Navigation: Previous Page | Contents | Next Page
Chapter 3
Procurement and supply of AT
Factors in NDIA decision making
3.1
Submitters highlighted a number of reasons why participants may be subject
to inappropriate decisions, or are experiencing misdirected funding or
shortfalls in their plans. These include:
- disregard of expert advice;
- the Scheme's focus on AT products rather than services;
- varying knowledge and experience in AT of planners;
- differing abilities of participants to understand, predict, and
advocate for AT; and
- the Scheme's emphasis on value for money.
Utilisation of expert reports
3.2
Reports from therapists are routinely required as part of the assessment
process. Unfortunately, the committee received a plethora of feedback that
there is general disregard for expert advice and recommendations on appropriate
AT for participants amongst planners and staff considering applications.[1]
3.3
Can:Do Group argued that specialist recommendations are frequently
ignored by delegates despite their lack of knowledge about the device or
client:
The lack of specialist knowledge of planners regarding AT
needs for participants is highly concerning, as they are allocating funding and
making decisions regarding appropriate devices, often without ATS assessments
or in direct contravention of expert advice. This is resulting in insufficient
funding to provide equipment required, or rejection of recommended equipment
required by the client. There is also a lack of appreciation for specialised AT
knowledge – which is evident across NDIA. Recommendations are often over ruled
or over looked.[2]
3.4
The Benevolent Society raised similar concerns:
Our staff find it very frustrating to have conducted
extensive trials on equipment, to only have their recommendation following the
trials declined or questioned by the NDIA who may suggest trialling less
expensive but inappropriate technology. [3]
3.5
The committee heard that therapists' reports are frequently
misunderstood, or not read by, staff reviewing applications.[4]
3.6
Submitters argued that the Agency should recognise practitioners' AT
knowledge, experience, and judgement to make appropriate recommendations,
especially in cases where it has requested the advice.[5]
3.7
Ms Volkert from Occupational Therapy Australia made the point that the
NDIA's administrative requirements often involve a relatively unskilled planner
making decisions, sometimes in conflict with that of the therapist:
All too often the delegate is an unskilled planner who does
not have an understanding of disability, the clinical reasoning required to
determine the most appropriate solution for an individual or the AT options
available to address disability. We are also particularly concerned to hear of
instances when a planner or an unskilled delegate has sought to change selected
items within an AT application without consulting the prescribing occupational
therapist, resulting in the provision of inappropriate or inoperable assistive
technology.[6]
3.8
Ms Olsson from Speech Pathology Australia concurred, and provided an
example of NDIA staff making recommendations about Augmentative and Alternative
Communication (AAC) Assistive Technology:
[There are] various issues related to poor planner knowledge
and skills and their propensity to work outside of their scope, such as making
recommendations for AAC AT themselves or suggesting alternative options to
those that have been recommended by an experienced allied health practitioner,
repeatedly requiring the assessor adviser to provide additional and lengthy
clinical justifications for their recommendations as part of trying to make
their decisions about whether the item meets the reasonable and necessary
requirements, and refusing a request based on uninformed or ill-informed
assumptions about what AAC AT is appropriate or represents value for money for
participants.[7]
3.9
As illustrated below in the discussion about mainstream technology, the
criteria used by the NDIA delegate sometimes results in perverse outcomes which
do not meet the participant's needs:
It's certainly been the experience that we have heard from
our members that decisions are questioned and overturned. It is occasionally
the situation that a recommendation from an occupational therapist is
overturned and something more expensive is put into place.[8]
3.10
The NDIA responded to questions from the committee that over the last
two years of the Scheme operating, inconsistencies in advice from specialists
has led to the Agency being circumspect about the advice provided:
[T]he experience of the agency in the last two years is that
the variation in that advice, which we didn't expect to see, has meant that in
some cases we get really good advice and in other cases the advice has proved
problematic. So we've had some participants with a request that we have signed
off on for, say, an $18,000 wheelchair, but the actual assessment hadn't
checked the person's home, so they actually couldn't get it in the front door.
