CAT teams or do something about the education of the police.[831]
8.82
As illustrated it the above example, coordination
between crisis teams and the police is essential in responding to crisis
situations involving mental health consumers. The role of police in mental
health services is discussed further in Chapter 13.
8.83
There is a need to ensure effective responses for
people with mental illnesses requiring emergency attention. CAT teams currently
have limited availability and are concerned about attending potentially violent
situations. Emergency departments, while always open, are stretched and do not
necessarily provide an environment or interventions appropriate for acute
mental illness. Similarly, while emergency services such as police and
ambulance will attend mental illness crisis situations, they are not trained to
respond effectively to psychotic episodes and their presence can escalate the
situation.
8.84
One of the NSW Government's initiatives is to improve
emergency mental health responses is the establishment of a 24-hour 1800 phone
number for each NSW Area Health Service.[832]
It was not clear from the NSW Government's submission the extent of the
services that would be offered via this phone line. However, a single 24 hour
access point for mental health emergencies may assist carers and consumers who
currently report a desperate need for assistance. The Council of Australian
Governments' proposed National Health Call Centre Network[833] may help meet this need, if
adequately resourced to include dedicated mental health professionals and
backed up by available intervention and treatment services.
8.85
Two points stand out in discussion of crisis services
for mental health. First, the very nature of mental health crises often means
that it is quite inappropriate for police or ambulance to respond. Mental
health crises need a mental health response. Being told to 'call the police' in
particular often seems to be inviting the escalation of a situation that need
not necessarily deteriorate. Second, better community-based care and support
would almost certainly mean less crises in the first place.
Contrasting experiences
8.86
Some witnesses expressed a view that evidence presented
to the committee may overly represent negative experiences:
The inquiry will receive a great deal of anecdotal evidence
about the inadequacy of services. For various reasons, the inquiry is unlikely
to hear from people who are satisfied with the service. For example, stigma is
still so great, people who are coping reasonably well will not want to draw
attention to themselves.
Anecdotal evidence can be out of date. Situations can improve or
deteriorate quite rapidly. It can come from people who are so shocked, angry or
distressed and who wish to find some one or something to blame. Two families
can have much the same experience and describe it in quite different ways.[834]
8.87
The Victorian Government commented on the nature of the
inquiry:
The methodology focuses on subjective measures such as
submissions and public hearings which will elicit public and expert opinions
from those who choose to submit, but will be limited if this information is not
balanced by objective evidence of systemic issues regarding state service
provision.[835]
8.88
It is difficult to reconcile this view with the
Victorian Government's own submission which states that the operating
environment in Victoria is one of 'sustained demand pressure', with 'services
operating over capacity, as evidenced by high community caseloads and chronic
acute bed blockages' and 'crisis driven service responses, difficulties with
service and bed access, 'revolving door' clients....and a significant impact on
other social policy areas'.[836]
8.89
There is evidence that confirms that systemic issues
underlie the personal experience of mental health services. Anecdotal
experiences of inpatient and crisis services are consistent with service
reviews, such as the Victorian Auditor-General's finding that:
Increasing service demand and associated levels of unmet demand
are resulting in service access difficulties for many consumer, early discharge
from hospital, and increased burden on family and carers. These outcomes
increase the likelihood of future unplanned re-admissions.[837]
8.90
The NSW Auditor-General similarly remarked:
The increase in demand for emergency mental health services has
offset many (and perhaps all) of the gains from funding increases. The system
is under considerable pressure, and patients can face lengthy delays before
being admitted to a bed.
It is important that services work together to share resources
at times of peak demand. Yet, there are times when the availability of mental
health beds means that some patients face being transferred very long distances
to access an acute mental health bed.
There is also evidence that some patients spend inappropriately
long periods in emergency departments while awaiting acute mental health beds
or are discharged from the emergency department prior to a bed becoming
available.[838]
8.91
The dearth of outcome reports in the mental health
sector also means there is little ongoing, systematic assessment of the actual
health outcomes provided by mental health services. There is generally no data
to contradict many of the systemic issues illustrated by personal anecdotes to
this committee.
