Chapter 4 - Resourcing
4.1
There is no doubt that more resources need to be
devoted to mental health services. Time and again the committee heard from
every stakeholder in mental health, from individual consumers to federal and
state governments, saying that more money needs to be spent on services.
4.2
This message is not new. It was clearly articulated in
the Burdekin Report of the early 1990s:
Lack of resources has bedevilled community-based care in much
the same way that inappropriately allocated resources contributed to the
ineptly executed demise of the large institutions. Clearly, resources and
effective coordination are imperative if mainstreaming is going to work.[181]
4.3
The committee heard that mainstreaming, despite the
rhetoric, has not been successful; that a 'silo' mentality continues to exist
within government departments, both state and federal; and that the integration
of services to provide resources where they are most needed has, to a large
extent, simply not occurred. It was suggested that nothing has changed since the
Burdekin Report and that the quote above is as relevant today as it was in
1993.[182]
4.4
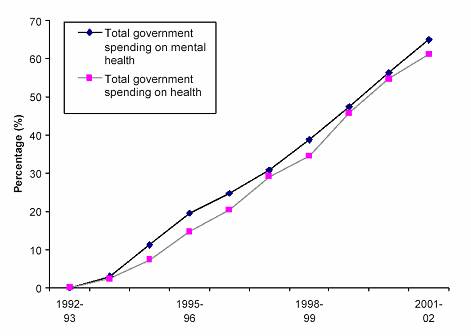
Calls for greater resources certainly appear to have
been met with relatively little action. This is not to say, however, that
resources for mental health have been static for the last ten years. Funding
for mental health has increased steadily (Figure 4.1):
Figure 4.1 Growth in health expenditure and mental health expenditure.[183]
4.5
The graph shows that mental health expenditure rose by
about 65 per cent from 1992–93 to 2001–02. It also reveals the reason why resources
for mental health remain a prominent issue. Ten years ago, mental health was a
neglected field of health care. Since that time, expenditure on mental health
has risen no faster than health expenditure in general. This suggests that
mental health is not being given the priority it needs. Throughout this report
evidence is presented of capacity constraints and neglect across the sector
indicating that resource levels need to rise.
4.6
This chapter outlines the cost of mental health
problems, demonstrates the need for more resources, and outlines debate about
where those resources should go.
The Costs of Mental Illness
4.7
Mental illness costs the country a great deal in many
different ways. There are the human costs in terms of time lost to disability
or death, and the stresses that mental illnesses place upon consumers, carers,
and the community generally. There are financial costs to the economy which
results from the loss of productivity brought on by illness. Then there is the
expenditure by governments, health funds, and individuals associated with
combating mental illness and facilitating mental health.
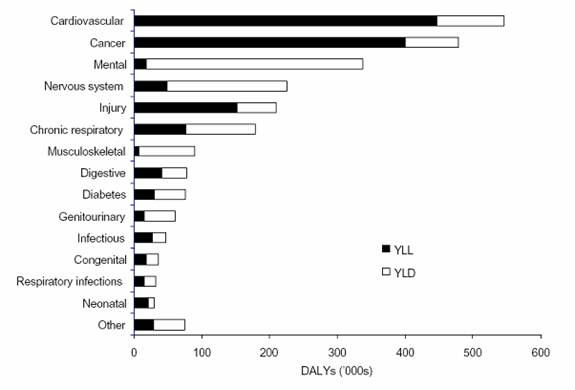
4.8
It is well established, but not well enough understood,
that mental illness is the number one health problem causing years lost to
disability (YLD) in the Australian community.[184]
Other diseases like heart disease and cancer may take more lives, but nothing
causes as much ongoing suffering and disablement as does mental illness. The
level of health burden caused by a disease can be measures in terms of
disability-adjusted life years (DALYs), and Figure 4.2
compares these figures for major types of illness:
Figure 4.2 The burden of mental illness compared.[185]
4.9
Behind the figures showing the very high level of disability
due to mental illness lie two stories, one about health and one about human
suffering. In health terms, mental illnesses are different to most other
illnesses. The overwhelming burden of mental illnesses falls upon the young,
while most other conditions are more likely to affect the old. Thankfully most
mental illness is not fatal. However, the early onset of much mental illness
can mean that sufferers, particularly of acute conditions, can face varying
degrees of disability for many years of their lives. As shown below, this means
mental illnesses can create enormous costs for our health system and our
society – costs that are exacerbated if effective treatment and care are not
provided.
4.10
The human story behind the high level of disability
caused by mental illness is the story of considerable hardship faced by people
experiencing mental illness as well as those who care for them. These hardships
are documented throughout this report, but are borne particularly by the
families of, and other carers for, those experiencing mental illness, and this
is a focus of Chapter 11.
4.11
With so many people who experience mental illnesses
becoming ill at relatively early ages, it should be no surprise that these
conditions have major economic impacts. No comprehensive estimates are
available, but research on three conditions – depression, bipolar disorder and
schizophrenia – gives some indication of the issues. Beyondblue commented that the economic impact of depression was
large:
Apart from the social impact of depression, we know that over $3
billion is lost to our economy each year by not addressing the illness. These
costs are not just to the health sector but include indirect costs that impact
on other portfolio areas, for example welfare and disability support costs.[186]
4.12
SANE Australia
commissioned research on the costs of two particular mental illnesses. That
research showed for bipolar disorder:
The direct and indirect costs of bipolar disorder and associated
suicides are substantial. Real financial costs total $1.59 billion in 2003, 0.2
per cent of GDP and over $16,000 on average for each of nearly 100,000
Australians with the illness. Around half of this cost is borne by people with
the illness and their carers.
– Direct health system costs are estimated at $298 million in
2003, with two-thirds being hospital expenditure, 13 per cent medical
expenditure (GPs and specialists), 11 per cent residential care, 2 per cent
pharmaceuticals and the remainder on allied health, pathology, research and
administration.
– This represents only $3007 per person with bipolar disorder,
even less than spending on the average Australian’s health care and 0.43 per
cent of national health spending.
– 42 per cent of costs relate to depression, 36 per cent to
mania or hypomania and 22 per cent to prophylaxis.
