Stillbirth in Australia—an
overview
2.1
Australia is one of the safest places in the world to give birth, yet six
babies are stillborn here every day, making it the most common form of child
mortality in Australia.
2.2
Stillbirth affects over 2000 Australian families each year. For every
137 women who reach 20 weeks' pregnancy, one will experience a stillbirth. For
women from Aboriginal and Torres Strait Islander backgrounds the rate is double
that of other Australian women.[1]
2.3
Furthermore, the rate of stillbirth in Australia has not changed over
the past two decades, despite modern advances in medical practice and health
care. According to the Centre of Research Excellence in Stillbirth (Stillbirth
CRE), '[u]p to half of stillbirths at term in Australia are unexplained'.[2]
2.4
Stillbirth is one of the most devastating and profound events that any
parent is ever likely to experience. It is 30 times more common than Sudden
Infant Death Syndrome (SIDS), but stillbirth receives far less public or
government attention than other infant and childhood deaths.[3]
2.5
Stillbirth is a hidden tragedy. The culture of silence around stillbirth
means that parents and families who experience it are less likely to be prepared
to deal with the personal, social and financial consequences. This failure to
regard stillbirth as a public health issue also has significant consequences
for the level of funding available for research and education, and for public
awareness of the social and economic costs to the community as a whole.
The sorrow and sadness associated with a stillbirth has a
profound rippling effect across communities that is long-lasting and is
acknowledged to have significant social, emotional and economic impacts.[4]
2.6
This chapter outlines the numbers, rates, causes, and risk factors of
stillbirth in Australia compared with other high-income countries.
Stillbirth rates
International trends
2.7
Internationally, the number of stillbirths occurring at or after 28
weeks' gestation declined by 19.4 per cent between 2000 and 2015, representing
an annual reduction of two per cent. The World Health Organisation (WHO) estimated
that, in 2015, there were 2.6 million stillbirths at or after 28 weeks'
gestation worldwide. Most (98 per cent) stillbirths occur in low- and
middle-income countries, and over half (60 per cent) occur in rural areas.[5]
2.8
The table below shows the rates and ranking of selected countries,
including Australia, in 2009 and 2015, based on the WHO definition of
stillbirth.
Table 2.1: Stillbirth rate (at or
after 28 weeks' gestation) per 1000 births, and rank, by country, 2009 and 2015[6]
| Country |
2009 |
2015 |
| Rate |
Rank |
Rate |
Rank |
| Finland |
2.0 |
1 |
1.8 |
4 |
| New Zealand |
3.5 |
34 |
2.3 |
11 |
| Australia |
2.9 |
15 |
2.7 |
17 |
| UK & Northern Ireland |
3.5 |
33 |
2.9 |
26 |
| USA |
3.0 |
17 |
3.0 |
29 |
| Canada |
3.3 |
26 |
3.1 |
30 |
| Malaysia |
5.9 |
55 |
5.8 |
55 |
| China |
9.8 |
82 |
7.2 |
68 |
| India |
22.1 |
154 |
23.0 |
165 |
| Pakistan |
46.7 |
193 |
43.1 |
194 |
High-income countries
2.9
Significant movement up the rankings occurred between 2009 and 2015 for
the United Kingdom (UK) and Northern Ireland, and New Zealand; Australia
slipped by two places; and the United States of America (USA), while having the
same rate of stillbirth in both years, fell in ranking from 17 to 29.
2.10
Analyses of data in high-income countries show a decrease in the rate of
stillbirth over the past 50 years, attributed largely to improvements in
intrapartum care, but there has been little or no improvement over the past two
decades and evidence of increases in some countries including Australia.[7]
2.11
In 2017 countries with the lowest stillbirth rates were Iceland (1.3
stillbirths per 1000), Denmark (1.7), and Finland (1.8).[8]
2.12
Australia (2.7 stillbirths per 1000) lags well behind other high-income
countries, with the stillbirth rate beyond 28 weeks of pregnancy 35 per cent
higher than the best-performing countries.[9]
Australian trends
2.13
The rate of stillbirth in Australia is based on the Australian Institute
of Health and Welfare (AIHW) definition of stillbirth as a fetal death
occurring at 20 or more completed weeks of gestation or 400 grams or more
birthweight.[10]
2.14
The AIHW uses this definition for the National Perinatal Data Collection
(NPDC). This differs from the definition recommended by the World Health
Organisation (a baby born with no signs of life at or after 28 weeks of
gestation or 1000 gram birthweight) and the United Kingdom (24 weeks).[11]
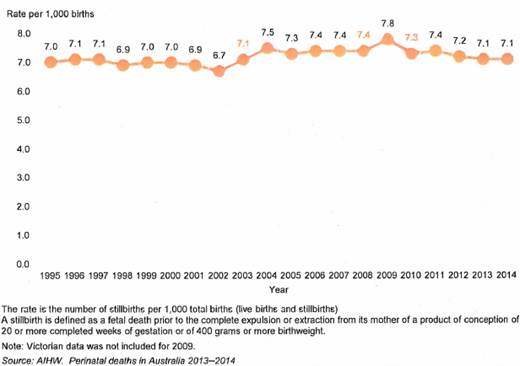
2.15
Between 1995 and 2014, there was an overall reduction in neonatal deaths
(deaths occurring from birth to 28 days old), from 3.2 to 2.6 per 1000 births.