There was a key flaw that had occurred.[9]
3.11
When further pressed by the committee, Dr Walker from the NDIA said the
Agency would 'assist' participants who are in the situation where the planner
has disagreed with the advice of a specialist, to 'put strength back into that
advice'.[10]
3.12
Furthermore, Dr Walker stated in response to a question on whether there
should be a presumption in favour of accepting specialist advice:
I think that would be our approach.[11]
Interaction between the NDIA and
Allied Health professionals
3.13
In a related area, the committee also heard that it is very difficult
for a therapist to communicate with the Agency to clarify any aspects of their
advice.[12]
3.14
Submitters argued the inequity could be mitigated by requiring staff
processing applications to contact the prescribing therapist if they have
queries about the request, or are planning on rejecting the application, to
allow for any misunderstandings to be resolved during the decision-making
process.[13]
3.15
The Agency explained that NDIS delegates are unable to contact assessors
if consent has not been provided by the participant.[14] However, the NDIA is working to incorporate explicit consent from participants
on its improved templates to ensure that delegates can contact prescribing
therapists for clarification as needed.[15]
3.16
The NDIA is also piloting a panel of specialised AT assessors in Q3 2018–19
to attempt to improve the quality of plans.[16] According to the Agency these changes are expected to help manage assessment
costs, through contracted arrangements with a specialised panel of providers to
inform the planning process.[17] Mr Scott McNaughton, General Manager, Government, NDIA, explained:
...the most significant reform that we've got coming up next
year is creating a specialist panel of AT assessors who'll work on arranging
the functional assessment for those more complex and costly AT home modifications
and vehicle modifications. The intent there is for the panel to do that
assessment before a plan is approved. Then we use that information and approve
the plan so the person doesn't have to wait for those assessments after the
plan's approved. We think that will really expedite the process quite
considerably and unblock some of those challenges we experience now. We're also
creating internally a team of subject matter experts who will provide counsel
and more support for our network so that we can reduce delays and help monitor
and resolve more quickly any issues that keep arising.[18]
3.17
However, Vision Australia expressed deep concerns that a panel
type arrangement would only provide a generic response, and would not provide
the specialist knowledge that some AT decisions require for specific
conditions:
...we are concerned that the panel of assessors for AT will be
a generic one, without specialist understanding or knowledge sufficient to
determine the AT support needs of a participant who is blind or has low vision.
Vision Impairment makes up between 2-4% of the NDIS market, and the AT support
options are highly specialised, from braille devices to new technology such as
Aira. Participants who are blind or have low vision, and other low incidence cohorts,
will have limited confidence in a new system which does not recognise
specialist need.[19]
Committee view
3.18
A fundamental aspect of how the Agency interacts with Allied Health
professionals in this space is trust. Over the course of numerous inquiries the
committee has heard repeated evidence of what can only be described as the
development of a culture of mistrust of participants and their needs. The
evidence the committee heard in this inquiry around how formal clinical reports
and expert opinions of Allied Health professionals are discounted, or second
guessed, in favour of either those of the planners, or presumably in favour of
other allied health professionals without specific knowledge of the case on an 'expert
panel'.
3.19
The committee recognises the Agency's efforts to introduce a panel of
specialised AT assessors to help improve quality of plans. However, if planners
and NDIA staff placed greater trust in the advice of professionals and
participants, it would not need to implement a panel of specialists.
3.20
The committee is well aware of the financial imperatives the Agency is
required to work to, and that there will be circumstances where a further
assessment will be appropriate. However these circumstances should be
prescribed and published.
3.21
Given the evidence received, in particular from professional
organisations representing highly trained and accredited Allied Health
professionals, the committee is of the view that there should be a presumption
in favour of accepting the advice from appropriate experts.
Recommendation 4
3.22
The committee recommends that the Agency publish criteria of the
circumstances which will require the Agency to conduct further assessment
beyond that provided by a registered therapist.
