Chapter 7 - Quality improvement programs
7.1
This chapter discusses the
inquiry’s terms of reference relating to the effectiveness of quality
improvement programs to reduce the frequency of adverse events. While the terms
of reference specifically focus on programs for quality improvement much of the
evidence received by the Committee discussed quality improvement in general
terms. This chapter focuses on these broader issues as the evidence indicated
that a discussion of quality improvement cannot be solely restricted to its
impact in addressing adverse events given the impact of these programs on other
quality of care issues.
7.2
It was highlighted during the
inquiry that the community has a right to expect that the quality of care in
public hospitals meets the highest standards. While most treatments carry some
risk, the hospital system should be organised to minimise those risks and the
extent of any injury which might result from an adverse event. A concern for
safe, high quality care should permeate the whole public hospital system.[367] While evidence to the Committee
indicated that the quality of public hospital services in Australia
is of a generally high standard it was emphasised during the inquiry that in
several critical areas safety and quality could be enhanced.[368]
7.3
Several Australian studies in
the 1990s have focussed on the issue of quality and safety in health care. The
1995 Quality in Australian Health Care Study focussed particular attention on
safety issues by suggesting that a higher than expected number of hospital
admissions were associated with adverse events. Following the release of the
findings of the study, the Taskforce on Quality in Australian Health Care was
established in June 1995 to consider the data and report to Australian Health
Ministers on measures to reduce the incidence and impact of adverse events in
the health care system. The Taskforce reported to Health Ministers in June
1996. In March 1997, the National Expert Advisory Group on Safety and Quality
in Australian Health Care was established to provide practical advice to Health
Ministers on further steps to improve safety and quality of health care
services. The National Expert Group presented its Interim Report to Health
Ministers in July 1998 and its Final Report in August 1999.[369]
Definition of quality improvement
7.4
The subject of quality in
health care has been described as ‘bedevilled with definitional confusion and
ambiguities’.[370] Terms such as
‘quality’, ‘quality improvement’ or ‘quality assurance’ are often difficult to
precisely define and are often used interchangeably. During the inquiry, a number of terms were
referred to when describing quality of care issues including ‘quality
improvement’, ‘quality management’ and ‘quality assurance’. ‘Quality
improvement’ in the context of hospitals has been defined as the end result of
effective quality management and can be measured in relation to the degree to
which practices in hospitals result in the production of known or assumed
maximum health status improvement for patients. Quality improvement has three
components - identifying problems within hospitals, for the most part
identifying system defects; resolving those problems; and measuring the
resultant improvement.[371]
7.5
‘Quality management’ has been
described as an umbrella term that includes a wide range of hospital activity
designed to produce a ‘quality mature’ hospital. Quality management includes
such activity as quality assurance, risk management, credentialling of medical
staff, incident reporting and analysis, adverse events monitoring, quality
assessment and quality improvement. A ‘quality management program’ is defined
as an organised, coherent, range of activities that will enable the hospital
and its medical staff to improve the quality of care provided.[372] ‘Quality assurance’ has been
described as the process of ensuring that clinical care conforms to criteria or
standards and is a subset of quality management.[373] Generally the term ‘quality
improvement’ is used throughout this chapter as it relates directly to the
terms of reference and is the term most commonly used in submissions and other
evidence to the inquiry.
Nature and extent of adverse events
7.6
There is little data on adverse
events in Australia. The 1994 the Quality in Australian Health Care Study
(QAHCS) was commissioned by the then Commonwealth Department of Human Services
and Health to determine the proportion of admissions associated with an adverse
event (AE) in Australian hospitals.[374]
This was the first published study in Australia that attempted to identify
quality of care problems in Australian hospitals.
7.7
There is no nationally or
internationally agreed definition of what constitutes an adverse event. In the
Australian context, the Quality in Australian Health Care Study defined an
adverse event as ‘an unintended injury or complication which results in
disability, death or prolongation of hospital stay, and is caused by health
care management rather than the patient’s disease’.[375]
7.8
The QAHCS study found that 16.6
per cent of hospital admissions were associated with an adverse event and 51
per cent of the adverse events were considered preventable.[376] While in 77.1 per cent of cases the
disability had resolved within 12 months, in 13.7 per cent the disability
was permanent and in 4.9 per cent the patient died. For the two categories of
‘death’ and ‘greater than 50 per cent permanent disability’, the proportion of
high preventability were 70 per cent and 58 per cent respectively. There was a
statistically significant relationship between disability and preventability,
with high preventability being associated with greater disability.[377] The proportion of admissions
associated with permanent disability or death due to adverse events increased
with age; however temporary disability and preventability were not associated
with age or other patient variables.
7.9
A significantly lower
proportion of the adverse events were reported for obstetrics (7.2 per cent)
and ear, nose and throat surgery (7.9 per cent) than for other specialities,
while a higher proportion were associated with digestive (23.2 per cent),
musculoskeletal (21.9 per cent) and circulatory (20.2 per cent) disorders.
7.10
The study found that
extrapolating the data on the proportion of admissions and the additional
bed-days associated with adverse events to all hospitals in Australia in 1992
indicated that about 470 000 admissions and 3.3 million bed days were
attributable to AEs.[378] The study
also found that the number of patients dying or incurring permanent disability
each year in Australian hospitals as a result of AEs was estimated to be -
18 000 deaths, 17 000 cases with permanent disability, 50 000
cases resulting in temporary disability and 280 000 cases of temporary
disability.[379]
7.11
A Victorian study recorded an
adverse event rate of 5 per cent of separations using inpatient data from all
public and private acute care hospitals in that State in 1994-95. Most (81 per
cent) were complications after surgery or other procedures; 19 per cent
were adverse drug effects; and 1.7 per cent were misadventures.[380] The study has, however, been criticised
on the basis of the less rigorous definitions it employed than the Quality in
Australian Health Care Study.[381]
7.12
The cost to the Australian
health care system of adverse events in hospitals has been estimated at $867
million per year. Over a five year period this would amount to $4.3 billion.
This estimate does not include any subsequent hospital admissions and
out-of-hospital health care expenses, loss of productivity of the patients
involved, and the long term community costs of permanent disability from AEs.[382] The National Expert Advisory Group
estimated that the extrapolated potential savings from preventable AEs in
1995-96 would be $4.17 billion.[383]
7.13
Regarding overseas comparisons
of AEs, the Australian study found that when expressed as a rate of adverse events
per admission, the rate of hospital admissions associated with an adverse
events was 13 per cent compared to the rate of 3.7 per cent in the Harvard
Medical Practice Study in the United States on which the Australian study was
modelled. The study noted that the considerably higher rate recorded in the
Australian study may have been due to the fact that the US study was concerned
with medical negligence and malpractice, whereas the Australian study focussed
on prevention - which may produce different incentives for the reporting of
AEs. In addition, while both studies surveyed medical records - the US study in
1984 and the Australian study in 1992 - the quality of the medical records may
have improved in the intervening years. These factors suggest that the US study
could have underestimated the AE rate.[384]
7.14
The Committee considers that
the extent of adverse events highlighted in these various studies are
disturbing. The implications in terms of preventable adverse outcomes and the
use of health care resources are substantial, especially as the Quality in
Australian Health Care study suggests that in up to half of all adverse events
practical strategies may be available to prevent them.
Current approaches to quality improvement
7.15
The main quality improvement standard
in the Australian health care sector is the Australian Council on Healthcare
Standards (ACHS) accreditation and quality improvement program. The Council
supports health care organisations in their implementation of quality
improvement; develops and reviews quality standards and guidelines in
consultation with the industry, professional bodies and consumers; benchmarks
clinical care through the collection, analysis and dissemination of clinical
indicators; and advises on health care quality improvement.