However, the rate of stillbirth remained relatively unchanged, varying between
6.7 and 7.8 deaths per 1000 births over the same period (see Figure 2.1 below).
Figure 2.1: Stillbirth rate in
Australia, 1995−2014[12]
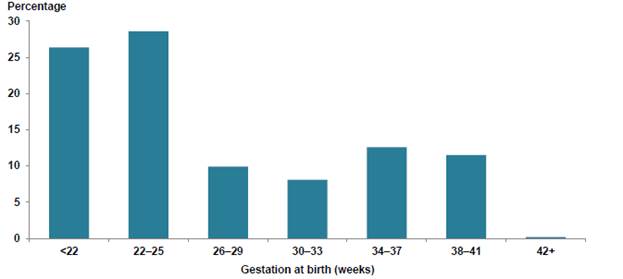
2.16
Figure 2.2 shows the percentage of stillbirths by gestation at birth in
Australia over 2013 and 2014.
Figure 2.2: Percentage of
stillbirths by gestation at birth in Australia, 2013−14[13]
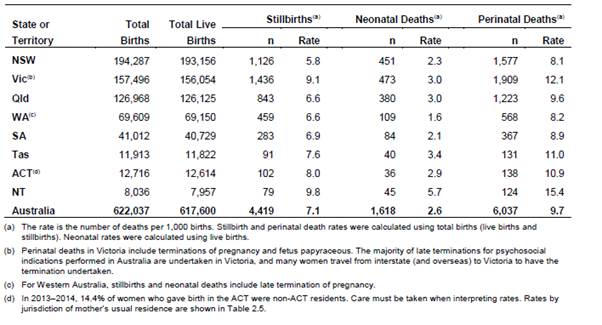
2.17
Table 2.2 presents the numbers of births, live births and stillbirths
and the rate of stillbirths by jurisdiction between 2013 and 2014.
Table 2.2: Perinatal deaths by
jurisdiction in Australia, 2013−14[14]
Causes of stillbirth
2.18
A high proportion of stillbirths in Australia are unexplained. Many occur
unexpectedly in late pregnancy, and many are related to undetected fetal growth
restriction (FGR) and placental conditions.
Many of the predisposing factors for stillbirth are closely
linked and overlap with those responsible for other serious perinatal outcomes
including hypoxic [lack of oxygen to the brain] and traumatic injury to unborn
babies.[15]
2.19
An AIHW study of the causes of stillbirths occurring between 1991 and
2009 showed the major causes of stillbirth in Australia as follows:
Table 2.3: Major causes of
stillbirth in Australia, 1991−2009[16]
| Cause of stillbirth |
% |
Number |
| Congenital abnormality |
22.3 |
1891 |
| Unexplained antepartum death |
22.3 |
1896 |
| Maternal Conditions |
13.4 |
1141 |
| Spontaneous pre-term (<
37 weeks gestation) |
11.5 |
980 |
| Specific perinatal condition |
8.1 |
684 |
| Fetal growth restriction (FGR) |
7 |
593 |
| Antepartum haemorrhage |
6.9 |
589 |
| Perinatal infection |
3.5 |
251 |
| Hypertension |
3.1 |
265 |
| Hypoxic peripartum death |
1.9 |
159 |
| No obstetric antecedent |
0.5 |
41 |
| Total |
100 |
8490 |
2.20
AIHW data for 2013−14
showed the main causes of stillbirth as congenital anomaly (27 per cent),
unexplained antepartum death (20 per cent) and maternal conditions (11 per
cent).[17]
Risk factors
High-income countries
2.21
According to recent international research, 90 per cent of stillbirths
in high income countries occur in the antepartum period, and are frequently
associated with placental dysfunction and FGR. Many stillbirths remain
unexplained, while others are associated with preventable lifestyle factors.[18]
2.22
One international study of stillbirth summed up the situation in
high-income countries:
The proportion of unexplained stillbirths is high and can be
addressed through improvements in data collection, investigation, and
classification, and with a better understanding of causal pathways. Substandard
care contributes to 20–30% of all stillbirths and the contribution is even
higher for late gestation intrapartum stillbirths. National perinatal mortality
audit programmes need to be implemented in all high-income countries. The need
to reduce stigma and fatalism related to stillbirth and to improve bereavement
care are also clear, persisting priorities for action. In high-income
countries, a woman living under adverse socioeconomic circumstances has twice
the risk of having a stillborn child when compared to her more advantaged
counterparts. Programmes at community and country level need to improve health