Focus on AT equipment rather than outcomes
3.23
The NDIS AT Strategy supports the provision of tablets and
smartphones where they are found to be the most cost effective solution that
best meets the participant's needs. It states that:
- AT in the NDIS includes devices used by people without disabilities
(e.g. smartphones, tablets and 'apps') that are offering new ways to form
connections and increase participation;[20]
- the Agency is committed to keeping up to date with changes to mainstream
technology and how they can benefit people with disability;[21] and
- smartphones and tablets are offering potential solutions in some parts
of the disability sector. These require further investigation and efforts to
encourage take-up, given tablets and smartphones may provide similar functionality
to a specialist disability device and are generally lower cost.[22]
3.24
In many cases, a smartphone or tablet is the most appropriate and
cost-effective AT solution for the participant.[23] However, the committee has repeatedly received feedback that smartphones and
tablets are being rejected by the Scheme on the grounds that they are 'mainstream
technology'.[24]
3.25
Ability Research Centre expressed bewilderment that the Agency would
reject superior devices simply because they were 'mainstream':
...it is clear that sometimes a generic option such as an iPad
is simply the best option, offering superior outcomes and value for money. Yet
these recommendations are consistently queried, or even rejected outright, by
NDIA staff. Despite the inclusion of “customised commercial tablet” in the NDIA
AT Code Guide, it is now notoriously difficult to get an iPad approved by the
NDIA. It is baffling that the NDIA would always fund a dedicated communication
device over an iPad, despite the latter being more compatible, better supported
and up to ten times less expensive.[25]
3.26
The absurdity of the policy was captured in this example:
...we had a client who had an AT system of environmental
control equipment recommended for him. One element of the system was a
smartphone or tablet, neither of which were owned by the client. As funding for
this element of the system was denied by the NDIA, $3,000 worth of approved
specialised equipment was supplied but sat idle because the client had no
device to control it. The stand-off rolled on for months and then became years.
Phantom approvals for a tablet appeared then disappeared. The equipment, now
well out of date, was sent to the NDIA and sits in a box somewhere. The client
never received their system.[26]
3.27
Ms Olsson from the Speech Pathology Australia summed up the situation
succinctly:
There's a focus on the item rather than the purpose or the
outcome.[27]
3.28
Mrs Rachel Tosh, Director, Therapy Alliance Group, provided a similar
example illustrating that the Agency's decision-making process does not
consider what barriers are being overcome by a particular piece of equipment:
As an example, we submitted a request for an iPad and a
Proloquo2go. It was rejected. The NDIA representative suggested the alternative
of an Android tablet, which doesn't support the apps that the client was
already using for communication. The iPad and Proloquo2go were $2000. The alternative recommended by NDIA was $7,000, hadn't been
trialled with the client and was not appropriate to that client's needs, and
the application for the iPad and Proloquo2Go was rejected.[28]
3.29
ILC WA pointed out that many specialist products do not allow for
testing prior to purchase, limit options for local setup and repairs, and are
quickly obsolete due to emerging technology.[29] It argued many devices have now crossed into mainstream markets, and not
including them in plans can leave consumers with outdated and complicated
equipment or none at all.[30]
3.30
The committee heard that policy ambiguity has led to some inconsistency
across plans, whereby some participants have had devices funded while others in
similar circumstances and with similar needs have not.[31]
3.31
In advice to the committee, the Agency confirmed that tablets,
smartphones, and phone and data plans are generally considered day-to-day
living costs, and are therefore not NDIS fundable. However, it is Agency policy
to fund tablets when it is a stand-alone communication device required due to a
person's disability.[32]
3.32
Dr Emily Steel argued there is a need to define what 'AT' covers as
there is an assumption it is about products, rather than products and services.[33] Indeed, the Agency's definition of AT stipulates that AT is 'any device or
system that allows individuals to perform tasks they could not otherwise do'
which seems to imply a focus on products.
Committee view
3.33
Mainstream technology such as iPads have been transformational in the
field of AT. The committee has heard countless examples of where the platform
has provided for an extensive range of communication aids. The apparent ban on
funding them because they are mainstream technology seems to disregard the many
positive reported outcomes of the use of the technology, and the associated
applications. The committee urges the Agency to make decisions based on
outcomes rather than a funding ban on technology that has the potential to
deliver those outcomes.
Recommendation 5
3.34
The committee recommends that the NDIA makes funding decisions based on
outcomes rather on whether the item is considered mainstream, or could be used
beyond its AT purpose.