8.92
Hearing personal experiences and reporting individual
concerns does not belie the substantial reforms that have occurred, the
systemic deficiencies that remain and the concerted and coordinated effort
required to continue to improve mental health services. The Victorian Government submitted:
A number of [the inquiry] terms of reference sit well outside
the mandate of the specialist mental health system and will require vigorous
and sustained effort by many different areas and levels of government,
including the Commonwealth Government, to address.[839]
8.93
The committee certainly assumes that all levels of
government are committed to making the 'vigorous and sustained effort' required
to improve mental health services, and ultimately the mental health of all
Australians.
Concluding remarks
8.94
There are serious problems facing people with mental
illness who find themselves seeking, or being placed in, acute care. There has
been some discussion of whether these problems are a result of the way in which
the policy of mainstreaming has been implemented. Mainstreaming was intended to
involve the replacement of stand-alone psychiatric facilities with a pattern of
brief admissions to acute psychiatric wards within general hospitals backed up
by community-based care of varying types. However, for many consumers this has
not been the reality.
8.95
A key criticism has been the apparent inability of
mainstream services to meet the specific needs of mental health consumers.
Submitters pointed to the need for tailored treatment and for the treatment
environment to be conducive to recovery:
The other point I would like to make in the broad sense is that
mainstreaming has failed. Mainstreaming was the idea that you bring all mental
health services under the one umbrella of general health and somehow this means
that all discrimination goes away. But that is not the case. There is some
reduction in stigma. One of the good things about mainstreaming is that it
recognised the role of general practitioners. But what it has not done is
maintain a focus on the unique needs of patients with psychiatric illness.
Because of this loss of focus we now have, for example, inpatient units being
built with no space. Psychiatric patients need space. When they are very unwell
they are agitated, they are sometimes very sensitive to others and they need
room.[840]
8.96
Dr Scott-Orr
argued for 'co-located' services, in which psychiatric services share medical
resources with general hospitals, but retain a separate environment and
specialised care:
It is my view that general hospital architecture and functioning
does not lend itself to mental health care. Nor does the recent design of
mental health units in general hospitals give me any hope or joy. I consider
the place(s) of round the clock mental health care should be readily accessible
by walking, to and from the relevant general hospital, and sharing its resources
for all sorts of medical reasons and economies.
It needs to provide a 'homey' environment, with that look and
feel, in which people are up and about in street clothes, preferably to have
its own street address, while having provision for some secure area and ready
observation where needed.[841]
8.97
On the other hand, the Royal Australian and New Zealand
College of Psychiatrists strongly supported mainstreaming:
We should progressively move to integrate mental health into
general health. There are enormous advantages in having the majority of
psychiatric services in general hospitals as part of the culture of general
hospitals with regard to constant review and quality improvement and in the
accessibility of general health care to patients with mental illness as well.
There is probably going to be a need for small specialist services for people
with particular disorders where all they need is psychiatric intensive care,
but I would see that as being a very small part of the much larger integrated
system.[842]
8.98
The committee accepts the argument that bringing acute
psychiatric care into a mainstream hospital setting helps ensure quality
treatment for all of a patient's health needs, and can have workforce and
management advantages. Effective acute care, however, needs to involve higher
standards of care and the provision of facilities that meet the specific needs
(such as open space and a more home-like environment than is typical for a
general hospital) of people with mental illness. Above all, these need to be
linked in to community-based services, before admission and after discharge.
8.99
There is now a substantial body of evidence before this
and other recent inquiries to show that inpatient and crisis mental health
services have severe shortcomings. Services have failed to meet the standards
Australians should now, after many years of inquiry and reform, be able to
expect.
Navigation: Previous Page | Contents | Next Page