in disadvantaged families to address these inequities.[19]
2.23
Potentially modifiable risk factors for stillbirth in high income
countries include maternal overweight and obesity, advanced maternal age,
placental abruption and pre-existing hypertension and diabetes.[20]
Australia
2.24
Similarly, the major risk factors for stillbirth in Australia have been
identified by the Royal Australian and New Zealand College of Obstetricians and
Gynaecologists (RANZCOG) as obesity, advanced maternal age, smoking, first
pregnancy and diabetes and hypertension.[21]
2.25
As in other high-income countries, there is also an elevated risk of
stillbirth and other adverse pregnancy outcomes for women and women who live
with social disadvantage.[22]
2.26
In 2011−12,
the stillbirth rate for babies of teenage mothers and mothers older than 45 was
more than twice that for mothers aged 30−34
(13.9 and 17.1 versus 6.4 deaths per 1000 births).[23]
2.27
In 2015, most stillborn babies were preterm (85 per cent) and the mean
birthweight of stillborn babies (1125 grams) was far lower than for live-born
babies (3342 grams). Four in five stillborn babies were low birthweight, and
more than half (65 per cent) were extremely low birthweight (<1000 grams).[24]
2.28
A study of stillbirths in New South Wales found additional risk factors,
including small birthweight for gestation, low socioeconomic status, previous
stillbirth or preterm birth, Aboriginality, and maternal country of birth.[25]
2.29
However, studies have found that risk factors differ across gestational
age and reflect different causes, with foetal anomalies and infection
associated with stillbirth at early gestation; anomalies and antepartum
haemorrhage across 26−33
weeks; vasa praevia,[26]
infection and diabetes affecting late term stillbirths; and FGR being a strong
predictor across all gestations.[27]
2.30
Professor Craig Pennell, Senior Researcher at the Hunter Medical
Research Institute, remarked that about half of the causes of stillbirth have a
primary placental origin, but identifying those women whose placentas are not
functioning well becomes increasingly difficult as a pregnancy progresses:
...we're relatively good at picking up the low-hanging fruit
when it comes to pregnancies, but we're not very good at determining when a
pregnancy that is going well starts to fall off. The simplest way to explain
that is that the average placenta has about a 30 per cent reserve. So if I'm
looking at a patient and her baby's growing normally and her blood flow studies
are normal, all that tells me is that her placenta is functioning between 67
per cent and 100 per cent. It doesn't tell me where it is in that range.[28]
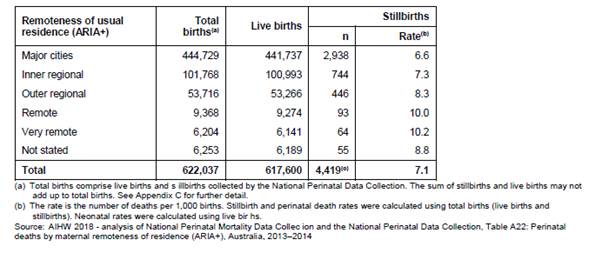
Regional and remote communities
2.31
Around 33 per cent of all stillbirths in Australia are to women who live
in regional and remote areas of Australia. According to AIHW data, the further
away women are from a major city, the higher the rate of stillbirth, as shown
in Table 2.4 below.
Table 2.4: Stillbirth deaths by
maternal remoteness of residence, Australia, 2013−14[29]
2.32
The AIHW found that babies born to mothers living in remote and very
remote areas were 65 per cent more likely to die during the perinatal period
than babies born to mothers living in major cities or inner regional areas, as
shown in Figure 2.3.