Knowledge of planners
3.35
Poor quality plans were linked to a lack of knowledge and experience
amongst NDIS local area coordinators (LACs) and planners. Feedback suggests
there is limited understanding among staff about the impact different
disabilities can have on individuals and the appropriate AT solutions.[34]
3.36
The committee heard that some plans have missed key AT items:
We are concerned that due to a lack of education and training
for Planners and Local Area Coordinators, as well as staff attrition, this has
also caused distress for some Participants who have experienced key items being
missed on their Plan. This has been particularly the case where a Participant
lacks confidence or capacity to self-advocate and/or is unsure of what AT (or
other items/services) would assist them to achieve their goals and aspirations.[35]
3.37
Submitters reported some participants, despite their own limited
knowledge, were having to educate planners and LACs:
Limbs 4 Life has received numerous phone calls from educated,
intelligent and positive people who, when entering the NDIS, are immediately
thrown into a world they know nothing about. They need to be proactive,
assertive and advocate on their own behalf to justify their needs and goals but
without any tools (other than that provided by Limbs 4 Life) to do so. They
have subsequently been thrown into a situation whereby they need to educate
their Planners and LACs, who more often than not have a limited understanding
of the unique needs of people living with limb loss, to ensure that the
Planners understand what needs to be included in their Plan.[36]
3.38
Able Australia argued that some planners are not aware that some devices
may not be complex on their own, but when used together they must be configured
for the participant and thus require additional funding:
Deafblind users often need a range of hardware, software and
accessories that combine to provide "the device" and each of these
components are from different suppliers. Bought separately they may not require
an assessment but they combine to provide a holistic solution. The device
should be recognised as a Category 3 complex device and receive adequate
funding to customize the configure the device so that the participant can use
it. There is limited expertise amongst planners to navigate this process and
often breaks down.[37]
3.39
Ability Research Centre reported that some plans include funding for the
AT product but omit associated set up, customisation, and training costs:
...NDIA staff often seem to be unaware of the essential AT
services that are needed to implement and/or complement AT systems, and the
additional funding therefore required. It is commonplace for planners to
include a provision for "assistive technology" in a participant's
plan, without additional funding for the services required to assess their
needs, set up and customise their AT system, or train them in its use.[38]
3.40
The NDIS AT Strategy identified there is a 30 per cent
abandonment rate of AT when individuals do not understand how to properly use
their equipment or devices.[39]
3.41
Amaze argued that insufficient training budgets can undermine the
benefits of the Scheme for participants. It expressed concern that none of the
42 respondents to its survey reported receiving funding for AT training in
their plans:
We are concerned that training is not generally being funded
to support participants and their families to use complex AT. Without
appropriate training, the use and cost-effectiveness of funded AT can be vastly
undermined...In particular, if funding is provided for a communication app,
funding must also be provided for a parent/carer and relevant others (including
education providers, employers, etc.) in how to use it. This training needs to
be ongoing to ensure its use is sustainable and evolves to meet the evolving
needs of the user.[40]
Ability to understand and predict
AT needs
3.42
The Scheme's individualised planning approach is predicated on the
ability of participants to understand their disability, their requirements, the
AT options available, and then advocate for their preferred AT solution.
However, many participants, and their families and carers, are not well
informed about disability or AT in general, and are unable to advocate strongly
for their needs.
3.43
This is amplified for individuals and families with a newly acquired or
complex disability and those dealing with sophisticated and ever-changing
technology:
...amongst the amputee population very little is known about
accessing prosthetic trials, gaining access to a physiotherapist for further
gait training and/or support from Occupational Therapists for upper limb device
training. People living with limb loss are users of some of the most complex
and technical AT devices required to live an ordinary life. This cohort
sometimes uses advanced complex prosthetic and other AT devices; with
engineering and technology advancing at a rapid pace in this particular space.