7.16
ACHS’ quality improvement
program - the Evaluation and Quality Improvement Program (EQuIP) - is a
continuous quality improvement program that provides a framework for
establishing and maintaining quality care. EQuIP requires an integrated
organisational approach to quality improvement by assisting health care
organisations to improve overall performance; develop strong leadership; and
focus on a culture of continuous quality improvement with an emphasis on
patients and outcomes.[385]
7.17
ACHS conducts surveys of
hospitals and awards accreditation on the basis of the demonstrated ability of
a hospital to demonstrate significant and continuous improvement. Participation
in the accreditation process is voluntary and larger hospitals are more likely
to seek accreditation.[386] As the
table shows, in 1995-96, 40 per cent of public hospitals were accredited,
representing 69 per cent of accredited public hospital beds. In 1997-98, 47 per
cent of public hospitals were accredited, representing 75 per cent of beds in
public hospitals.[387]
Table 7.1:
Accreditation of public acute care hospitals (a)
and average available beds, 1995-96
|
Public
Hospitals |
NSW |
Vic |
Qld |
WA |
SA |
Tas |
ACT |
NT |
Total |
|
Accredited hospitals |
100 |
55 |
25 |
26 |
38 |
3 |
2 |
- |
249 |
|
Non-accredited hospitals |
73 |
60 |
119 |
61 |
37 |
12 |
-
|
5 |
367 |
|
Total hospitals |
173 |
115 |
144 |
87 |
75 |
15 |
2
|
5
|
616 |
|
Proportion hospitals accredited |
58% |
48% |
17% |
30% |
51% |
20% |
100% |
-
|
40% |
|
'Accredited' beds |
13,861 |
9,410 |
4,401 |
3,432 |
3,098 |
1,061 |
769 |
-
|
36,032 |
|
'Non-accredited' beds |
4,300 |
2,787 |
5,567 |
1,439 |
1,653 |
174 |
-
|
570 |
16,489 |
|
Total beds |
18,161 |
12,197 |
9,968 |
4,870 |
4,751 |
1,235 |
769
|
570
|
52,521 |
|
Proportion beds 'accredited' |
76% |
77% |
44% |
70% |
65% |
86% |
100%
|
-
|
69% |
- All
acute care hospitals are included in this table whether or not
accreditation was sought. Hospitals are included in this table for
performance indicator purposes and for some jurisdictions excludes
multipurpose facilities, mothers and babies facilities and dental
hospitals.
Source: AIHW, Australia's Health 1998, Canberra 1998,
p.210.
7.18
There are a number of other
accreditation systems involved in the health care sector including those
related to community health, mental health, aged residential care, and general
practice. In addition, a number of other professional accreditation systems
exist through specialists’ colleges, health professional organisations and the
post graduate medical council.[388]
7.19
At the Commonwealth level there
are a range of activities and initiatives to promote safety and quality of
health care, which attempt to promote a national focus and an integrated approach
to quality and safety. The Department of Health and Aged Care (DHAC) stated
that ‘although the Commonwealth does not have responsibility for the day to day
running of public hospitals, [there]... are examples of where the Commonwealth is
currently working with other stakeholders to support quality and safety
improvement’.[389]
7.20
These initiatives are detailed
below:
-
Australian Council for Safety and Quality in
Health Care - the Council was established in January 2000 to act as a national
partnership between governments, health care providers and consumers to improve
the safety and quality of care. The Council will initiate research and identify
strategies to improve the quality and safety of health services and strengthen
the link between existing quality improvement programs.[390]
-
National Institute of Clinical Studies - the
Institute, which is yet to be established, will work with the medical
profession to identify, develop and promote best clinical practice across a
range of clinical settings, and encourage behavioural change by the medical
profession.[391]
-
Consumer Focus Collaboration - this organisation
was established in April 1997 and is a national body consisting of
representatives from consumer organisations, professional associations, State
and Territory health departments and the Commonwealth. Its aim is to strengthen
the focus on consumers in health service planning, delivery, monitoring and
evaluation. The goals of the organisation is to facilitate the provision of
information to consumers; to facilitate active consumer involvement in health
service planning, monitoring and evaluation; improve health service
accountability and responsiveness to consumers; and promote education and
training that supports active consumer involvement in health service planning
and delivery.[392]
-
National Resource Centre for Consumer
Participation in Health - the Centre became fully operational in May 2000. Its
aim is to assist service providers, such as hospitals, to improve their
strategies for involving consumers in developing their services and practices.
It has two functions, namely as a clearinghouse for information about methods
and models of community and consumer feedback and participation; and in the
longer term as a centre of excellence in consumer participation where clients can
seek assistance to develop, implement and evaluate feedback and participation
methods and models.[393]
-
Clinical Support Systems Project - the Royal
Australasian College of Physicians (RACP) is undertaking a consultancy for DHAC
to focus on the measurement and improvement of clinical care through the
implementation of clinical support systems. The College is working with
innovative and leading clinicians and hospitals to explore whether combining
the use of evidence with a systematic approach to clinical practice results in
more effective and efficient health care with a view to improving patient
outcomes.[394]
-
National Demonstration Hospitals Program - NDHP
is a Commonwealth funded program designed to identify and disseminate
information about best practice models for innovation in acute hospital care.
The effectiveness and transferability of these innovations are evaluated
through demonstration projects conducted in a range of hospitals. Phases 1 and
2 focussed on innovation in internal processes in hospitals to improve patient
care and resource management. Projects in Phase 3 are reaching beyond the
immediate acute care sector and are focussing on identifying and developing
systems and processes that link and coordinate all services delivered by the
acute and related areas of the health sector. [395]
7.21
Further information on these
projects is provided in discussion in this chapter on measures to improve
quality and safety in hospitals.
7.22
In addition to these
initiatives, under the current Australian Health Care Agreements (AHCAs)
approximately $660 million is allocated to the States and Territories to fund
and support quality improvement and enhancement practices in hospitals. This
requires Ministers to agree, on a bilateral basis, to a strategic plan for
quality improvement during the term of the Agreement. Progress under each plan
will be reviewed during the 2000-01 financial year.[396]
7.23
For example, in Queensland a
quality improvement program is being implemented by funding provided under the
AHCAs. Under the program over the period from 1999-2004 major activities to be
undertaken include requiring all services funded or provided by Queensland
Health to have in place quality and continuous improvement systems; ensuring
that all services participate in an endorsed accreditation program;
implementing systems to assess risk, including the monitoring of adverse
incidents and monitoring and evaluating quality performance criteria. The
program also aims to provide relevant information to consumers, which allows
them to make informed decisions regarding their own health and to measure
patient satisfaction and patient experience of health services particularly
with respect to outcomes.[397]
7.24
The Committee notes that there
is no means of knowing if the quality enhancement funds provided by the
Commonwealth are being spent effectively by the States. Under Clause 23 of
Schedule E of the AHCAs, each State and Territory has agreed to provide the
Commonwealth the following reports within five months of the end of each grant
year:
-
a statement to acquit the amount of funds
provided in the relevant grant year as Health Care Grants under the terms of
the Agreements; and
-
a certification that the Health Care Grant
funding received in the relevant grant year was expended on the provision of public hospital services.
7.25
Under Clause 24 of Schedule E,
each State and Territory has agreed that the reports referred to in clause 23
of Schedule E will be in the form agreed with the Commonwealth from time to
time. This acquittal form includes separate identification of components of
Health Care Grants paid to each State and Territory, including for quality
improvements and enhancement.
7.26
However, DHAC cannot provide
details of how each State/Territory has spent its quality improvement and
enhancement funds in the 1998-99 financial year because they are not required
to allocate the quality funding against specific projects or to reconcile this
funding at the end of each financial year. It is therefore not possible to
determine whether the $660 million provided to the States is being used to
drive quality improvements. Unless better financial accountability mechanisms
are put in place the ad hoc and unsystematic approach to quality improvements
in the Australian health care system will continue.
7.27
A range of activities are also
undertaken at the State and Territory levels towards supporting safety and
quality in health care. In NSW the Framework
for Managing the Quality of Health Services in NSW Health was developed in
1998 to provide a comprehensive approach to assessing the performance of Area
Health Services in NSW. The Framework which is currently being implemented on a
State wide basis identifies a number of dimensions of quality relevant to
patients and health providers, in the areas of ‘safety’, ‘effectiveness’,
‘appropriateness’, ‘consumer participation’, ‘efficiency’ and ‘access’.[398]
7.28
In South Australia, the
Department of Human Services has engaged the Australian Patient Safety
Foundation (APSF) to provide service infrastructure and monitoring software for
a comprehensive package to measure risk and the incidence of adverse events and
provide for analysis of these factors. The APSF system has been trialed and is
being introduced across the State.[399]
In Tasmania the State Government indicated that it is developing a comprehensive
quality plan to address adverse events and other quality issues.[400]
7.29
Evidence to the Committee
suggested that current quality improvement programs need to be improved to
reduce the frequency of adverse events. The Royal Australasian College of
Physicians (RACP), Health Issues Centre (HIC) & the Australian Consumers’
Association (ACA), reflecting much of the evidence stated that:
While there have been extensive efforts at Commonwealth, State
and hospital level in relation to quality improvement in hospitals, much of the
effort remains unsystematic and ad hoc.[401]
7.30
The Consumers’ Health Forum
(CHF) also noted that ‘effective quality improvement programs are essential to
reduce preventable injury and death in hospitals. These programs are currently
very ad hoc and “process”, rather than “outcome” oriented.[402]
7.31
Dr Lionel Wilson of Qual-Med
put the view starkly when he stated that:
...few if any such programs exist and those that do are largely
ineffective...Unfortunately, quality management programs barely exist in most hospitals
although sporadic efforts exist to implement a range of quality management
projects. It is this absence of program activity that accounts for the fact
that current activities are quite ineffective in reducing the frequency of
adverse events, or indeed, a wide range of additional quality of care issues.[403]
7.32
Dr Wilson stated that the
overall results of this situation are that ‘no patient in Australia can be
guaranteed high quality of care in any of our hospitals and there are no
worthwhile initiatives to reduce or even identify adverse events in most
hospitals resulting in high levels of avoidable mortality and morbidity’.[404]
Improving quality and safety in public hospitals
7.33
During the inquiry a number of
areas were highlighted where improvements to safety and quality of care in
public hospitals could be made. These issues are discussed below and include a
discussion of the role of the Australian Council for Safety and Quality in
Health Care; the need for improvements in data collection on adverse events, the
need for pilot projects to find solutions to system failures, the role of
financial incentives, improved accreditation processes, improved education and
training for health professionals; encouraging best clinical practice;
promoting greater consumer participation; and the development of performance
indicators.
