Chapter 3
Commonwealth hospital funding
The 2014 budget did
serious damage to Commonwealth-state relations and the confidence with which
states could plan and manage health services. It did this by abrogating an
agreement about public hospital funding which had been signed by governments of
all political persuasions and unilaterally imposing a new funding model on the
states.[1]
Dr Stephen Duckett,
Director, Health Program, Grattan Institute
Introduction
3.1
The previous chapter provided the historical context of hospital funding
in Australia, and the struggle to find an agreement between levels of
government about funding responsibility. As noted in Chapter 2, a forum for
cooperation between federal, state and territory governments was achieved in
2011 when all parties signed the National Health Reform Agreement (NHRA). As a
result of this agreement, long term funding certainty, through until at least
2024-25 was achieved for hospital funding.
3.2
This chapter examines the impact of the Coalition Government's decision
to cease the funding mapped out under the NHRA. The effects of this decision,
made in the highly criticised 2014-15 Budget, have reached further than just
the removal of funding. This chapter also looks at:
-
the need for a mechanism that promotes cooperation between state
and federal governments on hospital funding and planning;
-
missed opportunities to promote reform in hospital funding;
-
the need for long-term, sustainable funding which allows for
workforce planning and infrastructure development; and
-
issues that have emerged or been exacerbated by the removal of certainty
in hospital funding.
2014 changes to Commonwealth hospital funding
Unsustainable health spending myth
3.3
A key element in the Coalition Government's justification of the cuts to
hospital funding was the argument that government expenditure on health was
unsustainable.[2]
The same argument was used to justify the $7 co-payment policy, later scrapped,
and the continuing freeze on MBS indexation.[3]
3.4
This argument has been widely disputed. In its Public Hospital Report
Card 2015, the Australian Medical Association (AMA) observed in relation to
the Coalition Government's health and hospital funding cuts:
The Government has justified its extreme health savings
measures on the claim that Australia’s health spending is unsustainable. But
Australia’s health financing arrangements are not in crisis.
In 2012-13, Australia had the lowest growth (1.5 per cent) in
total health expenditure since the Government began reporting it in the
mid-1980s. Without any specific Government measures, there was negative growth
(minus 2.2 per cent) in Commonwealth funding of public hospitals in 2012‑13,
and only 1.9 per cent growth in 2011-12. Our health sector is doing more than
its share to ensure health expenditure is sustainable.
Australia's expenditure on health has been stable as a share
of GDP, growing only one per cent over the last 10 years. Health expenditure
does not demand radical changes to existing services.[4]
3.5
Compared to other OECD countries, Australia spends just below the OECD
average for health funding. In 2015, Australia spent 9.7 per cent of GDP[5]
on health, while in comparison the US spent 16.4 per cent of GDP,[6]
Canada spent 10.2 per cent,[7]
and the UK spent 8.5 per cent.[8]
The OECD Health at a Glance 2015 notes that Australia's health
expenditure 'achieves good outcomes relatively efficiently'.[9]
2014-15 Budget cuts to hospital
funding
3.6
The 2014-15 Budget Overview incorrectly categorised hospital
funding as primarily a state responsibility:
State Governments have primary responsibility for running and
funding public hospitals and schools. The extent of existing Commonwealth
funding to public hospitals and schools blurs these accountabilities and is
unaffordable.[10]
3.7
On this argument, the government used the 2014-15 Budget to unilaterally
cancel the NHRA, signed by the states and Commonwealth governments in 2011, and
terminate various health-related National Partnership Agreements.[11]
States were 'expected to continue contributing to these arrangements at their
expense.'[12]
3.8
As part of the 2014-15 Budget, the Federal Government pledged that from
2017-18 Federal Government funding would revert to the former block funding
model based on indexation at the Consumer Price Index (CPI) and population
growth.[13]
Despite promising "no cuts to health", the Federal Government
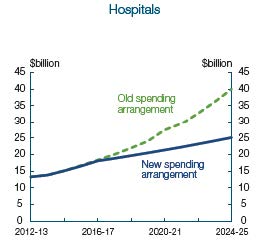
projected that this new funding arrangement would save over $57 billion
between 2017-18 and 2024-5.[14]
Figure 1, reproduced from the 2014-15 Budget Overview, shows the
government's projected reductions to hospital funding.