In light of this the vast majority of consumers, regardless of whether they
have lived with limb loss for decades or only months, are not aware of the AT
available to them.[41]
3.44
ILC WA argued that it takes a skilled clinician to understand and
forecast appropriate AT and associated services:
With complex AT, it takes an experienced and skilled AT
clinician to see, mitigate, and plan for future issues...Under the NDIS this
decision and planning is left to the responsibility of the participant who
often don't hold or value this knowledge and may solely rely on suppliers or
their own social networks.[42]
3.45
Limbs 4 Life pointed out that the NDIS has been a crash course for many
individuals:
For many, the process has been a crash course in education,
the ability to self-advocate, an urgent need to understand their disability
requirements, while simultaneously trying to understand and interpret new
NDIS-related processes...With the rollout of the NDIS individuals
are required to have a complete and thorough understanding of the NDIS process
and structures or risk having their AT needs not met.[43]
National accreditation for AT
practitioners
3.46
In response to a lack of knowledge across all stakeholders, some
submitters proposed a national accreditation system for allied health
professionals that recognises skills, knowledge, and experience in AT.[44] As pointed out by ARATA, a lack of accreditation makes it difficult for NDIS
participants to determine who can provide appropriate and quality AT services.[45]
3.47
There are varying levels of AT knowledge held by prescribing therapists,
and no minimum competencies or standardised skills across the sector. There are
concerns some may be relying solely on the advice of AT suppliers which raises
questions around conflict of interest.[46] Indeed, Dr Ken Baker argued that, with the future uncertain for state-funded
independent living centres, independent advice and the ability to trial AT in a
neutral environment is at risk of being lost.[47]
3.48
Previous work undertaken by ARATA and Assistive Technology Suppliers
Australia identified the need for a credentialing and accreditation system that
recognises competence and sets minimum practice standards for providers and
suppliers.[48] The project found that regulatory schemes such as accreditation can achieve:
-
reduced abandonment of assistive products;
- greater efficiency by directing demand for higher or lower
practitioner competence based on risk and complexity;
- consolidation of knowledge amongst practitioners;
- agreement on necessary AT competencies.[49]
3.49
The project reviewed national and international systems and recommended
an approach to establishing an Australian national accreditation system for AT
practitioners and suppliers.[50]
3.50
The committee acknowledges that some professions, such as orthotists and
prosthetists, are already required to undertake core competencies in AT and
should therefore not be subject to additional requirements.[51]
3.51
SWEP in Victoria provided information on their Registration and
Credentialing Framework, which currently has over 8000 providers across all
Allied Health and medical staff with the knowledge and skills required in the
prescription of all types of AT. Key features include:
-
Threshold credentials for each AT category;
- Performance expectations of prescribers at each level (green,
amber and red);
- Client characteristics that may impact prescription;
- Robust, accountable and credible system that defines standards of
competence;
- A matrix for categorisation of AT, client and prescriber; and
- Standards for minimum requirements for registration.[52]
3.52
According to the their submission, SWEP's 'traffic light' system works
in the following way:
SWEP credentialed prescribers are allocated a traffic light
colour for each AT category which relates to their formal qualification
(threshold credentials), years of experience, frequency of prescribing AT and
continuing professional development (CPD). A 'white' prescriber provides
administrative support to registered prescribers only, they cannot prescribe. A
'green' prescriber can prescribe AT for clients that is considered non-complex.
An 'amber' prescriber will have a higher level of expertise and experience,
while a 'red' prescriber is recognised as an expert in their field.[53]
3.53
Speech Pathology Australia supported this model which they claim will
build the capacity of the sector as a whole:
The Association supports a model similar to one employed by
the Victorian State-wide Equipment Service which can offer the scaffolded
supports whereby providers can develop the knowledge, skills and expertise
about AAC AT, helping to build capacity in the sector as a whole.[54]
Emphasis on value for money
3.54
Striking a balance between adequate funding for individuals whilst
ensuring Scheme sustainability is no easy task. There are concerns that the
NDIA is placing undue emphasis on value for money at the expense of
participants' outcomes.[55]
3.55
The NDIA's operational guidance states that the Scheme will only fund
the minimum necessary or standard level of support required to meet the
functional specifications needed to meet the participant's goals.[56] However, submitters argued there is usually a reason why a more expensive
option has been recommended.[57] Vision Australia pointed out there are many elements to a therapist's
recommendation or a participant's preference:
...things such as the design of the user interface, prior
experience, the amount and availability of training and support, ergonomic
considerations, reading and learning preferences, cognitive function and many
more. These are often not given any consideration due to the planner's
insistence on getting a cheaper product that, in their opinion, is equivalent.[58]
3.56
Therapy for Kids et al made a similar argument:
Items can be rejected with the suggestion that a cheaper item
of similar characteristics should be suitable. An understanding of how an
assistive technology item removes a barrier in participation or activity for a
participant assists in identifying why an item has been suggested by a therapy
provider. Often a similar or cheaper product does not remove the barrier being
experienced by the participant and is therefore a meaningless purchase.[59]
3.57
The concerns were echoed by Develop Therapy Services:
Planners do not always have the appropriate skills to decide
to approve or not approve specific items. Approval seems to be based largely
around the cost of the recommended AT when there are multiple factors to
consider, as we have listed above. It is false economy to provide a cheaper
alternative if it results in injury or lost opportunity to the participant.[60]
3.58
WA OTA argued that participants may choose AT suppliers based on
reputation and reliability but that these preferences are being disregarded for
cheaper alternatives.[61]
3.59
Vision Australia argued that a focus on cost rather than outcomes places
progress in AT innovation at risk as new solutions that may be marginally more
expensive are rejected.[62]
Committee view
3.60
The committee heard evidence that the focus on value for money, is more
a focus on bottom line cost, rather than value. The committee fully understands
the pressure the Agency is under to ensure the sustainability of the Scheme. However,
a focus on monetary value alone disregards the tangible outcomes that will
ensue if participants have access to the appropriate assistive technology that
will assist them in being as physically, socially, and economically
participative in society as possible.