– Real indirect costs are estimated at $833 million, including
$464 million of lost earnings from people unable to work due to the illness,
$145 million due to premature death (the net present value of the mortality
burden), $199 million of carer costs and $25 million of prison, police and
legal costs.
– Transfer payments are estimated at $224 million of lost tax
revenue (patients and carers) and $233 million in welfare and care payments,
primarily comprising disability support pensions.[187]
The results for an analysis of the economic impact of
schizophrenia reveal even larger costs:
The direct and indirect costs of schizophrenia and associated
suicides are enormous. Real financial costs of illness totalled $1.85 billion
in 2001, about 0.3 per cent of GDP and nearly $50 000 on average for each
of more than 37 000 Australians with the illness. Over one third of this
cost is borne by people with the illness and their carers.
– Direct health system costs were $661 million in 2001,
including 60 per cent hospital costs, 22 per cent community mental health
services, 6 per cent medical costs (GPs and specialists), 4 per cent nursing
homes and 2 per cent pharmaceuticals.
– This represents nearly $18 000 per person with
schizophrenia, over six times the spending on the average Australian’s health
care and 1.2 per cent of national health spending. Even so, it is clear that
public health spending in Australia
is at the low end of the international spectrum (1.2 per cent of health
spending compared to 1.6 per cent to 2.6 per cent in other comparable
countries)
– Real indirect costs were $722 million, including $488 million
of lost earnings from people unable to work due to the illness, $94 million due
to premature death (the net present value of the mortality burden), $88 million
of carer costs and $52 million of prison, police and legal costs.
– Transfer costs were $190 million of lost tax revenue (patients
and carers) and $274 million in welfare payments, primarily comprising
disability support pensions.[188]
4.13
As these studies have noted, a considerable proportion
of the economic costs of mental illness are borne by consumers and carers.
However, there is obviously also major government expenditure on mental
illness. For many years now, expenditure on mental health by governments and
private health funds has been outlined in the National Mental
Health Reports.
Expenditure on mental health
4.14
The different levels of government have different roles
in funding the mental health care system:
State and territory governments are primarily responsible for
the management and delivery of public specialised mental health services while
the Australian government, as well as providing leadership on mental health
issues of national significance, also subsidises the cost of primary mental
health services, principally through the Medicare and Pharmaceutical Benefits
Schemes. The Australian government also
subsidises private health insurance and directly funds a number of other
initiatives...[189]
4.15
Total expenditure on mental health services by federal,
state and territory governments and private health funds was $3.3 billion in
2002–03.[190] Detailed description of
historical trends and breakdowns of how the sector is resourced are covered by
the National Mental Health Reports, and are
not reproduced here. More detail is included in Appendix 2 to this report.
Mental health funding has risen in real terms, but it has risen no faster than
health funding generally.
4.16
In addition to this direct spending on mental health,
there is significant indirect expenditure by governments. Indirect expenditure
'refers to the estimated costs...of providing other social, support and income
security programs for people affected by mental illness'. The Commonwealth
indicated it spent $3,648.6 million across the following items:
-
Income support payments.
-
Workforce participation programs.
-
Department of Veterans' Affairs disability
compensation payments.
-
Housing and accommodation programs.
-
Aged care residential and community services.
-
Home and Community Care programs.
-
National Suicide Prevention Strategy (NSPS).[191]
4.17
Government expenditure due to mental illness is even
broader, however. As Chapter 13 will show, a significant number of people who
come into contact with the justice system, do so as a result of mental illness,
and this is an economic cost of caring for the mentally ill that is 'hidden' in
the budgets of state and territory correctional services authorities.
4.18
The private sector plays a significant role in mental
health care:
The private sector contribution towards hospital admission that
relate to MDC 19 Mental Disease and Disorders is substantial and it has
increased. In the last 12 months the proportion of all mental disease and
disorders treatments performed in the private sector increased by 5.7 per cent,
from 37.5 per cent to 43.2 per cent (2001-02 compared with 2002-03, Data source
AIHW).
The private sector provided 95,672 in-hospital treatments for
mental diseases and disorders in 2002-03. This included 73,137 same day
separations and 22,535 overnight admissions. ON average each overnight
admission had an average length of stay of 16.4 days. The private sector
provided 443,210 patient days in private hospitals.
In 2002-03 the private sector contributed at minimum $135
million toward the funding of in-hospital treatments for mental diseases and
disorders.[192]
4.19
There are many non-government organisations that
provide care and assistance for people experiencing mental illness. Some of
these do so under government funding arrangements. Many others, such as
Lifeline and GROW, do so largely on the basis of volunteer time, and donations.
Lifeline Australia
informed the committee that approximately 80 000 (or 27 per cent) of its
counselling calls in 2002 were known to be about mental health and that a study
conducted of Sydney
callers found that 69.5 percent of those callers suffered from high levels of
psychological distress.[193] Except in Victoria,
Lifeline does not receive any recurrent government funding 'to manage
increasing demand of mental callers'. It is interesting, however, that
government agencies refer clients to Lifeline, if they are in crisis.[194]
4.20
A great part of the cost of care of many people
experiencing mental illness is carried by their families and carers. Individual
carers on average contribute 104 hours per week caring, or being on call to
care, for people with mental illnesses.[195]
Without the sustained efforts of carers and family members, the current mental
health system would not function.
4.21
The costs to these families and carers are substantial.
As well as direct and indirect financial costs, families bear the social and
emotional costs of their family members' illnesses. Direct and indirect
financial costs borne by families include:
-
Ongoing expenses of health professionals,
medication and health programs;
-
Costs of travel whether public transport or
personal petrol costs of car & parking fees;
-
Replacing everyday items destroyed from loved
ones inability to use or care for items (saucepans; washing machines; vacuum
cleaners to personal items of clothing etc.);
-
Payment of abnormal expenditure and debts
incurred by loved ones;
-
Loss of incomes with the need to give 24-hour
care to loved ones;
-
Loss of housing opportunities, living with ageing
parents, substandard housing, homeless shelters; and
-
Loss of careers – carers and family members'
inability to fully commit to study and/or careers.[196]
4.22
Social and emotional costs include:
-
Significant health and psychological distress
experienced as a result of caring;
-
Breakdown in relationships due to the burden of
caring;
-
Reduced quality of life – handling the myriad of
issues from ongoing crises and/or relapses; and
-
Loss of self worth because of the stigma of
mental illness.[197]
4.23
Carers described the sacrifices they had made in their
own lives in order to carry out their caring role. One major impact of
providing ongoing care was the inability of carers to maintain full-time
employment. Having to give up jobs, or reduce working hours, not only affected
carers' financial wellbeing, but also their own sense of self and achievement.