Figure 2.3: Perinatal mortality
rates by remoteness of maternal residence in Australia, 2013−14[30]
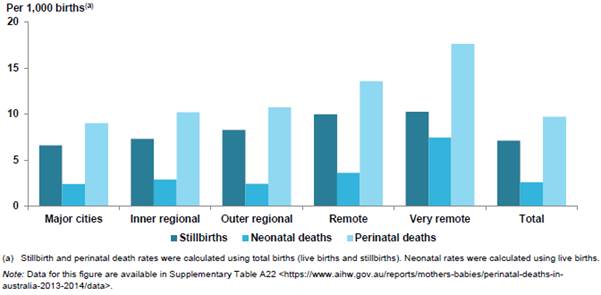
2.33
This trend may increase in the future as a result of the closure of
small maternity units in rural and remote communities across Australia, where pregnant
women are less likely to leave their community to seek antenatal care until
late in their pregnancy.[31]
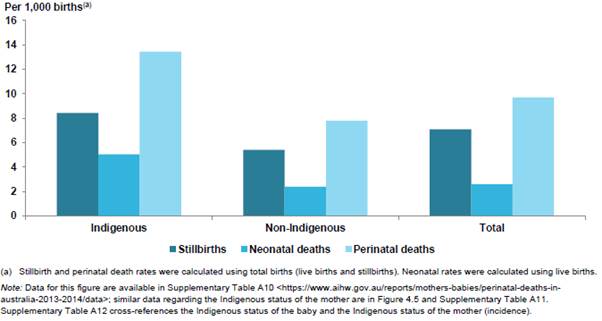
Aboriginal and Torres Strait
Islander communities
2.34
The rate of stillbirth for Aboriginal and Torres Strait Islander babies
is double that of other Australian women (13 in 1000 births compared to six in
1000 births).[32]
2.35
Whilst there has been some progress in reducing the disparity for
Indigenous women, this varies across jurisdictions. In Queensland, for example,
rates are reducing, in Western Australia there has been no improvement, and in
Victoria the rate amongst Aboriginal and Torres Strait Islander women has
fallen to that of non-Indigenous women.[33]
2.36
A recent study of stillbirth rates in Queensland found that Aboriginal
and Torres Strait Islander women continued to be at increased risk of
stillbirth as a result of potentially preventable factors including maternal
conditions, perinatal infection, FGR and unexplained antepartum fetal death.[34]
2.37
Figure 2.4 shows the Aboriginal and Torres Strait Islander stillbirth
rate by Indigenous status of the baby in Australia for the period 2013−14.
Figure 2.4: Perinatal mortality
rates by Indigenous status of the baby in Australia, 2013−14[35]
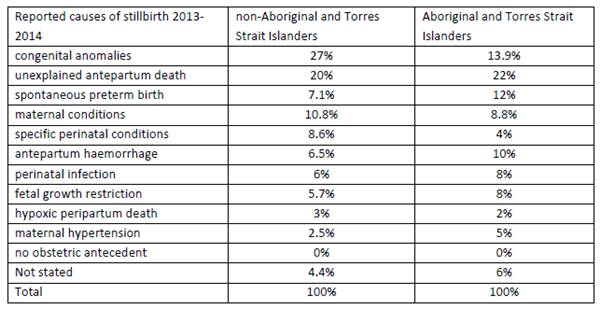
2.38
Table 2.5 compares the reported causes of stillbirth in 2013−14 between non-Aboriginal
and Torres Strait Islander women and Aboriginal and Torres Strait Islander
women.
Table 2.5: Perinatal Society of
Australia and New Zealand Perinatal Death Classification (PSANZ-PDC) cause of
stillbirth comparing non-Aboriginal and Torres Strait Islander women and
Aboriginal and Torres Strait Islander women, 2013−14[36]
2.39
Obesity is a major maternal risk factor for stillbirth in high income
countries. The rate of obesity increases with remoteness, with rural and remote
people 30 per cent more likely to be obese than those in major cities.
2.40
Maternal smoking is another risk factor for stillbirth in high income
countries. In Australia, 45 per cent of Aboriginal and Torres Strait islander
mothers smoke during pregnancy and are more likely to have pre-existing
diabetes or hypertension.[37]
2.41
There has been a significantly increased risk of stillbirth due to an
outbreak of syphilis infection among Aboriginal and Torres Strait Islander
women living in regional and rural areas.[38]
The Australian government responded in 2018 by introducing rapid point-of-care
testing across three high-risk regions in northern Australia, including a
strong focus on expectant mothers and women considering pregnancy.[39]
2.42
Such outbreaks have highlighted the need for infection prevention and
control through improved antenatal screening, treatment and notification of
partners as part of a broader stillbirth prevention strategy.[40]
Culturally and linguistically
diverse communities
2.43
There are higher stillbirth rates amongst culturally and linguistically
diverse (CALD) communities in Australia. In 2013−14,
1531 (34.6 per cent) of the 4419 stillbirths that occurred in Australia were
born to women who were themselves born in countries other than Australia.[41]
2.44
The percentage of women from CALD backgrounds in Victoria is slightly
higher, with 38.5 per cent of women giving birth in 2016 born outside of
Australia. However, information on ethnicity is not routinely collected for
perinatal data collections, and has resulted in incomplete data.[42]
Navigation: Previous Page | Contents | Next Page