Australian Council for Safety and Quality in Health Care
7.34
At the August 1999 meeting of
Australian Health Ministers’ Conference all health ministers agreed to
establish the Australian Council for Safety and Quality in Health Care (ACSQHC)
to address the need for a national coordination mechanism to improve
Australia’s health care system and to support action at the local level.[405]
7.35
The National Expert Advisory
Group on Safety and Quality in Australian Health Care (the Expert Group)
recommended in 1999 that the Council be established to improve safety and
quality in health care through:
-
providing national leadership and coordination
of health care safety and quality activities;
-
developing an overall coherent plan for
improving the quality of health care services;
-
facilitating action by dissemination of
information about quality activities and their outcomes through appropriate
agencies and organisations;
-
promoting a systematic approach to safety and
quality within the health care system and within the community at large; and
-
providing advice to Ministers and the public
about the safety and quality of the Australian health care system.[406]
7.36
The Council’s subsequent terms
of reference reflect the recommendations of the Expert Group. The Council’s
stated role is to lead national efforts to promote systemic improvements in the
safety and quality of health care in Australia with a particular focus on
minimising the likelihood and effects of errors. The aims of the Council are
to:
-
provide advice to Health Ministers on a national
strategy and priority areas for safety and quality improvement;
-
develop, support, facilitate and evaluate
national actions in agreed priority areas;
-
negotiate with the Commonwealth, States and Territories,
the private and non- government sectors for funding to support action in agreed
priority areas;
-
widely disseminate information on the activities
of the Council including reporting to Health Ministers and the public at agreed
intervals.
In undertaking these tasks, the Council will:
-
work collaboratively with stakeholders, in
particular building on the existing efforts of health care professionals and
consumers to improve the safety and quality of health care;
-
establish partnerships with existing related
national bodies and organisations, in particular the National Institute of
Clinical Studies (NICS) and the National Health Information Management Advisory
Committee (NHIMAC) to facilitate action in agreed priority areas;
-
consider and act to improve health care in the
priority areas identified as a result of national consultations undertaken by
the National Expert Advisory Group on Safety and Quality in Health Care
including:
-
methods to enable increased consumer
participation in health care;
-
implementation of evidence-based practice;
-
agree a national framework for adverse event
monitoring, management and prevention including incident monitoring and
complaints;
-
effective reporting and measurement of
performance, including research and development of clinical and administrative
information systems;
-
strengthening the effectiveness of
organisational accreditation mechanisms;
-
facilitate smoother transitions for consumers
across health service boundaries; and
-
education and training to support safety and
quality improvement; and
-
co-opt members with specific expertise, and
establish sub-committees and reference groups as required.[407]
7.37
The Council comprises 23
members including experts in the areas of health care quality and safety;
education, training and research; and consumer members. Its membership reflects
the view of the Expert Group that the Council members be appointed from a range
of stakeholders including Commonwealth and State representatives, members of
learned Colleges and professional associations, hospitals and consumer
representatives.[408] The Commonwealth
and the States were asked to nominate members for the Council with the
Commonwealth negotiating with the States on the final list of nominees. All
Health Ministers agreed on the list of nominees for the Council. Mr Bruce
Barraclough, currently President of the Royal Australasian College of Surgeons
and Vice Chair of the Committee of Presidents of Medical Colleges was appointed
Chair of the Council on 21 January 2000. The Council will receive $5 million in
core funding over five years from all governments.[409]
7.38
The Council has identified a
number of key priority areas that need to be addressed. These priority areas
are to:
-
develop a national reporting system for errors
that result in serious injury and death of patients;
-
address medication errors across the system,
including investigating IT support for health professionals;
-
provide support for consumer incident reporting
and feedback - what goes wrong and what
goes right;
-
establish mechanisms to review causes of
preventable deaths and the interventions that would improve practice;
-
establish programs to educate health
professionals across the spectrum - undergraduate and postgraduate - about safe
practice, quality improvement and communication;
-
investigate workforce issues such as skill mix,
supervision and workplace constraints across all professional groups;
-
examine methods of auditing practice to provide
feedback to clinicians about their performance against best practice standards;
-
examine a system to track implanted medical
devices;
-
look at the issue of credentialling and
licensing of health professionals with a view to development of national
standards; and
-
provide support for a national/international
conference on safety and quality in health care.[410]
7.39
It is envisaged that the
Council will initiate a detailed plan of action on these priority areas by June
2001.[411] The Council has identified
three priority areas in which it will focus its efforts in the first instance.
These are improvements in data collection and reporting mechanisms; more
effective ways to support the safe practices of health care professionals; and
re-design of systems to strengthen a culture of ‘safety improvement’ within
health care organisations.[412]
Role of the Council
7.40
Evidence to the Committee
indicated that there was general support for the establishment of the Council.[413] The Committee of Presidents of
Medical Colleges (CPMC) stated that with the establishment of the Council ‘we
have every hope that we will now get quality, particularly in dealing with
adverse events higher on the agenda, and that we will get some effective ways
of dealing with that’.[414] The
Australian Medical Association (AMA) noted that, in supporting the Council,
‘individual doctors and hospitals are putting in an enormous amount of effort
to improve quality, yet it needs a national focus that the Council can give’.[415]
7.41
The Centre for Health Program
Evaluation (CHPE) stated that an important role of a permanent quality
assurance group ‘would be the determination of core measurement and performance
indicators for each sector and specialisation, and the determination of the
validity of these instruments. This suggests the desirability of a capacity to
monitor work in other countries and to run pilot studies in Australia’.[416] The Expert Group envisaged that the
Council would support a number of pilot programs aimed at establishing national
standards and evaluation tools.[417]
The nature and extent of pilot programs undertaken by the Council have yet to
be considered by Health Ministers.
7.42
Professor Jeff Richardson,
Director of the Health Economics Unit, also stated that the Council should be
put under ‘very close scrutiny’ that they are implementing examples from around
the world in regard to best practice medicine.[418] Professor Guy Maddern representing
the South Australian Salaried Medical Officers Association (SASMOA) expressed
the view that while the Council may initiate action at the Commonwealth level
there is a concern that initiatives will ‘not get down to the state level where
in fact most or all of the public hospital dollars are spent’.[419]
7.43
Dr Wilson also added a note of
caution in relation to the Council questioning its composition the breadth of
its expertise. He noted that, while acknowledging the need for such a national
monitoring body on quality issues:
Unfortunately, what has been established is a reflection what I
call the Australian disease: it’s full of state representatives, and in some
case, their role would be to see that nothing changes the status quo in that
state. What is more, apart from some exceptions-notable exceptions-there is a
minimum of expertise on that council because they have been chosen for other
reasons, and this is a complex area and there is little expertise in this
country...What is required of a council like that is not something that
addresses the political difficulties between the federal government and the
states...but one which applies a good deal of expertise to the problem...I have
some hesitation as to whether that council will be terribly effective.[420]
7.44
With regard to composition of
the Council, of its 23 members, nine are representatives of Commonwealth and/or
State and Territory health departments. This indicates that of the total
Council membership some 40 per cent are Commonwealth or State representatives.
The Committee shares the concerns expressed by Dr Wilson that this may be an
overly large representation of government officials, a representation that
would need to be matched by a strong commitment of those representatives to
establish an effective partnership between the Commonwealth, the States and
other key stakeholders to advance safety and quality issues in Australia.
7.45
As to the perceived lack of
expertise on the Council the Committee notes the concerns expressed. The
Committee notes, however, that the Council has a number of noted professionals
and other experts in the area of quality and safety. The Committee does,
however, consider that the composition of the Council and the range of
expertise represented should be kept under review.
7.46
The Council’s lack of formal
links with the health system is also of concern to the Committee. Under the
current structure the Council lacks the ability to make sure its strategies are
implemented across the health care system. The Council can produce reports and
strategies and make recommendations to the Health Ministers but it has no
mechanism to directly drive cultural change and institutional reforms.
7.47
The Expert Group considered
that the Council and its performance should be reviewed prior to the conclusion
its first four year term.[421] The
Government determined that the term of the Council would be five years but did
not put a formal review process in place. The Committee believes that the
Council should be reviewed after two years of operation, and that this review
should consider, among other things any change in the structure and composition
of the Council and the degree to which its aims and objectives are being met.