I have had to leave my position as a senior social worker...after
20 years in ICU/CCU hospital settings...[198]
I was a very good teacher of maths and science, and, what is
more, enjoyed doing it very much – all my education and experience has been
lost to both myself, and the community, and my role as a carer has ensured that
I enjoy an old age of certain poverty – no superannuation for me![199]
4.24
For some families, lack of employment combined with the
additional costs of providing care leads to poverty.
We
just become poorer and poorer. I cannot get dental care; I’m on the waiting
list for that. You name it; I’m on the waiting list for a number of things
ranging from health care through to accommodation. I probably won’t be able to
keep the car going after this year. The payment I get is just not enough to live on. I can’t remember our
last holiday. I shop at St
Vinnies, haven’t had new
clothes for ages. It is just so tiring trying to make ends meet. It can come
down to, do I buy milk and food or go to the doctors.[200]
4.25
This wide range of sources of funding and support does
not hide two fundamental problems: not enough is spent on mental health
services; and it is not clear the resources are being applied wisely.
Not enough is spent on mental health
4.26
Just about every witness, whether government or
non-government, peak group or special interest group, health care professional
or consumer, indicated that the level of resources is inadequate.
4.27
The Mental Health
Council of Australia's (MHCA) first point about resources for mental health is
that there aren't enough:
The burden of mental illness and associated disability within
the community is not matched by the funding allocated to prevent, relieve and
rehabilitate people experiencing mental health illness.[201]
4.28
This message was explored in detail in their report Not for Service. The Australian Medical
Association (AMA), in response to the release of the MHCA report stated:
The 'Not for Service' report into Australia’s mental health care
system reveals a sad story of inactivity, poor planning, under-funding and
under-resourcing by all Australian governments in the face of one of the
biggest health challenges facing the nation in the 21st century – mental health
care.
At a time when demand for quality mental health services is at
its highest, our national commitment to the mental health sector is
frighteningly inadequate and fragmented.[202]
4.29
Other witnesses agreed including the Victorian Mental
Illness Awareness Council, the Mental Illness Fellowship Australia, and RANZCP:
the greatest impediment to policy implementing has been the
failure of government to provide adequate funding so that what is written as
policy actually can happen in practice.[203]
Federal government needs to lead states and territories in the
implementation of reforms and increase the funding allocation for mental health
and allied services. Australia
spends less than 7 per cent of the health budget on mental health. This sum
places Australia
well down on comparable amounts spent by OECD countries. Despite the low
funding allocated to mental health, it is the leading cause of disability.[204]
RANZCP believes that the mental health system in Australia
has all the right fundamentals but requires additional recurrent funding.
Ideally one billion dollars per year is required to reform existing mental
health service systems, ensure a sustainable workforce, address equity issues
and ensure the provision of an agreed level of service delivery in all
geographic areas.[205]
4.30
Medicines Australia
considered that 'More resources need to be devoted to treat mental illness,
given the disease burden placed on the Australian community'.[206] Beyondblue
broadly concurred:
One billion dollars is required as an injection for mental
health, with the Federal Health Minister taking on portfolio responsibility to
lead a reform agenda. The wider costs associated without a social coalition
approach cannot be underestimated.[207]
4.31
This need reflects widespread public perceptions,
reflected in the 70 letters sent as part of one write-in campaign to the
committee's inquiry,[208] as well as many
individual submissions by carers and consumers:
One of my adult daughters, who lives in NSW, has suffered from
schizophrenia for over ten years. During that time it has become more and more
apparent to me and other family members that there are many inadequacies and
gaps in the provision of adequate mental health care and community support
services for someone with her condition. I think that the majority of these
matters are a direct result of inadequate funds and resources being available
to mental health services.[209]
4.32
While there was a strong consensus on the general lack
of funding for mental health, there were also specific areas where that lack of
resources was perceived to create particular problems. The most prominent
concern was the lack of support for counselling, psychological services and
talk therapies:
Patient out-of-pocket costs are probably a key reason why few
people with depression or anxiety currently receive CBT, despite considerable
evidence for its cost effectiveness.[210]
4.33
Dr Gil
Anaf agreed, saying:
I am most interested to reverse an ill-informed push that aims
to reduce access to long term therapy services, and that aims to only promote
medication and quick-fix therapies as the main rebatable treatments.[211]
4.34
This position was also supported by the National
Association of Practising Psychiatrists, which indicated:
Psychiatrists are placed in an untenable ethical situation of
having to refuse appropriate treatment, where no other treatment would be
efficacious, because most patients do not fulfil the criteria of Item 319, and
because they cannot afford to treat more than one or two, or no, patients at
half the fee. Most patients cannot afford to pay half of the schedule fee if
they receive intensive treatment because many psychiatric patients are
vocationally and thereby financially disadvantaged. This legislation
contravenes the mandate of Medicare of equity of access.[212]
4.35
Psychologists Rudd and Jackson
agreed:
Cost of services is a major barrier for many in need, and not
just at the individual client level. For example, in Victoria,
it has been reported that teachers with special needs students (including
mental health difficulties) often find it difficult to access specialist
Psychologist services because of lack of funding.[213]
4.36
More generally, there was concern that the high level
of copayments was an issue, particularly for those without private health
insurance:
Co-payments are preventing people access to quality health
service. Without measures to reduce copayments, the Commonwealth Fund will continue
to document financial barriers to access for a significant percentage of
Australians. Those with mental illnesses will be amongst the most likely to
suffer.[214]
I can’t afford psychological counselling even with the $50
refund provided by my private health fund. My annual net medical expenses are
already about $7000. Medicare Plus also provides reimbursement of $50 for up to
five counselling sessions in a year but five sessions is not enough and it is
still expensive.[215]
4.37
The Australian
Council of Social Services (ACOSS) and others were concerned about equity of
access, citing as an example:
psychological counselling services, [which] are highly
restricted within the public system but available to those with sufficient
private means and/or private health insurance.[216]
4.38
Australian College
of Psychological Medicine noted:
Many sufferers from significant mental health disorders require
a multi-disciplinary approach, with the majority of them too socially
disadvantaged to afford private health insurance.[217]
4.39
BlueVoices reported a consumer saying 'I cannot afford
private health insurance so my only option for treatment is medication'.[218] This seems a recurrent and
disturbing complaint. BlueVoices also indicated that:
many consumers report to us that unless they have private health
insurance they are unable to afford the recommended fee of the Australian
Psychological Society for cognitive behaviour therapy from a Registered
Psychologist.[219]
Inappropriate targeting of spending on mental health
4.40
While the dominant theme in the inquiry was the
inadequacy of spending on mental health, issues were also raised around how
that spending was being prioritised and administered. A question repeatedly
raised about the allocation of funding for mental health, is why mental health
does not receive a greater proportion of the health budget:
In Australia,
the provision of mental health services receives an inappropriately low
priority having regard to the large number of people affected, the high burden
of disability, the untoward impact on service-deprived sub-groups within the
community and the missed potential for the cost-effective achievement of better
health outcomes. International comparisons of mental health spending are dated
(circa 1993) but suggest a spending shortfall in Australia
compared to Canada,
the US and the Netherlands.