Figure 1—projected hospital funding cuts from the 2014‑15
Budget[15]
3.9
The Coalition Government's 2014-15 Budget was widely criticised. For
example Dr Stephen Duckett, Director of the Grattan Institute's Health Program,
told the committee:
The 2014 budget provided that future indexation to the states
would be in line with:
... a combination of the Consumer Price Index and population
growth.
If this is taken at face value, then the 2014 proposal is the
most parsimonious indexation arrangement that has ever applied to public
hospital funding grants.[16]
3.10
The Budget Overview went on to explain that the responsibilities of the
different levels of government would be the subject of a White Paper on the
Reform of Federation, to be completed at the end of 2015.[17]
The recently abandoned White Paper process is discussed further below.
Impact of hospital funding cuts on
states and territories
3.11
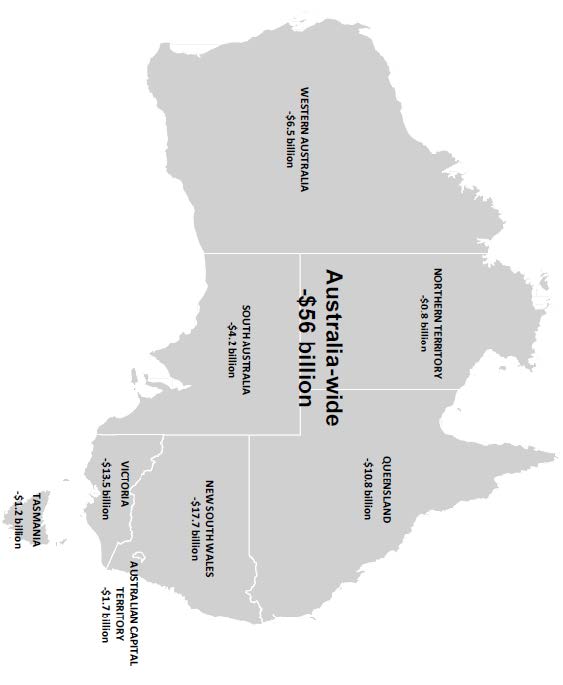
The committee sought a submission from the Parliamentary Budget Office (PBO)
in order to gain a clearer understanding of the impact the Coalition
Government's funding cuts will have on each state and territory. The submission
is reproduced at Appendix 4. Figure 2, which is based on the PBO's findings,
shows the funding each state and territory will lose as a result of the 2014-15
Budget.
3.12
The funding cuts calculated in the PBO's submission relate to the
2014-15 Budget decision. These preceded the April 2016 COAG agreement to partly
reinstate funding out to 2020. While this COAG decision, discussed below, has
partially mitigated the 2014-15 Budget cuts, the $2.9 billion allocated across
three years (2017‑18 to 2019-20) is not adequate to address the $7.9 billion
shortfall over this same period created by the 2014‑15 Budget cuts.
3.13
During its inquiry, the committee has undertaken 52 hearings and held
public hearings and site visits in every state and territory. The following eight
chapters focus on each of the states and territories, detailing the extent of
the loss of funding and the issues which have arisen for each state. While
state governments have, to a large extent, provided short-term additional
funding to cover the immediate Commonwealth shortfall, this situation is
unsustainable long term. The loss of certainty over long term funding has also
meant that state governments are unable to forward plan workforce and
infrastructure and must subsist from budget to budget.
3.14
In addition to state-specific issues, there are also some issues caused
by the cuts to hospital funding that are Australia‑wide. These range from
high-level policy questions, such as the need for a mechanism for cooperation
between the states and federal governments, to grassroots impacts, such as
increased waiting times. These national implications are discussed throughout
this chapter.