7.48
Some evidence suggested that
there should be a statutory body established to oversee quality issues. The
Australian Healthcare Association (AHA) argued that the most effective way to
deal with these issues would be to have an independent statutory body at least
to oversee the implementation of the Expert Group’s report.[422] AHA also suggested that while there
are a number of organisations that are involved in various aspects relating to
quality ‘none of them...have the independence, freshness or breadth in their
current brief to be able to do that’.[423]
The Committee sees merit in this proposal and believes that a statutory
authority should be established to oversee the quality programs.
7.49
The Committee has some concerns
at the level of resources devoted to the Council. As noted above, Health
Ministers have agreed to funding of $1 million per year over five years ($5
million in total) for operating costs. The Task Force argued that funding of
$17.4 million ($4.35 million per year over four years from 1999-00) should be
provided, which would allow for a number of targeted research, development and
dissemination activities suggested by the Expert Group (as outlined above).[424] The Council advised that Health
Ministers would consider additional resources for the Council at their meeting
in July 2000.[425] At their meeting,
Health Ministers agreed, in principle, to provide $50 million over five years
for the Council to lead a ‘national program of work to improve the safety and
quality of care’.[426] The Health
Ministers agreed to provide $5 million for a one year work program and the
Council will provide a report to Ministers on progress. Both of these
commitments were in line with the recommendations of the Council in its first
report to Health Ministers.[427]
Further commitment of funds by Health Ministers to the Council will be
dependent on the progress and results of this one year program of work.
Conclusion
7.50
The Committee believes that new
quality funding arrangements that include financial incentives and penalties
linked to agreed national quality targets are required. To be effective the new
funding arrangement would need to be supported by an institutional body or
authority with the capacity to monitor and report on the achievements of
quality and safety outcomes of different health systems. Under the current
system there is no body that oversees quality and drives the required reforms.
7.51
Quality improvements are
currently limited to pilot projects and consequently there is no overall
requirement for the system to commit to quality improvements. Quality
improvements will remain an ‘optional extra’ in our health system until new
funding arrangements are developed and implemented that require specific
quality measures to be built into the entire system.
7.52
The Committee believes that the
Australian Council for Safety and Quality in Health Care has the potential to
place quality improvement high on the national health agenda and to provide the
essential national leadership and coordination of safety and quality
activities. However, under the current funding arrangements State and Territory
health systems are not obliged to adopt the Council’s agenda. The Council’s
work needs to be supported by an independent statutory body that sets quality
improvement targets and reports on their implementation across the different
systems. An independent statutory body would overcome the ad hoc and unsystematic
approach that has characterised quality reforms in Australia. Funding for
quality programs needs to be made more accountable, especially the funds
provided through the AHCAs.
7.53
The Committee considers that
the Council should pursue a vigorous and pro-active program of reform aimed at
improving the quality of health care across the nation and that this program of
reform should be adequately resourced. In this regard, the Committee notes the
recent decision of Health Ministers to provide $5 million to the Council for a
one year program of work. The Committee notes, however, that this is only a
fraction of the funding needed, especially considering that the Taskforce on
Quality in Australian Health Care sought $166.3 million over five years when it
reported in 1996. It is also only a fraction of the total cost to the health
care system of adverse events which has been estimated at $867 million per
year. The Committee is concerned that the Council will require increased
funding to enable it to fulfil its functions. The Committee also notes the very
long time taken for the Government to address the quality agenda. The Taskforce
reported in 1996 but the Council was not established until January 2000.
Recommendation 25: That a national statutory authority be established
with responsibility for improving the quality of Australia’s health system.
This authority would be given the task of:
-
collecting and publishing data on the
performance of health providers in meeting agreed targets for quality
improvements across the entire health system;
-
initiating pilot projects in selected hospitals
to investigate the problem of system failures in hospitals. These projects
would have a high level of clinician involvement; and
-
investigating the feasibility of introducing a
range of financial incentives throughout the public hospital system to
encourage the implementation of quality improvement programs.
Recommendation 26: That the mechanism for distributing
Commonwealth funds for quality improvement and enhancement through the Australian
Health Care Agreements be reformed to ensure that these funds are allocated to
quality improvement and enhancement projects and not simply absorbed into
hospital budgets.
Recommendation 27: That the Commonwealth Government undertake a
review of the structure, operations and performance of the Australian Council
for Safety and Quality in Health Care after two years of operation.
Recommendation 28: That Commonwealth
and State and Territory Health Ministers ensure that the Australian Council for
Safety and Quality in Health Care receives sufficient funding to enable it to
fulfil its functions.
Collection of data on adverse events
7.54
Submissions emphasised the need
for common systems for the collection of information about adverse events and
incidents in Australia. The Australian Health Insurance Association (AHIA)
argued that all hospitals should be required to report incidents to a central
incident reporting system.[428]
7.55
Infections and medication
errors are the two areas that have been identified as the major contributors to
adverse events in several Australian and international reports.[429] Figure 7.1 in this chapter indicates
that data on ‘hospital acquired
infection rates’ are not yet completed and there is no mention in the chart of
data relating to medication errors.
7.56
In the United States in February this year the
US President, Bill Clinton, announced reforms to begin to reduce medication
errors:
I'm calling on the Food and Drug Administration to develop
standards to help prevent medical errors caused by drugs that sound similar or
packaging that looks similar. In addition, we'll develop new label standards
that highlight common drug interactions and dosage errors.
Hospitals that have already taken these steps have eliminated
two out of three medication errors. This is very significant. We tend to think
all our problems are the result of some complex, high tech glitch. We just want
to make sure people can read the prescriptions - two out of three of these
errors can be eliminated.[430]
7.57
The United States report To Err is Human: Building a Safer Health
System recommended:
a nationwide mandatory reporting system should be established
that provides for the collection of standardised information by state
governments about adverse events that result in death or serious harm. Reporting
should initially be required of hospitals and eventually be required of other
institutional and ambulatory care delivery settings.[431]
7.58
A comprehensive system of data
collection on adverse events enables the health system to identify and learn
from errors:
Reporting is vital to holding health care systems accountable
for delivering quality care, and educating the public about the safety of their
health care system. It is critical to uncovering weaknesses, targeting
widespread problems, analysing what works and what doesn't, and sharing it with
others.[432]
7.59
The Committee highlights the
urgency for the infection and medication error framework indicators to be
completed noting that they are necessary to inform the development of national
strategies to address these quality issues. The Committee believes that there
should be mandatory reporting of both medication errors and hospital acquired
infection rates and that these data should be made public.
7.60
There are a number of systems
and methods in place at present to collect information about incidents and
adverse events. These include the systematic audits of registers of death and
selected complications associated with particular procedures or treatments and
the Australian Incident Monitoring System (AIMS). AIMS is an incident reporting
system operated by the Australian Patient Safety Foundation. It is a voluntary
reporting system largely restricted to hospitals in South Australia and the
Northern Territory. Data on adverse events are also collected by the Australian
Council on Healthcare Standards as part of their surveys of facilities for
accreditation purposes.[433] Evidence
to the Committee indicated that these ad hoc attempts at data collection could
be improved by implementing a system aimed at collecting comprehensive and
consistent data across all hospitals nationally.[434]
7.61
The Expert Group argued that
systems need to be put in place to support the efficient collection of
incidents and adverse events - ‘these systems need to be simple, usable, robust
and must not add significant administrative burdens to those involved in their
use’.[435]
7.62
Several submissions called for
the establishment of a nationally consistent adverse incident reporting scheme.[436] The Expert Group also argued that
there was a need for State and Territory Governments, health care organisations
and other agencies involved in collecting data on incidents, adverse events and
complaints to agree on common systems for efficient collection and reporting
data on adverse events, with the capacity for national analysis of safety and
quality trends.[437]
7.63
The Committee notes that the
Australian Council for Safety and Quality in Health Care has set as one of its
priorities the development of a national reporting system for errors that
result in serious injury and death of patients in the health care system.[438] The Committee strongly supports the
adoption of a uniform national approach to this problem as both necessary and
long overdue.
7.64
The Committee believes that the
national statutory authority could play an important role in overcoming the
current ad hoc approach and in establishing a national system of data
collection and reporting.
Recommendation 29: That a mandatory reporting system,
especially for hospital acquired infection rates and medication errors, be
developed as a matter of urgency.