A decade or so after the deinstitutionalisation of mental health, it is now
obvious that governments did not ensure enough resources for the new
community-based care structures to operate effectively.[220]
...
The Sane Mental Health Report 2004; 'Dare to Care' states that
Australia
spends less than 8 per cent of its national Health Budget on mental
health. The same report asserts that
comparable OECD countries spend upward of 12 per cent of their health budget on
mental health.[221]
...
While total health funding has grown over the life of the
National Mental Health Strategy, spending on
mental health has remained static in comparison with overall health spending;
yet mental health has grown as a component of the overall health burden.[222]
4.41
Another recurrent theme was the contrast between the
mechanisms for Commonwealth funds allocation and those of the states and
territories. Victoria
argued:
The Commonwealth funded health care system also constrains and
provides barriers to improving services to people with serious mental illness.
For example, newer atypical pharmaceuticals used to treat psychosis are not
always funded by the Pharmaceutical Benefits Scheme so the states must find
this funding. Additionally, the Medicare Scheme does not impose significant
restrictions on the number of visits to private psychiatrists. Neither are
there adequate controls over the distribution of private psychiatrists, nor on
priority of access for those people most in need. Few incentives exist for
psychiatrists to take on new clients or to work in a public sector with capped
funding and more complex clients...
4.42
The South Australian Government described the problems
of coordinating services 'when enhancement monies from the Australian Government
may promote particular or specific aspects of a service only'.[223] The Queensland Government noted the
difficulties faced by the states and territories in 'invest[ing] new monies
each year on a recurrent basis, representing real growth in monetary terms',
which results in them having to 'fully fund reform'.[224] The Victorian Government argued:
More weight should be given to the constraints the states and
territories operate under that impact on the rate and extent of change. These
constraints include capped budgets and high levels of non-discretionary
expenditure related to meeting statutory obligations to involuntary clients.[225]
4.43
There was particular concern about the direction of
funds to medication and away from other therapies. Over the nine-year period of
the mental health strategy:
the Australian Government’s contribution increased 127 per cent,
though 66 per cent of this increase was accounted for simply by the increase in
expenditure on medications through the Pharmaceutical Benefits Scheme. While
new medications play an important role in improving mental health outcomes, to
achieve value for money they need to be backed by complementary psychological,
social, informational and self-management strategies. To date, significant
developments in these other areas have been promising but limited in scope or
reach (Hickie et al. 2004) and now require more overt long-term support by the
Australian Government.[226]
Psychotherapy (such as Cognitive Behavioural Therapy) has proved
to be a cost effective treatment for some mental disorders, especially anxiety
and depression. However, under the current Medicare arrangements, Medicare only
funds psychotherapy costs where the provider is either a psychiatrist or a
general practitioner with some welcome, but limited provision, for psychology
services through new initiatives such as Better outcomes in Mental
Health. This effectively restricts longer term psychotherapy
access to those people who either have ancillary private health insurance (for
a psychologist only) or can afford to pay the costs themselves, or to seek
treatment from a psychiatrist or general practitioner, or public mental health
services.[227]
4.44
The Western Australian Government also commented on the
true basis for the increase in expenditure on mental health by the Australian Government
since 1993:
When this increase (65 per cent in real terms) is further
examined it is found that in constant prices the major area of growth is in
Pharmaceuticals provided under the PBS. The increase in expenditure for
psychiatric drugs is nearly 600 per cent during this time period and accounts
for nearly two thirds of all the growth in Federal mental health expenditure.[228]
4.45
Other concerns have also been raised about the
allocation of resources, including that research on mental illness is
under-resourced:
At present, Australia
spends 3 per cent of funding on mental health research, compared to 9 per cent
for cancer research. The 8.9 per cent of NHMRC funds spent on mental health is
small when compared to the 19.1 per cent contribution of mental disorders to
disease burden in Australia.
Compared to other OECD countries, Australia
spends relatively little on research.[229]
4.46
The Commonwealth was critical of the argument that
money should be allocated directly according to percentage of disease burden.
Pointing out that costs of treatment vary from illness to illness, Mr
Davies of the Department of Health and
Ageing said:
to argue that the spending should be proportionate to the burden
of disease is not a safe line of argument to pursue, because obviously the costs
of treating different types of conditions vary. Just because something is 10
per cent of our burden of disease, to argue we should spend 10 per cent of our
health budget on it is not really a logical line of argument.