Figure 2—Commonwealth hospital funding cuts from the
2014-15 Budget[18]
'Skin in the game'
Removal of the mechanism for state
and federal cooperation
3.15
As described in Chapter 2, the history of hospital funding in Australia
has been marked by a struggle to find a means of settling the respective
contributions of the state and federal governments. Of particular importance
has been the need to avoid short-term funding agreements and instead establish
sustainable long-term funding arrangements.
3.16
The Coalition Government's unilateral abandonment of the long-term NHRA
did more than remove Commonwealth hospital funding. It caused the loss of
goodwill in state-federal cooperation on health. Dr Stephen Duckett, Director
of the Grattan Institute's Health Program, described the 2014-15 Budget as
having done 'serious damage to Commonwealth-state relations and the confidence
with which states could plan and manage health services.' It did this by:
...abrogating an agreement about public hospital funding which
had been signed by governments of all political persuasions and unilaterally
imposing a new funding model on the states. The funding model promulgated in
the 2014 budget was presented in the budget papers as saving more than a
billion dollars over the forward estimates, with savings described as being in
the tens of billions over the ensuing decade. The words 'saved' and 'savings'
are an example of creative accounting. They are savings to the Commonwealth
budget only, but are not real savings to the public purse at all. Instead, they
are simply a massive and unsustainable transfer of costs from the Commonwealth
budget to state budgets.[19]
3.17
Dr Duckett categorised the NHRA as having 'dealt with some of the
dysfunctional aspects of federalism in health care'. The agreement had done
this by:
...creating an alignment of incentives. It made the
Commonwealth share directly in the costs of activity growth in health care,
which gave it an incentive to develop policies in its sphere that might
mitigate that growth. For example, the Commonwealth traditionally funds primary
care, while the states fund hospital care. Making the Commonwealth share
responsible for hospital funding gave it a stronger incentive to improve
primary care and reduce the number of avoidable and expensive hospital visits,
generating actual savings to the public purse. The 2014 budget removed that
alignment of incentives.[20]
3.18
Professor Mike Daube, Director of Public Health Advocacy Institute of
Western Australia at Curtin University, agreed with Dr Duckett. Professor Daube
described the situation after the 2014 cancellation of the NHRA funding
agreement as:
There is a whole lot in limbo now. I must say I think it
created distrust of central government, because if you have agreements that are
supposed to be lasting and suddenly they are cut then the state governments
which had to implement them will have people on contracts and so on, because
they would have assumed that the funding would continue. So it creates distrust
for them. It creates uncertainty out in the community...[21]
3.19
In the two years since the 2014-15 Budget, there has been much debate
about the role of the Federal Government in hospital funding. The Reform of the
Federation White Paper process has been part of that debate, although not to
the same extent as the ongoing criticisms of the 2014-15 Budget by groups like
the AMA.
Reform of the Federation White
Paper
3.20
The White Paper process was begun in the first half of 2014. Its main
objective was to 'clarify roles and responsibilities to ensure that, as far as
possible, the states and territories are sovereign in their own sphere.'[22]
Other objectives included reducing duplication between levels of government and
improving the efficiency of the federation.[23]
3.21
As part of the White Paper process, issues papers regarding various
aspects of the federation, including health and hospital funding, were produced
in the second half of 2014. However the Green Paper, which was to be released
in the first half of 2015, was not published until after it had been leaked in
June 2015.[24]
3.22
The 'discussion paper', as the leaked Green Paper was titled, lists five
options for reform of hospital funding. These range from a shared
responsibility for funding between the state and Federal governments to sole
funding responsibility resting on state and territory governments:
-
establishment of a benefit scheme similar to the Medicare
Benefits Schedule for all hospital treatments;
-
Commonwealth and states jointly fund individualised care packages
for chronic or complex conditions;
-
establishment of regional purchasing agencies to source health
services geographic areas;
-
Commonwealth becomes solely responsible for funding; or
-
states take full responsibility for public hospitals.[25]
3.23
It had been anticipated that federation reform would be part of the COAG
leaders' retreat on 23 July 2015, but the topic was not covered in the
communique for that meeting. Reform was discussed at the 11 December 2015 COAG
meeting, but leaders only agreed to further consideration of health funding at
the first COAG meeting of 2016.[26]
3.24
The White Paper on federation reform had been scheduled for publication
at the end of 2015, but this did not happen. Instead, a variation of the
options in the 'discussion paper' was put to the COAG meeting held on 1 April
2016, leading to an agreement to extend activity based funding to 2020
(discussed further below).