Pilot projects
7.65
Submissions identified the need
for pilot studies with system wide application to find solutions to the system
failures which have been identified in the various studies of adverse events
both in Australia and overseas.[439] In
most studies of hospital systems, some form of system failure, for example, the
absence of, or failure to use policy, protocol or plan; inadequate reporting;
or inadequate training or supervision of staff is usually judged to be a
contributing factor in up to 90 per cent of cases of adverse events.[440]
7.66
Dr Wilson noted that most quality problems in
hospitals are not about individuals making mistakes but are due to system
failures. He added:
This is what happens when things do wrong in hospitals. The
person in charge of theatre was not there that day; someone else was there who
did not know the routine. The theatre team was new. The surgeon was not well or
had been up all night. A whole series of events go wrong. It is not just about
an individual misbehaving or behaving badly, or very rarely it is. It is mainly
a system failure.[441]
7.67
Dr Wilson further stated that:
Implementing effective quality management that ensures real
quality improvement, needs to be done slowly in a small number of facilities
with carefully managed and monitored pilot projects. Such projects will require
resources and will need to be evaluated to ensure that they are producing value
for money.[442]
7.68
CPMC noted that clinician
involvement in identifying and implementing solutions is crucial in any reduction
in the frequency of adverse events.[443]
The Committee notes that the Medical Colleges have indicated to the Department
of Health and Aged Care that they are ‘willing to take a leadership role in
these activities’.[444]
7.69
The Committee believes that the
problem of system failures in hospitals needs to be addressed and that pilot
projects to investigate this problem should be undertaken by the new statutory
authority. The Committee also believes that the connection between system
failure in hospitals and cultural change needs to be addressed. The Australian Council for Safety and Quality
in Health Care stated that there is a need for creating ‘changes in the culture
in which health professionals work from one of “judgement and blame” to one of
“learning for quality improvement”’.[445]
This cultural change will require more than just pilot projects, it will
require national leadership to implement findings on a national scale.
Recommendation 30: That the new statutory
authority to oversee quality programs initiate pilot projects in selected
hospitals to investigate the problem of system failures in hospitals and that
these projects have a high level of clinician involvement (see Recommendation
25).
Recommendation 31: That the issue of
cultural change within the hospital system be addressed, particularly the
capacity for improvements in information technology to drive change through
greater transparency and the adoption of consistent protocols.
Financial incentives
7.70
Evidence suggested that there
is a serious lack of financial incentives throughout the health system that
will promote quality of care. CHPE stated that:
The key issue is the lack of any reward under current payment
arrangements for the achievement of high quality care...The full potential of
financial levers is not explicitly recognised. In principle, a system committed
to quality improvement would embody incentives to achieve this objective at all
levels.[446]
7.71
Professor Richardson commented
that ‘when you change incentives and financial incentives you will actually
change behaviour. That behaviour change, usually with a time lag, is followed
by some sort of institutional change...there are any number of studies now from
any number of countries - primarily, the United States - which illustrate that
financial incentives do have a major effect’.[447]
7.72
Dr Wilson stated that:
There are no drivers at all for quality management in health
care. It is continually assumed that, if you have well-trained people, that is
enough. It is important, but it is not nearly enough, not in today’s world. So
that is the next thing: drivers. And they probably have to be financial drivers
because they are the most potent.[448]
7.73
A number of options were
suggested to address the issue of the lack of financial incentives. In the area
of private health insurance, AHIA suggested that the default payment should be
linked with quality criteria, that is, hospitals should not automatically be
entitled to benefits without meeting some degree of quality assurance, such as
the implementation of a recognised quality improvement program.[449] The Australian Private Hospitals
Association (APHA) argued that hospitals offering quality services should be
rewarded by insurers through financial incentives, in the form of higher
benefits.[450]
7.74
CHPE suggested that one option
would be to reduce default payments (preferably to zero) for non-participating
hospitals. The health insurance funds should be permitted to base their
selection of preferred providers on explicit performance indicators of quality
and be permitted to publicise what and why they have selected particular
providers.[451]
7.75
With regard to public
hospitals, Dr Wilson argued that financial drivers need to be applied to
hospital boards and management, who should have prime responsibility for
quality management and improvement programs. As noted above, he argued that at
present there are no incentives for a hospital managers to undertake the steps
necessary for ‘quality management’. ‘Quality management’, as discussed
previously, is a general term used to describe a range of hospital activity
which aims to produce a quality mature hospital. It includes activities such as
risk management, quality assurance and credentialling of medical staff. Dr
Wilson stated that the introduction of financial incentives available to
hospital managers who implement a stated range of quality management activities
that are verifiable within a certain timeframe, combined with a financial
sanction for failing to achieve designated goals, would substantially improve
quality and safety in hospitals.[452]
7.76
CHPE also suggested that the
use of ‘normative DRGs’ and other penalties/rewards should be explored. With
these, the cost weight per DRG would have a deterrent or reward loading which
could reflect under or over used procedures; origin of the patient in an over
or under serviced geographic location; the receipt of services from an
accredited hospital; and some other quality related activity such as discharge
planning and follow-up service.[453]
7.77
In relation to doctors, CHPE
argued that accreditation may be linked to a differential fee. This could be
extended so that a loading was added to fees when doctors indicated their
compliance with broad evidence based guidelines. The extent of their commitment
could, potentially, be monitored using routine administrative data.[454]
7.78
The Committee believes that the
new statutory body should explore the use of financial levers to encourage
improved quality of care in the hospital setting.
Recommendation 32: That the new statutory authority overseeing
quality programs investigate the feasibility of introducing a range of
financial incentives throughout the public hospital system to encourage the
implementation of quality improvement programs (see Recommendation 25).
Accreditation processes
7.79
A number of submissions argued
that there should be improved linkages and coordination between the range of
current accreditation and quality improvement approaches, in order to minimise
duplication and confusion for health service organisations regarding expected
standards of care. In the joint submission of the Australian Healthcare
Association (AHA), Women’s Hospitals Australia
(WHA) and the Australian Association of Paediatric Teaching Centres
(AAPTC) it was noted that in addition to the Australian Council on Healthcare
Standards there are now a number of other accreditation systems involved in the
health care sector including those related to community health and aged
residential care. A number of other professional accreditation systems also
exist through specialists’ colleges and health professional organisations.[455]
7.80
The Queensland Nurses’ Union
(QNU) raised the issue of how these separate processes interrelate and whether
there is a need for an ‘overarching framework’ that will facilitate the
involvement of all key stakeholders in activities relating to continuous
improvement in health - ‘we believe that better integration is required to
facilitate consistency of approach with respect to these matters’.[456] The Australian College of Health
Service Executives (ACHSE) expressed a similar view.[457]
7.81
ACHSE argued for the
establishment of an accreditation authority for all health services. The
authority would need to be independent of the funding authority and ensure that
there was effective stakeholder and consumer involvement.[458] AHA, however, arguing against the
creation of a national accreditation body stated that:
I think accreditation is part of the overall process of managing
risk and improving quality. I do not think it is the total answer to quality
and safety so I do not necessarily think a national accrediting body could take
responsibility for quality. However, I think an authority that has
responsibility for safety and quality could certainly have a look at the
plethora of accrediting bodies that are in place at the present time.[459]
7.82
AHA, WHA & AAPTC argued
that the Commonwealth and State Governments should collaborate in the
establishment of a national accreditation process for all types of health care
facilities.[460]
7.83
Submissions also noted that
accreditation currently focuses on quality control ‘processes’, that is, it has
a strong input focus. The Australian Nursing Federation (ANF) argued that to
strengthen its capacity to bring about significant reductions in the frequency
of adverse events, accreditation criteria ‘must be comprehensively linked to
the achievement of desired health outcomes’.[461]
AHA also stated that accreditation systems should move beyond the inputs,
processes and simple indicators of the quality of products to an approach that
is multidisciplinary in its focus to better reflect the nature of contemporary,
best practice care delivery systems.[462]
7.84
Some submissions also argued
that there was a need for more consistent national standards to underpin
quality improvement and accreditation approaches. Professor Don Hindle of the
School of Health Services Management at the University of NSW advocated the
‘adoption of national standards for quality of care and outcome measurement’.[463] AHA, WHA & AAPTC stated that the
proliferation of different standards for the same type of facilities, and of
different ways of measuring the same features in multiple settings is a major
concern of the Associations.[464] The
Expert Group noted that a first step should be to facilitate discussion and
debate about the underlying quality standards that should be key elements of
all quality improvement approaches.[465]
Recommendation 33: That the Australian Council for Safety and
Quality in Health Care review the current accreditation systems currently in
place with a view to recommending measures to reduce duplication in the
accreditation processes.