CHAIR—What is the argument? What is the line of establishing
what the level of spending is for particular burdens of disease?
Mr Davies—Spending
in health care and the allocation of resources between different conditions is
essentially a social, political, societal decision. In terms of the services we
fund, as the Australian government, all that Medicare spending, the PBS
spending, is ultimately determined by people’s propensity to seek out services
and doctors’ propensity to prescribe. There is no cap on the total MBS or PBS
budget, nor is there an allocation of that as between mental health and other
services. It is very much demand driven for the Australian government funding.[230]
4.47
The committee formed a clear impression that while Mr
Davies may be correct, the prevailing
'social, political, societal' view is that resources for mental health are
deficient.
4.48
Consumer groups are concerned about whether consumers
have an adequate role within the funded health care system:
Consumer self advocacy groups, organisations and individuals
have insufficient funding to provide the overwhelming support needs of
consumers whose rights have been abused. Nor do we have funding to provide the
kinds of alternative supports that we know will work for many of us. Nor do we
have funding to allow us to hold forums, conferences, communicate with each
other. Without funding we remain voiceless and disconnected. Without funding we
cannot participate in any of the ways that our mental health policies tell us
we should be participating.[231]
4.49
It was also argued that funds provided to advocacy
groups have not been targeted appropriately:
Current funding to consumer groups hosted and controlled by
groups such as MHCA and ‘beyondblue’ is a misuse of these limited funds and
needs to be redirected to genuine consumer-survivor organisations.[232]
4.50
Non-government organisations (NGO) are an integral
component of the mental healthcare workforce, providing much-needed services to
the community that are either not available – or in short supply – through the
public or private systems. Federal, state and territory funding to NGOs,
particularly funding allocated on a recurrent basis, is severely limited,
reducing the ability of NGOs to provide an optimal level of service. NGOs
reported that the shortage of funding has resulted in having to turn away
people who are in need of help. These matters are examined in Chapter 9. Instead of funding NGOs, including
consumer-run organisations, the vast majority of resources continue to be
channelled to the public and private for-profit organisations.
The problem of the pilot
4.51
As the committee travelled across Australia,
it kept hearing about promising pilot schemes, project trials and new program
proposals that were not receiving funding support. There were recurrent
complaints that pilots were not rolled out to a broader public, regardless of
their success; that projects were not placed on a sustainable budget basis; and
that groups applying for grants could not effectively plan for the future of
their operations.
4.52
The MHCA submitted:
Australia
is often known as “the land of pilots”, and with good reason. The mental health sector is littered with
project and pilots that are funded for a short period and then abandoned.[233]
4.53
The NT Mental Health
Coalition submitted that:
... over the past few years the federal government has funded some very innovative and effective
'pilot projects'. However, the lack of ongoing funding for these projects from
either the federal or NT governments has resulted in the loss of good services
and clients having expectations being raised only to be disappointed.[234]
4.54
St Luke's
Anglicare Limited, which offers Psychiatric Disability Rehabilitation and
Support programs stated:
Our agency has been able to provide some pilot recovery programs
for young people who experience psychosis but we have no recurrent funding to
support these early intervention recovery and rehabilitation programs in the
longer term. Philanthropic sources of funding are very limited for this group
of consumers.[235]
They recommended that recurrent funding be provided for such
services so that target programs for young adults could be offered.[236]
4.55
The SA Divisions of Private Practice also raised
concerns about the current practice of providing short-term funds for pilot
programs:
... Divisions of General Practice have a history of episodic,
short-term project, and pilot funding by government. This is also evident in other parts of the
health system, especially for work that seeks to bring about system
change. By the time one project nears
completion, the funding agenda has moved on and hence the opportunity to
capitalise on the learnings and apply them more broadly is lost. SADI recently had the experience of a
successful pilot project which aimed to re-align private psychiatrist practice.
... This project was terminated by the Commonwealth Government Department of
Health and Ageing at the completion of the pilot phase ... The termination
occurred before the planned (and paid for) evaluation had been completed or
submitted. No evidence was provided as
to why this decision was made. It was
clearly not based on objective analysis of the comparative evaluation
data. Short term episodic funding often
makes the whole system worse, as clinicians, consumers and carers become
cynical. ... Pilot projects need to be a part of an overall strategy, and if they
show benefit, need to be rolled out more broadly.[237]
4.56
Concern about insecure funding and a preponderance of
pilot projects was shared by other groups.[238]
The committee heard about a dieting disorder pilot program that was neither
continued nor expanded, despite no evidence to suggest it had produced poor
results.[239] It heard about the lack
of recurrent funding to indigenous community-controlled health organisations
being linked to service delivery inefficiencies.[240] Similar stories were recounted by
many organisations, particularly those in the non-government sector involved in
advocacy, support and service delivery.
4.57
MHCA identified a number of difficulties for
organisations and programs that receive short-term funding, including that:
consumers, their carers and families become distressed, with adverse effects on
their mental health, when a successful program is cancelled; uncertainty
regarding tenure acts as a barrier to recruiting and retaining quality staff;
organisations suffer a loss of corporate knowledge; and organisations can be
prevented from engaging in long-term planning.[241] The St. Vincent de Paul Society also
identified those difficulties for organisations and recommended a return to
recurrent funding to guarantee continuity of programs.[242]
What more is needed?
4.58
More funding is needed for mental health care, but
attention needs to be paid to more than just the amount. The committee heard
that other areas of concern are that mental health care be extended to more
people; that enhanced resourcing must go hand in hand with continuing reform;
that there be better integration of services; and there be more accountability
for and evaluation of mental health expenditure.
Greater resources
4.59
Witnesses made suggestions about how much extra funding
was needed. The Royal Australian and New Zealand College of Psychiatrists
(RANZCP) believes that:
... the mental health system in Australia
has all the right fundamentals but requires additional recurrent funding.
Ideally one billion dollars per year is required to reform existing mental
health service systems, ensure a sustainable workforce, address equity issues
and ensure the provision of an agreed level of service delivery in all
geographic areas.[243]
4.60
In an answer to a question from the committee about the
application of those funds, RANZCP responded as follows:
... the RANZCP seeks a level of funding for mental health care
commensurate with the burden of the disease. We provide below a breakdown of
the major targets for increased funding.