3.25
On 28 April 2016, the Prime Minister confirmed that the Reform of
Federation White Paper process had been scrapped, with no White Paper to be
released.[27]
The cost of the process was reported to be in excess of $5 million.
3.26
The Reform of the Federation White Paper website explains that:
...work to improve federal financial relations and the
transparency of government spending will be progressed by the Council on
Federal Financial Relations, and the Commonwealth, state and territory
Treasuries. A progress report will be brought to the next COAG meeting.[28]
Committee view
3.27
The Reform of Federation White Paper could have been a valuable process
for rebuilding state-federal relations after the disastrous 2014-15 Budget.
Instead, it has been significant waste of public money, and has only resulted
in returning state-federal relations back to the often combative forum of COAG.
April 2016 COAG agreement
3.28
On 1 April 2016 the Prime Minister, the Hon Malcolm Turnbull MP, faced a
hostile COAG meeting with states and territories concerned that the 2014-15 Budget
cuts to hospital funding would leave them unable to provide adequate hospital
services.[29]
The Prime Minister's proposal to the states was for an additional $3 billion
over three years for hospital funding, and the possibility that the states could
raise their own income taxes as funding for the longer term.[30]
3.29
While the income tax proposal was rejected by the states, COAG did agree
to a Heads of Agreement for hospital funding to run from 1 July 2017 to 30 June
2020 'ahead of longer-term arrangements'.[31]
Additional Commonwealth funding under the agreement was to be $2.9 billion
between 2017-18 to 2019-20, with growth capped at 6.5 per cent per year.[32]
The funding was to be provided primarily on the basis of activity based funding
and block funding under certain circumstances as set out under the NHRA.[33]
3.30
For their part in the agreement, states undertook to:
-
reduce demand for hospital services through better coordinated
care, particularly for people with complex and chronic diseases;
-
improve hospital pricing mechanisms; and
-
reduce the number of avoidable hospital readmissions.[34]
3.31
Although the April 2016 agreement provides partial and short-term
respite from the full force of the 2014-15 Budget funding cuts, the additional
funds in the agreement fall well short of the funding states would have
accessed under the NHRA. Instead of the NHRA's funding increase of 9 per cent
per annum, the states will see funding growth capped at 6.5 per cent, only 2
per cent improvement on the 4.5 per cent rate unilaterally imposed by the
2014-15 Budget.[35]
3.32
As discussed earlier, the additional $2.9 billion figure compares poorly
with the funding increase of $7.9 billion which would have flowed to the states
had the government not abandoned the NHRA.[36]
Need for long-term, sustainable funding
3.33
The April 2016 COAG agreement is welcome in that it is an improvement on
the hospital funding cuts contained in the 2014-15 Budget. However, it does not
go towards solving the larger problem: that a long-term funding agreement is
urgently needed to replace the NHRA which was abandoned in the 2014-15 Budget.
3.34
Since May 2014, state and territory governments have been forced to
operate in an atmosphere of uncertainty. States have faced the fact that Commonwealth
funding will decrease from the expected NHRA levels, and have been planning how
to mitigate the worst impacts of the loss. In South Australia, representatives
of the Department of Health and Ageing told the committee that their ability to
plan for future hospital services is compromised by the uncertainty around
funding:
It is clear that where the Commonwealth provides funding it
is welcome by the state. However, South Australia and SA Health is keen to
ensure that any benefits of reform measures...are durable in the long term. SA
Health's ability to undertake budgetary and service planning is compromised by
uncertainty created by the Commonwealth. Uncertainty remains about public
hospital funding. National Health Reform Agreement arrangements are unlikely to
be clarified until the release of the Commonwealth's white paper on the reform
of the federation in 2016.