Education and training in quality improvement
7.85
Submissions argued that the
education and training available for health professionals and administrators at
all levels in quality improvement needed to be improved. ACHSE argued that:
greater emphasis and investment in education and training in the
philosophy and techniques of quality and safety are required for managers and
all health professionals. This will enable improved approaches to be
established effectively and new accountabilities to be met.[466]
7.86
The Australian Association of
Surgeons (AAS) argued that while formal quality improvement programs may
decrease the frequency of adverse events educational activities are usually
more cost effective.[467] The Doctors
Reform Society (DRS) also argued that quality improvement programs should be an
integral part of the on-going education of all medical practitioners.[468]
7.87
The Expert Group considered
that there would be benefits from the development of core quality management
aspects to be incorporated in all educational training provided to all health
professionals, whether they are being trained for clinical or administrative
roles. The Group also argued that there needs to be a national effort to
improve the education and training of health providers in safety and quality
matters and agreement on the curricula for continuous quality improvement for
inclusion in all undergraduate, postgraduate and continuing education and
training.[469]
7.88
The Committee notes that the
Australian Council for Safety and Quality in Health Care has identified as a
priority area the establishment of undergraduate and postgraduate programs to
educate health professionals about safe practice and quality improvement.[470] The Committee supports this
initiative noting the concerns expressed in evidence about the need for
improvements in the education and training of health professionals in the areas
of safety and quality.
Encouraging best clinical practice
7.89
Evidence to the inquiry called
for the uptake of evidence-based health care and the further development and
implementation of best practice guidelines.[471]
‘Evidence-based health care’ is an approach to health care based on a
systematic review of scientific data. ‘Best practice’ in the health sector
refers to the highest standards of performance in delivering safe, high quality
care, as determined on the basis of available evidence and by comparison among
health care providers.[472]
7.90
The National Health and Medical
Research Council (NHMRC) stated that there has been an increasing move towards
developing clinical best practice guidelines.[473]
‘Clinical practice guidelines’ are systematically developed statements to
assist providers and users of health services to make decisions about
appropriate health care for specific circumstances. The purpose of best
practice guidelines is to improve the quality of health care, to reduce the use
of unnecessary, ineffective services or harmful interventions and to ensure
that care is cost effective. The NHMRC has been primarily responsible for the
development and implementation of clinical practice guidelines to assist health
care providers implement research into practice. There is also an increasing
trend for other expert bodies and the learned Colleges and professional
associations to develop clinical practice guidelines for endorsement by the
NHMRC. Most States have also invested in clinical effectiveness units to
promote evidence-based healthcare and to link research with local practice.[474]
7.91
NHMRC noted that with the
development of evidence-based medicine, guidelines are becoming one of the
critical links between the best available evidence and good clinical practice.[475] The guidelines are intended to be a
distillation of current evidence and opinion on best practice. Clinical
practice guidelines are sometimes referred to as clinical pathways, protocols
and practice policies, although these differ from clinical practice guidelines
in that they are often much more prescriptive and not always based on evidence.[476]
7.92
Quality assurance and quality
improvement activities have a complementary and reciprocal relationship with
clinical practice guidelines. Quality assurance activities encourage the
implementation of guidelines, and guidelines are a crucial component of quality
assurance activities. Continuous clinical practice improvement aims to improve
the quality of care by bringing together research on variation of cost, access,
quality and standardised care. It requires a knowledge of processes and
systems, human behaviour and an approach to continuous learning.[477]
7.93
During the inquiry witnesses discussed
aspects of these approaches. For instance, RACP supported the development and
implementation of clinical practice guidelines and evidence-based medicine.
RACP stated that it is currently undertaking the Commonwealth-funded Clinical
Support Systems Project (CSSP), an initiative which focuses on the measurement
and improvement of clinical care through the implementation of clinical support
systems. Such systems include clinical practice guidelines, clinical pathways,
consumer pathways and information technology for clinical decision support and
measurement of health outcomes. It is an approach that links clinical practice
improvement directly to medical evidence and aims to improve the efficiency and
quality of health care provision.[478]
7.94
Professor Hindle advocated the
clinical pathways approach. A clinical pathway is a document which describes
the usual way of providing multidisciplinary clinical care for a particular
type of patient, and allows for annotation of deviations from the norm for the
purpose of continuous evaluation and improvement. He agued that good clinical
teams in Australia and overseas are increasingly using clinical pathways.[479] He argued that:
Good clinicians want to work in teams. They want to specify how
they will work together...so it is sensible to write down the protocol for what
they will normally do. They are making these changes around Australia as we
speak because they recognise that it will help them allocate their scarce
resources-they won’t waste resources on that patient when they are better spent
on another of their patients. They will improve quality of care and outcomes by
avoiding duplication of care or missing out on care and so on.[480]
7.95
Professor Hindle argued that evidence from
around the world shows that clinical pathways improve quality of care and
reduce costs because the team works better, thus avoiding omission, duplication
and other errors. He suggested that the main barriers to the use of clinical
pathways are that some clinicians are reluctant to work in a team, or are concerned
to avoid anyone else being aware of, and consequently in a position to
criticise, their clinical practice.[481]
7.96
The Expert Group argued that
existing efforts to promote evidence-based practice through such groups as the
learned Colleges and NHMRC should continue to be supported by all
jurisdictions, Colleges and other relevant groups, and that this work should
form part of an overall national action plan for safety and quality
enhancement. The Expert Group considered that the focus on evidence-based care
should also be underpinned by a commitment to continuous quality improvement in
clinical practice. The Group also argued that national action should continue
to be taken to research, develop and encourage implementation of evidence-based
practice, including use of clinical practice guidelines and quality improvement
tools that reduce unexplained variation and improve aspects of quality across
the continuum of care.[482]
7.97
Some evidence indicated that
the development of clinical practice guidelines by the Colleges has been
relatively slow. Professor Richardson indicated that while a number of the
Colleges are investigating evidence based medicine the pace of reform is
‘leisurely’ in relation to the importance of the issue.[483] The Menadue report into the NSW
health system also commented on the slow development of clinical practice
guidelines by most of the Colleges, with some notable exceptions.[484] The Committee is concerned at this
development and encourages the learned Colleges to further facilitate the
development of clinical practice guidelines.
7.98
NHMRC also stated that there
needs to be greater attention given to implementation and evaluation of
guidelines once they have been developed. NHMRC noted that many of those
involved in producing guidelines have become frustrated by the lack of
implementation. Further, health care professionals’ acceptance of clinical
practice guidelines has to some extent been marred by concern that the
guidelines represent ‘cookbook’ medicine.[485]
One study suggested that there were marked variations in the uptake of
evidence-based methods among different practitioners in different fields of
medicine - the fields that have a higher reliance on technology, such as
neonatology, appear to adopt evidence-based practice styles more readily.[486]
7.99
The Committee notes the
proposed establishment of the National Institute of Clinical Studies. As noted
previously, the role of the Institute is to promote best clinical practice
throughout the public and private health sectors and encourage behavioural
change by the medical profession. The Committee notes that the Institute was
due to begin operations in January 2000.[487]
The Committee is disappointed at the delay in the establishment of the
Institute given its potential importance in promoting best clinical practice.
7.100
The Committee notes that
several witnesses stressed the importance of the Institute in addressing the
issue of best practice medicine. Professor Donald Cameron representing the RACP
stated that the Institute will be ‘looking at outcomes -clinically significant
outcomes, not the sort of thing that has happened in the past like some
satisfaction surveys which usually ask if the doctor was polite and nice and so
on’.[488] Professor Peter Phelan
representing the CPMC stated that the Institute would assist in promoting best
clinical practice:
There are considerable variations in medical interventions
across the community...they occur because there is not good evidence on which
these interventions are based, so doctors use their own experience. We have not
been able to provide them with information to allow them to make more informed
judgements. I think the initiative to establish a national institute of
clinical studies may well start to provide that sort of information to doctors
which can make them more informed.[489]
7.101
The Committee supports the
further development and implementation of evidence-based medicine and of
clinical practice guidelines. The Committee believes that a firm commitment to
evidence-based medicine will promote best practice and improve the quality of
health care.
Recommendation 34: That initiatives by the National Health and
Medical Research Council, the Colleges and other relevant groups to encourage
the development and implementation of evidence-based practice, including the
use of clinical practice guidelines, be supported.
Consumer participation in quality improvement
7.102
Evidence to the Committee from
consumer organisations highlighted the need to improve consumer participation
in the development of quality improvement programs and the health system generally.