-
An additional $500 million a year is required for primary mental health
care, including access to allied health professionals, the Better Outcomes in
Mental Health Care Initiative, and reform of the Medicare Benefits Schedule
rebate for psychiatrists to encourage better delivery of consultancy services.
-
Youth mental health requires an additional $50 million per year.
-
Funding for mental health research should be increased from $15 million
to $50 million per year.
-
The remaining funding we envisage would be spent on the following
components, although these components are not all individually costed.
-
Employment participation, including:
-
Specialised schemes for people on a Disability Support Pension to
resume work;
-
Trials of workplace mental health awareness, screening and
implementation programs.
-
Population measures (such as destigmatisation programs, community
education, prevention, and early intervention).
-
Assistance for consumers and carers.
-
Annual and independent reporting on progress in national mental health
reform ($300,000 per year).[244]
4.61
The RANZCP expected that the money would come from the
states and territories, as well as the Commonwealth and did not consider that
funds should be transferred from other areas of the health budget.[245]
4.62
As stated earlier Medicines Australia recommended a
similar increase in funding, as did the MHCA:
Increase expenditure on mental health by $1.1 billion per year
over the next ten years, refocus funding on the full spectrum of service
provision system and adjust existing funding mechanisms to bring them into line
with the new funding (not the other way around as is more usual).[246]
4.63
The MHCA also submitted that the recommended increased
funding should be applied differently from current funding:
We submit that, while significantly more funds are needed to
deliver acceptable mental health care, on their own they will not fix the
problems, merely deliver the same sort of services more widely. The Strategy
has got the broad policy right but continuation of its present approach will
waste money and lives. What is needed is:
-
leadership,
-
accountability,
-
governance, and
-
investment in research and innovation.[247]
4.64
ORYGEN provide specialised mental health services for
youth aged 12-25 years, and have advocated a roll out of their services to
youths nationwide. This involves the establishment
of 30 new services units across Australia
to serve an equivalent number of young people as is currently occurring through
ORYGEN's Victoria-based model. It is estimated that eight specialised mental
health services for youth would be required in NSW, seven in Victoria,
five in Queensland, three each in
Western Australia and South
Australia, two in Tasmania
and one each in the Northern Territory
and Australian Capital Territory.
4.65
ORYGEN have estimated the annual operating costs for each service at $17.5 million, with a total recurrent
cost of $525 million per annum.[248] Some of these costs would be offset by the
re-distribution of existing resources within Child Adolescent Mental Health Services and Adult Mental Health Services. However, capital costs would also
be required to establish the new services.[249]
4.66
ACOSS expressed concern about where extra resources
should go:
Calls for major increases in the mental health budget must be
weighed carefully against other options, which may help lower the incidence and
severity of mental illness and its impact at the individual and community
level.[250]
More coverage
4.67
Only approximately 40 per cent of people with mental
health disorders access professional help. As the MHCA asked:
What other health sector would accept a non-response rate of 62
per cent in any 12 month period.[251]
4.68
Families, carers and community groups are left to deal
with the majority of untreated cases. Yet:
Nobody suggest that we restrict funding for osteoarthritis so
that we only treat half the sufferers and require the community groups to
provide exercise and weight loss programs to the remainder. Nor do people suggest we restrict the supply
of statins to reduce cholesterol levels to half the people with high cholesterol
and require community groups to encourage lifestyle modifications for the
remainder of people at risk of cardiovascular disease. Why do we accept low
coverage levels and inadequate treatment for people with mental disorder? It is
one of the enduring puzzles that is not unique to Australia.[252]
4.69
Professor Gavin
Andrews argued that the necessity for
greater funding is not to improve existing care, but to meet this significant
unmet need:
We do not need additional funds to provide care to the 40 per
cent of the people currently consulting, we just need good management to ensure
that the appropriate care is supplied in the least restrictive
environment. We will need to double the
funds if we are to double the proportion of people in need who are seeking care,
to the level of people with physical disorders who seek care. I cannot think of any justification for the
under-treatment of people with mental disorders.[253]
4.70
There are thus at least two drivers of increasing
expenditure: the need for better services; and the need to serve more
people.
More reform
4.71
As Chapters 8 and 9 will reveal, the transition from
the old psychiatric institutions to mainstream hospitals and community-based
care is incomplete, and some believe it is a reform agenda that has stalled.
One of the key consequences of the slowness of reforms is that funds fail to be
freed up for new initiatives and high priority needs. Failure to close
stand-alone institutions, a phenomenon most marked in NSW and South
Australia, creates budget pressures that prevent the
transformation of the mental health care system.[254] This is because without the
closures, savings are not available to be reallocated to other services. This
is consistent with the experience of reform in Italy,
in which the closure of institutions helped force the development of effective
community care.[255]
4.72
While the closure of institutions may have forced
Australian governments to develop community care, this can hardly be said to be
adequate. Anglicare Tasmania
quoted from a study of the effects that the closure of institutions has had on
homelessness, in which it is suggested that authorities failed to recognise the
range of services that institutions provided, including the provision of
housing, and to fully cost and transfer those functions to community programs.[256]
4.73
Boystown identified a number of areas for reform:
Review costs associated with the delivery of integrated mental
health care. Special attention should be paid to decision making processes for
listing psychotropic medications under the Public Benefits Scheme and the
availability of comparable generic alternatives; access to bulk billing
services; and the criteria for accessing the Disability Support Pension.[257]
4.74
Many areas for further reform are discussed in more
detail in subsequent chapters of the report.