SA Health looks forward to the ideas to be presented by the
Commonwealth about future roles and responsibilities for the health system as
part of this process. The present situation leaves the state bearing the risks
associated with growing demands on hospital costs and without the resources to
meet the expected growth. The state has had limited ability to influence the
full range of policy levers across the health system as a whole that drive
demand and public hospital services. This is not a sustainable process for the
health system in the future.[37]
3.35
In Victoria, representatives from the Department of Health and Human
Services told the committee that the Commonwealth is a 'critical partner' for
states in providing high quality hospital services:
The adoption of activity based funding as the basis for
Commonwealth funding contributions in 2011 signalled a commitment to carry a
share of hospital demand growth. To give that some perspective, Commonwealth
funding for public hospitals grew by an average of 6.6 per cent per annum for
the decade to 2010-11, growing to 7.1 per cent per annum to 2013-14. And growth
was estimated at 9.4 per cent beyond the 2013-14 forward estimates, based on
projected growth for Victorian public hospitals published in the 2013-14 MYEFO.[38]
3.36
The experience was similar in Queensland. Ms Kathleen Forrester, Deputy
Director-General Department of Health, told the committee that the NHRA had
provided a 'new and very different Commonwealth funding methodology' which:
...created the financial incentives for all levels of
government to work together to ensure the health system functions efficiently
and holistically to improve overall health outcomes. Furthermore, the
methodology accounted for all the main drivers of public hospital service cost
growth, because it is based on the actual increase in the volume of public
hospital services provided to patients.[39]
3.37
In comparison, the 2014-15 Budget decision to base funding on indexation
of CPI and population growth would 'break the link established...between
Commonwealth funding and efficient [growth] in public hospital services,
reducing the financial incentives for all aspects of the health system to work
together to improve outcomes.'[40]
The result would be:
...the major costs associated with other drivers of healthcare
demand would be borne by the states and territories, leading to an
ever-increasing share of state funding and a declining Commonwealth share. The
proposed funding model assumes that all population groups have the same need
for public hospital services. For example, it does not take account of the
greater health needs of Indigenous people and people from rural and remote
locations. This is particularly important for Queensland, which has the most
decentralised population in Australia. Nor does it take account of the ageing
population or the changing cost of service provision due to technological
advances.[41]
State issues
3.38
Chapters 4 to 10 of this report provide details of the impact of the
Federal Government's hospital funding cuts on each state and territory. While
the cuts had not been due to begin until 2017-18, the announcement of the
decision in the 2014-15 Budget included the removal of many of the National
Partnership Agreements which had provided funds to states and territories as
part of the NHRA. The effect of the funding cuts was therefore immediate, and states
had to begin planning for how to make up the shortfall in funds.
3.39
National Partnership Agreements, such as that relating to improving
hospital services, provided significant benefit, particularly to smaller states
and territories. In these cases, the funding cuts were felt most acutely. The
Northern Territory Chief Minister, the Hon Adam Giles MLA, described the loss
of the National Partnership Agreement funding:
Contrary to comments made by the Prime Minister today, the
pain from these front line service cuts will start being felt by the States and
Territories from July 1, 2014.
Let’s look at two examples. In 43 days time, the Territory
stands to lose $1.4 million in Federal funding for pensioner concessions and
health funding will be cut by $33.8 million or the equivalent of a minimum of
ten hospital beds.
These funding decisions will have a real and immediate impact
on the front line services offered to Territorians.[42]
3.40
Many states pledged to cover the immediate funding gap themselves;
however, that situation is not sustainable beyond the very short term. Issues
have already begun to emerge which demonstrate that without a state-federal
funding partnership, the states cannot adequately support Australia's
hospitals.
Committee view
3.41
Since its establishment in June 2014, the Senate Select Committee on
Health has seen other disastrous health policies from the 2014-15 Budget
scrapped or put on hold. But while the government has reversed ill-conceived
policies like the $7 co‑payment, the cuts to hospital funding have
lasted until 2016, when backlash from the states forced the government to make
a temporary and partial extension of funding.