Mr McCallum representing the Consumers’
Health Forum of Australia (CHF) stated that there was a need to:
...strengthen individual consumers and communities to think more
about the care they need, to make better choices about the care they access and
to become partners with the health system. It worries me that we will craft
solutions that will not involve the consumers and communities who might have
solutions for us in this.[490]
7.103
The CHF outlined a number of
requirements that they see as essential to any quality improvement program to
reduce adverse events. CHF argued that consumers should:
-
have access to their own medical records -
‘medical records are still one of the most important sources of information for
consumers trying to make sense of an adverse event’;
-
have access to effective information to help
consumers understand their treatment options;
-
have access to effective complaints mechanisms;
-
be informed when a mistake has been made or an
accident occurred as a result of the failure of the system, or of a medical
practitioner; and
-
participate in all levels of the health system.[491]
7.104
RACP, HIC & ACA also argued
that to promote a high quality public hospital system there needs to be
investment in better systems to promote ‘consumer-oriented care’. This includes
attention to best practice, clinical practice supports and protocols, the
measurement and analysis of variations in practice and health outcomes
measures.[492]
7.105
The Expert Group argued that
national action should continue to be taken to research, develop and
disseminate methods to enable better consumer participation in health care
service delivery, planning, monitoring and evaluation at all levels, including
strategies to improve the quality and accessibility of consumer health
information.[493]
7.106
DHAC stated that the
Commonwealth is working with consumer organisations, health service providers
and State/Territory Governments to increase consumer participation in the
planning, delivery and evaluation of health care. As noted previously, the
Consumer Focus Collaboration aims to improve the accountability and
responsiveness of the health care system to consumers.[494] The Collaboration is overseeing some
14 projects funded through the Commonwealth. These projects include:
-
Consumer and Provider Partnerships in Health
project - the aim of the project is to document the most effective approaches
available for teaching and learning the skills needed for effective
communication between health care consumers and providers. The consultant
undertaking the project will analyse the issue of education and training in
health care to promote active consumer involvement in health system planning
delivery and monitoring and evaluation.
-
Project to support nurses to involve consumers
in their own health care - the ANF and the Royal College of Nursing Australia
have been funded for a project to develop strategies to support nurses in
involving consumers in health care planning and delivery. A similar project
involving the AMA and the CPMC is undertaking a project to work with medical practitioners
to support their efforts to involve consumers in their health care.
-
Structural and Cultural Marginalisation in
Health Care project - the aim of the project is to identify ways that health
services have involved or sought feedback from groups of consumers who have
been excluded from existing processes due to structural or cultural barriers.
-
Toolkit for consumer participation - the aim of
the project is to provide a practical toolkit of approaches and strategies to
assist service providers and consumers to achieve effective consumer
participation in the planning, delivery and monitoring of health services.[495]
7.107
Many of these projects are
close to finalisation but there is only one published report available to date
on these projects. The results of individual projects are to be made available
to the National Resource Centre for Consumer Participation. As noted
previously, the Commonwealth has funded the National Resource Centre for three
years. It is being established to assist health service providers to improve
their strategies for involving consumers in the development of services and
will act as a clearinghouse for information on methods and models of community
participation in health care.[496]
7.108
At the State level, in NSW the
Menadue report argued that action was needed in that State to improve consumer
involvement in decisions about health care. The report argued that there needed
to be increased consumer access to information. The report recommended that NSW
Health establish a 24-hour Health Call Centre with full coverage across the
State; and that a health care Internet site be established to provide
information which supports the advice available through the Health Call Centre.
The NSW Government subsequently accepted these recommendations.[497]
7.109
The Menadue report also called
for expanded opportunities for local communities to participate in decisions
about the type and location of health services. The report proposed that formal
structures for ongoing community participation be established in each Area Health
Service. In addition, the report argued that there should be greater
involvement of consumer representatives in identifying health priorities at the
State level through the establishment of a State-wide Consumer and Community
Representative Forum to provide advice on planning, policy development and
resource allocation at the State level.[498]
The NSW Government announced that it will establish a Statewide consumer forum
to provide input to decision-making on policy and resource allocation. [499]
Report cards
7.110
Some submissions argued that
‘report cards’ on hospitals and medical practitioners should be published so
consumers can make informed choices concerning their treatment options. The
Health Consumers’ Council WA argued that hospital report cards ‘would ensure
greater knowledge of and confidence in our public hospital system. Data should
be collected and analysed to support the report card concept’.[500] CHF also argued that consumers need
more information on risks, benefits and options for treatment from their health
care providers as a basis for decision making. CHF stated that reliable,
independent information from sources other than the medical professional
administering the treatment is also needed.[501]
7.111
The medical profession
generally opposed the publication of league tables or report cards arguing that
they are not reliable indicators of performance or best practice.[502] AMA argued that there are
considerable difficulties in interpreting data based on report cards:
...the more competent, senior experienced surgeons are likely to
see the more difficult end of the spectrum and, amongst them, their death rates
may be higher because, for instance, they may be operating, especially in a
tertiary hospital, on patients that a surgeon at a peripheral hospital would
not touch. That is really the problem about report cards on both hospitals and
individual doctors.[503]
7.112
AMA (Victoria) argued that
current data collections and risk adjustment tools are poorly developed and
inadequate for the publication of comparative performance indicators for
hospitals and individual medical practitioners.[504]
7.113
The Committee questioned the
AMA concerning the current situation where a GP refers patients to a specialist
about which the patient as a consumer probably has little knowledge as to his
or her medical competence and therefore is not in a good position to make an
informed judgement concerning the surgeon. Dr Sandra Hacker, former Vice
President of the AMA conceded that the current situation is ‘not particularly’
satisfactory.[505] Dr David Brand,
former President of the AMA, added that ‘I would agree that the public has a
right to know, but it has a right to know about information where it can
compare - if you are going to compare apples with apples you have got to be
comparing apples with apples. That is something that is very difficult to do’.[506]
7.114
The Committee believes that
consumers should have access to information on the relative performance of
hospitals and the performance of individual providers so that they can make
informed choices about their treatment options. The Committee is not convinced
by the arguments advanced by the medical profession that because data are
supposedly inadequate for the dissemination of reliable comparative performance
indicators for hospitals and medical practitioners it therefore should not be
made available. The Committee believes that this is more an argument for
improving upon the current data than for not providing such information to
consumers.
Conclusion
7.115
The Committee believes that
there needs to be greater consumer involvement in the health system generally,
including the provision of health information to consumers and consumer
participation in health care service delivery and planning. The Committee
commends the initiatives at the Commonwealth and State level to encourage
consumer participation in the health system. The Committee further believes
that measures that encourage consumer involvement in the health area need to be
encouraged and expanded.
Recommendation 35: That strategies be developed to improve the
provision of health information to consumers, improve the accountability of the
health system to consumers by the release of information and comparable data
and increase consumer involvement in the health system, including consumer
participation in the development of quality improvement programs.
Performance measurement
7.116
Submissions argued that there
needs to be greater priority given to the development of performance indicators
and health outcome measures.[507] CHPE
stated that:
There is a need for the establishment of national performance
indicators for public hospitals and associated services, including inpatient,
outpatient and emergency department services. These performance indicators
could be used for comparative purposes across institutions relating to efficiency,
clinical outcomes and quality.[508]
7.117
DHAC indicated that data about
quality of care and health outcomes are piecemeal at present - ‘different parts
of the hospital systems collect a great range of data...However the data is often
haphazardly collected and there is little analysis of anything but information
relating to financial requirements. The use of data to improve performance in
the clinical area is at a very low level while data for system-wide analysis is
unreliable and poorly articulated and collected’.[509]
7.118
The Expert Group argued that
rigorous and reliable indicators for the measurement of safety and quality
performance are required at all levels of the health system and that joint
funding and support for national research and development of performance
information and indicators for health care quality are critical to continued
efforts in this area. The Expert Group argued for the development of a national
framework for performance management and reporting for all health services.[510]
National health sector performance
measures
7.119
In 1994 the National Health
Ministers’ Benchmarking Working Group was established to coordinate and report
on the development of national health sector performance indicators and
benchmarks. In August 1999 the Australian Health Ministers established the
National Health Performance Committee (replacing the National Health Ministers’
Benchmarking Working Group). The Committee, which has similar objectives to the
previous Committee, aims to develop and maintain a national performance measurement
framework for the health system, to support benchmarking for health system
improvement and to provide information on national health system performance.
7.120
The new Committee will have a
broader focus covering the whole of the health sector, including community
health, general practice and public health. The membership of the Committee
includes representation from each State and Territory and the Commonwealth
together with representatives from other national bodies such as the NHMRC and
the Australian Institute of Health and Welfare (AIHW).[511]
7.121
A number of other groups are
working in the area of performance measurement and related activities. These
include the Australian Council on Healthcare Standards, Australian Institute of
Health and Welfare, individual health authorities, universities and other
government authorities.
7.122
The terms ‘performance
indicators’ and ‘benchmarking’ are often used interchangeably even though they
deal with different but related concepts. A ‘performance indicator’ is a
measure that quantifies the level of performance for a particular aspect of
health service provision and allows comparison between service providers, modes
of service provision or both. ‘Benchmarking’ can be defined as the continuous
process of measuring products, services and practices against the best
available in the relevant area. The process examines attributes of performance
(indicators) in comparing individual units or organisations against standards
(benchmarks) that are considered attainable and desirable. The process by which
data are collected and collated can be defined as the process of performance
measurement. The Benchmarking Working Group has essentially focussed on the
development of performance indicators and the process of performance
measurement. [512]
7.123
The Working Group’s 1999 report
provides details of a framework of performance indicators for public hospitals
with an emphasis on those indicators of most relevance in gaining a ‘holistic’
view of the performance of the public hospital sector.