More integration
4.75
A more collaborative approach between all levels of
government is required to address the current 'crisis' in service delivery. The
Parliamentary Secretary to the Minister for Health and Ageing, the Hon
Christopher Pyne MP, outlined his view of the importance of addressing mental
health issues in the National Mental Health
Report 2004:
I...am aware that improving the mental health of the community
requires coordination across diverse areas of public policy, both within and
external to the health portfolio. Coordination
with action taken under the National Drug
Strategy and the National Suicide Prevention Strategy is especially critical,
but the need for linked initiatives extends to areas such as housing,
employment, social security, crime prevention and justice. Mental health can no longer be treated as an
isolated issue.[258]
4.76
The Parliamentary Secretary went further on a
subsequent occasion, saying that
Australia’s
states and territories stand condemned for their failure to deliver adequate
mental health services . . . perhaps it is time for them to cede their
responsibility for mental health to the Commonwealth.[259]
4.77
Professor Andrews
argued that these comments reflect concern both about the effects of
federalism, and the effects of poorly coordinated services:
Part of [Pyne's] rhetoric should be viewed in the light of
federal–state relationships. However, part does reflect the uncoordinated way
we fund our health systems — Medicare and Pharmaceutical Benefits at the
federal level, private health insurance, the state and territory provision of
public-sector services, and rising out-of-pocket expenses at the individual
level. A coordinated funding system would be preferable.
There are six contributors to Australia’s mental health service
— general practitioners, private psychiatrists, private psychologists, private
hospitals, state inpatient and community services, and non-government
charitable organisations. The work of these contributors is poorly coordinated.
It is like a six-horse chariot with six horsemen who seldom communicate.[260]
4.78
Others expressed similar concerns, complaining that
both governments and some individual agencies were 'passing the buck' for
providing better services:
There needs to be more resources as well as a better use of
existing resources and an acknowledgement that all Australian governments must
work together to provide adequate services for the mentally ill...
The statement by Christopher
Pyne, Australian Government Parliamentary
Secretary for Health: “Australia’s
States and Territories stand condemned for their failure to deliver adequate mental
health services” indicates a buck-passing mentality that is part of the
problem.[261]
A whole-of government
approach to mental health policy and funding should emerge from the
Commonwealth, in order to see the same level of integration in the States’
delivery of services. ...resources could be
better utilised if various silos of government were to develop more effective
collaborative arrangements...
The prerequisite to
achieving this is that the policy dialogue moves away from what have become
traditional notions of ‘core business’ beyond which an agency will accept no
responsibility, towards a ‘without prejudice’ discussion of those issues which
no single agency can hope to resolve and which are therefore ‘everybody’s
business’[262]
4.79
The patchwork of federal and state funding, coupled
with the provision of direct and indirect government funding to non-government
organisations, and a growing and changing role for the private sector, means
that integration, while vital, is a constant challenge.
4.80
The AMA was also critical of the way in which funds are
utilised within the mental health service sector:
Existing funding mechanisms favour defined episodes of care.
However the mental health conditions that generate the highest burden of
disease are chronic conditions and they require longitudinal care. The
Commonwealth/State funding arrangements are dysfunctional, funds are wasted in
duplication of administration and policy formulation while a silo mentality
detracts from the continuum of care.[263]
4.81
A consumer group said:
One of the biggest sticking
points for mental health services, including community non-government
organisations, is that the co-ordination of funding between commonwealth and
state governments via the CSDA agreement is an absolute bureaucratic nightmare,
full of gaps, centres more on “let’s try and short change this government or
that health service provider” than actually adequate[ly] funding in ‘real’
terms the ‘real’ costs of mental health service delivery that meets the needs
of people with a mental illness.[264]
4.82
RANZCP submitted that care must extend beyond mental
health care to all other relevant services needed by patients (general health
care, financial support, housing, substance abuse, rehabilitation etc.) and that
the development of a single integrated health system would require the removal
of structural barriers at state and Commonwealth levels, and substantial reform
in both sectors.[265]
4.83
RANZCP suggested the following strategies to achieve
better coordination:
-
the re-integration of drug and alcohol and dementia services with
mental health services;
-
inclusion of developmental disability services as an essential
component of the service matrix;
-
funding of nursing and allied health professionals in private
psychiatric outpatient practices such as More Allied Health Services (MAHS);
-
development of “stepped care” systems linking GPs and state mental
health services in the care of common and severe disorders, including
prioritisation of GP referrals over self-referrals in state services; and
-
encouragement of integrated staffing models, with more flexible
arrangements for public and private psychiatrists to work together will also
strengthen system effectiveness.[266]
More accountability and evaluation
4.84
As already outlined, funding for mental health is a
complex patchwork of direct and indirect expenditure, by different levels of
government, with spending based on numerous different policies, formulae and
guidelines. The National Mental health Strategy is meant to place the resourcing
of mental health in a coherent strategic framework, but it lacks a sharp focus
and was widely condemned for having few measurable performance benchmarks:
Unfortunately, what has been lost in this complex model of
funding and evaluation is effective service provision to the consumers, the
people at the heart of the issue. The National Mental Health
Strategy is not delivering mental health services effectively or efficiently
because it focuses on the process of managing funds and statutory relationships,
not on providing services to those people who desperately need them.[267]
4.85
The regular publication of National Mental
Health Reports provides a mechanism for accounting for
expenditure on and provision of mental health services at an aggregated level.
However, dollar figures and trends alone do not provide a complete picture on
whether expenditure has had any meaningful impact on service provision and
better mental health outcomes:
Whilst there have been eight National mental health reports
since 1994, there is still no accounting in them for the number of people that
are actually seen and treated in mental health services and whether they are
seen face-to-face, or merely by telephone contact. This contrasts with very specific details of
the number of Australians treated and even the number of hours spent treating
consumers by private psychiatrists in the private mental health sector. While
the private mental health sector has been collecting outcome measures of
consumers treated in private psychiatric hospitals over the last three years,
the public mental health system is only just starting to approach such a
project. There are also rumblings from
public sector clinicians that unless there is a very significant increase in
funding for such data collection, the outcome measurement process is likely to
further undermine the management of consumers in the public mental health
system.[268]
4.86
Additionally, it is not clear that the data that is
contained in the National Mental Health Reports findings necessarily reflect
the real position. The Australian Psychological Society (APS) submitted:
Although financial reports
support the conclusion that funding for mental health services has kept pace
with that provided to other areas of health, there is a strong sense from workers
in mental health facilities that positions have been lost, budgets reduced and
less and less services are able to be provided.