3.42
Before the NHRA was agreed in 2011, respective hospital funding contributions
had been a struggle between the state and federal governments. The reforms to
hospital funding implemented by the previous government allocated virtually
equal responsibility for funding to the state and federal governments, and
created a mechanism for all parties to work together to ensure that funds were
used efficiently.
3.43
When the Federal Government unilaterally tore up the NHRA in the 2014‑15
Budget, the action set hospital funding arrangements back ten years. The
decision obliterated states' confidence in any federal-state funding
negotiation process. State hospital infrastructure and workforce planning, which
was appropriately based on the long-term funding agreement in the NHRA, was
thrown into uncertainty. State governments struggled to figure out how to make
up the shortfall in funding; many admitting that it would not be possible
unless funding was taken from other areas.
3.44
The defining achievements of the NHRA were to:
-
provide long-term funding and continuity of funding to enable workforce
and infrastructure planning;
-
create a forum for states and federal governments to work
together on hospital funding; and
-
establish an activity based funding model and the associated
national efficient price for hospital services.
3.45
The Government's 2014-15 Budget decision to allocate federal hospital
funding based on indexation of CPI and population growth, and unilaterally scrap
the NHRA, has:
-
destroyed state and territory government confidence in
negotiation with the federal government;
-
removed the best forum for state-federal partnership and
cooperation over hospital funding; and
-
created a shortfall in hospital funding that the state
governments are struggling to cover.
3.46
The Federal Government claimed in 2014 that the Budget measures were put
in place because health funding was unsustainable. In actual fact, the 2014-15
Budget has created the situation where hospital funding, with the burden shifted
significantly to the states, is unsustainable.
3.47
Although the COAG agreement of April 2016 has partially mitigated the damage
done by the 2014-15 Budget, the future of hospital funding is bleak. At best
the three year agreement has created space for the federal government to work
to rebuild the confidence of the states and establish a long-term agreement on
hospital funding, backed by fair, equitable and sustainable federal funding.
3.48
As the following chapters of this report show, the NHRA had been working
effectively to distribute funding in a responsible and equitable way to public
hospitals. The Coalition Government unilaterally scrapped the NHRA and replaced
it with what can only be described as an omnishambles or 'a situation that has
been comprehensively mismanaged, characterised by a string of blunders and
miscalculations'.[43]
3.49
The committee believes that there is only one way Commonwealth-state hospital
funding arrangements can be repaired, and that is to work through the NHRA. The
committee's recommendations go towards this goal.
3.50
In building on the NHRA, rather than the omnishambles created by the
2014‑15 Budget and the Government's misguided actions since, the
committee believes that the Federal Government needs be a partner with the
states in terms of hospital funding. Without 'skin in the game', there is no
incentive to work with state governments to ensure that funding is used
efficiently. The Federal Government needs to urgently build goodwill with the
state and territory governments, in order to create a solid foundation for any
future finding agreement.
Recommendation 2
3.51
The committee recommends that the Government reconstitute the National
Health and Hospitals Reform Commission or a similar body to review hospital
funding arrangements and build on the National Health Reform Agreement. This
process should be guided by the principles of equity, fairness, adequate
funding and long-term certainty to ensure the continuity of public hospital
services.
3.35 While the committee is pleased that the Federal
Government has made a temporary agreement with the states until 2020, which partially
restores the withdrawn NHRA funding, the committee believes that this is not sufficient.
Until recently, the Federal Government was actively working to remove the
mechanisms by which activity based funding was set up. The committee urges the
government to halt the closure of the Independent Hospital Pricing Authority,
and the other structures put in place by the former government to implement
activity based funding.
3.52
The committee supports activity based funding as the best means of
delivering limited funds in a manner that drives greater efficiencies and
provides a strong incentive for the Commonwealth to improve primary care and
reduce the number of avoidable and expensive hospital visits.
Recommendation 3
3.53
The committee recommends that the Government urgently give an
undertaking that the mechanisms for activity based funding, such as the
Independent Hospital Pricing Authority, and the other structures put in place
by the former government to implement activity based funding, will not be
dismantled.
Navigation: Previous Page | Contents | Next Page