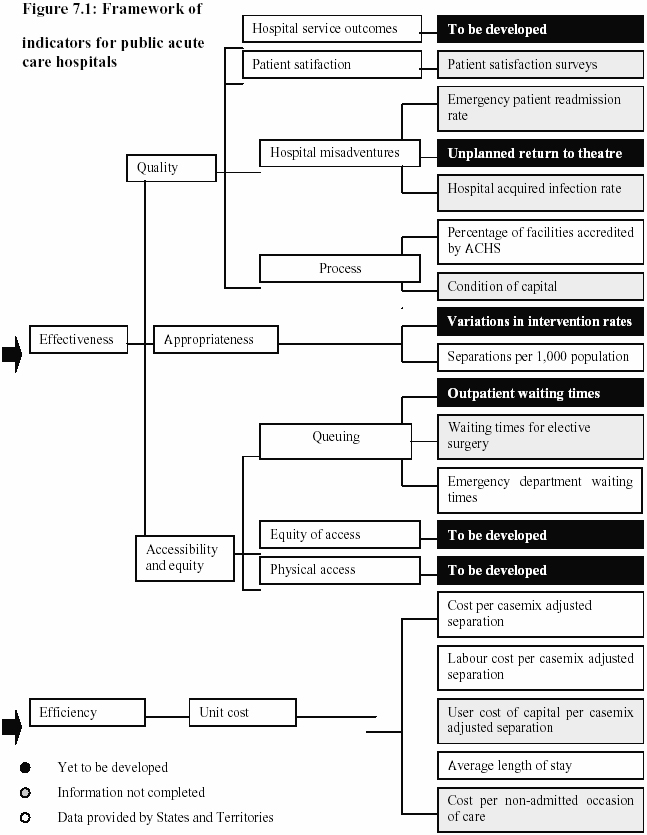
Source: National Health
Ministers’ Benchmarking Working Group,
Third National Report on Health Sector Performance Indicators, June 1999,
p.7.
7.124
As indicated in the table while
some performance indicators are provided by the States and Territories a
significant number of indicators have yet to be developed or the information is
incomplete. The report notes that comprehensive data that can fully investigate
the two dimensions of ‘effectiveness’ and ‘efficiency’ are ‘not yet available.
Available data for reporting against the indicators...are, therefore, limited to
a subset of the framework’.[513]
7.125
The Queensland Nurses Union (QNU), referring
to the above table, stated that while the data give some indicators for public
acute care hospitals they are far from complete:
...when you look at the indicators you see that they state that
hospital service outcomes are to be developed. Under quality outcomes and
hospital misadventures, you see there is no development of anything for
unplanned return to theatre. We are not assessing the number of patients who
are discharged who need to be returned to theatre. In terms of appropriateness
of health care, there is no assessment of variations in intervention rates. ...If
you look at queuing, there is some work being done on outpatient waiting times
but it is not fully developed. If you look at accessibility and equity, you see
that equity of access is still to be developed. Physical access is still to be
developed. A heck of a lot of indicators
which would tell you whether the system is working are not even developed yet.[514]
7.126
The Working Group’s report
noted that several barriers existed in further development of national
benchmarking including the complexity of some of the measurement issues; the
lack of coordination across jurisdictions; and the time required to establish
and implement national data standards. The report argued that ‘the
establishment and implementation of national data standards, which are
imperative for national benchmarking, will continue to be a slow and difficult
process’.[515]
7.127
The Committee believes that a
much more concerted effort should be made to develop performance indicators in
the health sector, especially given that a national working group has been
established since 1994 with the specific aim of developing national performance
indicators for the health sector. The Committee believes that the slow progress
to date in the development of national benchmarking points to the need for the
establishment of an independent statutory body to drive reforms in the area of
quality improvement. It is clear that the current system is too slow and that a
new approach is needed.
Performance measures - State level
7.128
In the States a range of
activities have been initiated in developing and implementing performance
measures. As noted earlier in the chapter, in NSW the Government has developed
a performance measurement framework for Area Health Services that encompass
indicators such as effectiveness, efficiency, safety and access.[516] The Menadue report also recommended
that comparative data for all NSW hospitals, on factors such as admission
rates, readmission rates, mortality rates and surgical intervention rates for
the major planned surgical procedures, should be included on the NSW Health
information website within 12 months.[517]
The NSW Government subsequently announced that health data and information on
treatments will be included on the NSW Health internet site.[518] In Victoria, the Government will
require the Department of Human Services to publish a series of performance
indicators by July 2001 to assess quality of care in public hospitals.[519]
Performance measures - AHCAs
7.129
The AHCAs also commits the
Commonwealth and States to work together to develop and refine performance
indicators and to publish information on performance against the indicators to
demonstrate whether overall funding is contributing to better health outcomes.
The objective in publishing this information is to enable the Commonwealth and
the States to compare performance within the acute health sector in order to
stimulate improvement in service performance and health outcomes; improve
national and State acute health development; and facilitate best practice
service delivery.[520]
7.130
A report on progress towards the development
of performance indicators will be included in the first AHCA annual report due
to be published in December 2000.[521]
Conclusion
7.131
The Committee believes that
there needs to be a coordinated effort by the Commonwealth and States to
develop a framework of indicators for the public hospital sector so that a
comprehensive set of performance indicators is available across all States for
comparative purposes.
7.132
The Committee notes that the
National Health Performance Committee is working in this area but that progress
has been relatively slow with several key indicators for public acute care
hospitals yet to be developed. The Committee also notes that the States are
also developing performance measures and that the implementation of the AHCAs
also provides for reporting against a range of the performance indicators
developed jointly by the Commonwealth and the States. As noted in this chapter,
the first report is yet to be released some 2 years after the Agreements
commenced. The Committee believes that the delay in the release of data on
comprehensive performance indicators, as provided for under the AHCAs, is
unsatisfactory and their release should be a matter of high priority. The
Committee also believes that there needs to be a high degree of co-ordination
between the various bodies at the Commonwealth and State level in order to avoid
duplication in the collection of data and in the development of performance
indicators.
Recommendation 36: That the Commonwealth work with the States
and Territories to develop a comprehensive set of national performance
indicators in relation to quality issues for the public hospital sector,
including the range of performance indicators as provided for under the current
AHCAs, and that this information be released publicly as a matter of priority.
Recommendation 37: That the development of a comprehensive set
of national performance indicators be the responsibility of the new statutory
authority (see Recommendation 25).
Conclusions - strengthening the commitment to quality
7.133
Evidence received by the
Committee suggests that while the quality of care in public hospitals is
generally of a high standard, more attention needs to be given to quality
improvement programs to reduce the frequency of adverse events and improve the
overall quality of care.
7.134
Patient safety clearly must be
an essential element of health care quality and accorded the highest priority,
notwithstanding the fact that all healthcare interventions have some potential
for risk. As noted previously, the Quality in Australian Health Care Study
showed that 16.6 per cent of hospital admissions in 1992 were associated with
an adverse event and that at least half of the adverse events were judged to be
preventable. The extent of adverse events identified in this study and others
clearly requires a concerted national effort to address safety and quality
issues in the hospital setting.
7.135
While there have been numerous
efforts at the Commonwealth, State and hospital level in relation to quality
improvement in hospitals, evidence to the Committee indicated that much of the
effort to date has been largely ad hoc and unsystematic. The Committee believes
that a commitment to further quality improvement requires concerted national
leadership by the Commonwealth and a firm commitment by the Commonwealth and
the States and other key stakeholders to work together to improve the quality
of health care services.
7.136
The Committee believes that the recent
establishment of the Australian Council for Safety and Quality in Health Care
has the potential to provide the necessary national focus on safety and quality
issues and to promote a systematic approach to these issues in the health care
system. The Committee believes that the Council must be proactive in pursuing a
reform agenda and be adequately resourced to address key areas of concern, and
to provide essential national leadership and coordination.
7.137
The Committee has identified a
number of key areas for reform. These areas include:
-
the establishment of a national statutory
authority with responsibility for overseeing the quality programs;
-
the establishment of pilot projects to find
solution to system failures identified in various studies of adverse events;
-
establishment of a system of financial
incentives throughout the health system to promote quality of care;
-
improved linkages and coordination between the
range of current accreditation and quality improvement approaches;
-
improved education and training for health
professionals and administrators in quality improvement;
-
measures to encourage best clinical practice;
-
greater consumer participation in quality
improvement programs; and
-
development of performance indicators and health
outcome measures.
7.138
The Committee believes that a
systematic and multifaceted approach to safety and quality issues and active
national leadership together with the fostering of an effective partnership
with State Governments and other key stakeholders will promote an environment
where quality and safety issues are paramount, and that patients and the
community generally can be assured that the quality of care received in public
hospitals meets the highest standards.