Repeated reports from APS members working in institutions or under
specific programs have raised concerns regarding this reduced level of funding
for mental health services by state and local instrumentalities. Although
these situations are clearly anecdotal, they are indicators of a crisis which
we believe currently exists in public mental health services.[269]
4.87
The MHCA also criticised the lack of accountability for
the provision of mental health services:
Over half of all public mental health services had not even
reviewed their performance against these standards [National Standards for
Mental Health Services] by June 2003, some seven years after they were agreed
to by all governments. This is a very clear example of the lack of
accountability and commitment to mental health by all Australian governments.
The reality of the reports of consumers, carers and providers is that they put
flesh on the difficulties of a system struggling to cope with the human cost of
the huge gap between policy and its implementation.[270]
4.88
The National Mental Health Centre submitted:
Crucial to addressing underlying impediments to realization of
these rights, such as disproportionately low mental health service funding and
priority from a whole-of-government perspective is the development of a
mechanism to ensure transparent service delivery and proper accountability of
mental health providers. Lack of accountability and secrecy systemically
undermine the legitimacy of complaints of people who have mental illness and
the confidence the community can have in the complaints systems and services
themselves.[271]
4.89
Part of the dysfunction of current funding arrangements
may well be attributable to the lack of discernable population health
monitoring. Professor Anthony
Jorm of the ORYGEN Research Centre advised:
It is amazing that we know so little about whether mental health
in Australia is
improving, worsening or stable. The only routinely collected indicator of
population mental health is the suicide rate.... We need to have other population
indicators which will monitor how we are doing as a nation and allow resources
to be focussed on sub-groups that are not doing well.[272]
4.90
Professor Jorm
further posits the question:
Why doesn’t Australia
already have population monitoring? The Australian Bureau of Statistics has
been collecting national data on mental health since the 1980s. However, they
have changed the measure they have used several times, making comparison over
time impossible. Even when a consistent measure has been used, other aspects of
the methodology have been changed. There is a need for consistent measures
collected at regular intervals using the same methodology.[273]
4.91
Catholic Health Australia
stated that governments should be aiming towards marked percentage improvements
in the health status and quality of life in the population generally and in
particular for vulnerable groups and recommended that:
Commonwealth and State/Territory Governments ... set targets for
improvements in mental health outcomes across the community and for specific
groups in greatest need and be held accountable for meeting these targets. [274]
4.92
The AMA suggested that the following themes should be
included in accountability mechanisms:
The importance of a proper econometric analysis of the need,
including the unmet need, for mental health services in Australia
with this analysis incorporated into future National Mental Health reports.
- The desirability of mandatory reporting by State
and Territory jurisdictions of the number of people treated and whether those
people are treated face-to-face or by telephone.
- The need for a significant increase in the
resources for outcome measurement in the public mental health system.[275]
4.93
It was widely argued that the establishment of a
national mental health commission would be a major step towards ensuring proper
accountability for mental health provision. A group of Australia's
most prominent mental health experts made a compelling case for the
establishment of an independent Mental Health
Commission to fill the role of anti-discrimination campaigner, information
repository and leader of coordinated mental health reform.[276] The authors cited the successful New
Zealand Commission as particularly suggestive for Australia,
but also referred to similar bodies in the United
States and the United
Kingdom.[277]
The New Zealand Commission has widespread powers encompassing:
-
human rights and anti discrimination agendas
without being restricted to these agendas (as would a commission set up under
the HREOC);
-
a formal mandate to monitor and identify service
gaps, oversee training and performance management and conduct evidence based
reviews and consultations;
-
an ability to provide continuity through
government change; and
-
the capacity to pursue a positive political
agenda, avoiding sequential and often unproductive inquiries.[278]
4.94
The model is distinctive in that the Commission is
established by legislation for a defined period, to perform specified tasks to
a set time frame, with the options of extensions until its work is assessed to
be completed:[279] 'ultimately, doing
itself out of a job becomes the measure of its success'.[280]
4.95
Particularly promising is the potential to override
federal, and state and territory tensions with their resulting 'buck passing'
and compartmentalisation of services. Despite concerns that the NZ Commission
would act as an unconstructive critic of Government, the NZ Ministry of Health,
Directorate of Mental Health, has found it has
been a most effective partner 'walking alongside us' in the reform process.[281]
4.96
Under the auspices of the New Zealand Commission,
mental health reform has replicated or adapted several Australian mental health
initiatives.[282] However, in New
Zealand these reforms were embedded after
wide consultation and appraisal of the international evidence base; service
gaps were then identified and resources accurately costed to fill these gaps.[283]
4.97
Many others were supportive of a commission. The Mental
Health Legal Centre, for example, submitted:
... the establishment of an adequately empowered and independent
national complaints and accountability mechanism may well be the only way to
address the serious deficiencies in terms of both 'civil libertarian' and service
access and quality rights which endure, Burdekin Report and National Mental
Health Strategy notwithstanding.[284]
4.98
The MHCA suggested:
That the Commonwealth Government establish regular, frequent and
formal reporting mechanisms to the Prime Minister and Heads of Governments on
specific key indicators including an annual public report to the Prime
minister, 'The State of our Mental
Health', with data which reflects user and carer experience, not just system
measuring indicators. Leadership of this process should be vested in an
independent, empowered national office or person with direct access to the
Prime Minister.
That the day-to-day responsibility for the National Mental
Health Strategy within the Commonwealth Government rests with the Cabinet level
Minister.[285]
4.99
The Centre for Psychiatric Nursing Research and
Practice and many others argued for a commission that would provide independent
monitoring and recommendations to guide performance of mental health services.[286]
Conclusion
4.100
This chapter has given a broad picture of how mental
health services are resourced, and a brief sample of the barrage of criticism
levelled at the system. It is not often that a committee hears such a united
chorus of criticism from such a diverse array of organisations and individuals,
and the concerns obviously raise serious questions about the adequacy of mental
health care in Australia.
4.101
Later chapters look in more depth at specific areas of
mental health care. First, however, the committee considered the diversity of
mental illnesses, and some of the fundamental assumptions that underpin their
treatment.
Navigation: Previous Page | Contents | Next Page