3.61
The committee welcomes the continuous efforts of the agency to improve
the capability of its decision makers. However, it is at a loss to understand
why the Agency has not utilised the expertise and experience of state and
territory systems. The credentialing model employed by SWEP in Victoria seems
to offer a robust, logical, cost effective, equitable, and efficient system for
ensuring the best possible outcomes for both participants and funding bodies.
The committee strenuously suggests that the Agency does not re-invent the wheel
yet again by attempting to design a model with all the features of the models
in place before the Scheme rolled out, but with much worse outcomes for all
stakeholders, including tax payers.
Recommendation 6
3.62
The committee strongly recommends that the NDIA adopt the SWEP
credentialing model for prescribing Assistive Technology.
The supply of AT
Market conditions
3.63
Much of the success of the NDIS overall relies on providers of services
coming into the Scheme to provide the choice and control that underpins the
ethos of the Scheme. Competition within the AT market supply and provision is
similarly essential to ensure the cost effective provision of equipment.
3.64
The NDIA provided evidence that they are exploring various options with
the sector to develop initiatives to stimulate choice and competition in the
market place.
3.65
Dr Lloyd Walker, Special Advisor, Assistive Technology and Home
Modifications, NDIA, explained:
...you have to recognise the agency's priority is to work
within a market system. [...] I was having a conversation yesterday with a
provider who has a very close link to a fleet car organisation about offering
fleets of very expensive power wheelchairs and vehicle modifications. The
agency would fund into a participant's plan effectively a lease. We would lease
off that fleet. That would cover their repairs, their maintenance. If they need
to change it, they could get it changed at a moment's notice pretty much. And,
potentially, they can add in a bit more money and lift the bar and go to higher
product, if that is what they want as well.[63]
State and territory systems
3.66
Given the extensive delays, and supply issues around the provision of
AT, the committee welcomed information on the seemingly extensive stores of AT
held by states and territories, and the apparently highly efficient procurement
and supply processes that were in place prior to the roll out of the NDIS.
3.67
Therapy 4 Kids described the ACT model as being a good exemplar:
The ACT's state model was particularly quick. Sometimes I
would get an answer within 24 hours, often within a week and always within a
month. For items that were more expensive, it was within three months.[64]
3.68
The body responsible for AT in NSW is Enable NSW who operate the Aids and
Equipment Program (AEP). Enable NSW is also a registered service provider to
the NDIA and can 'provide co-ordination of equipment supports approved in NDIS
Plans (for example placing orders for new equipment, ordering consumable
products or contacting suppliers to arrange repairs)'.[65]
3.69
EnableNSW also provide prosthetic and orthotic manufacturing services,
specifically for people in regional and rural NSW, which is again a registered
service provider to the NDIS:
...we operate two prosthetic and orthotic manufacturing
services in rural areas, which ensure people living in regional and rural New
South Wales have access to a service that would be otherwise unavailable. We
anticipate these services will continue to offer registered provider services
to NDIS participants who choose them on an ongoing basis.
3.70
EnableNSW provided a summary of their main KPIs for both internal and
external processes for Aids and Equipment and for Prosthetics:
INTERNAL
– AIDS AND EQUIPMENT
(i) Customer
service and processing times |
KPI |
Incoming calls |
Average Speed
of Answer < 40 sec |
Email response |
< 24 hours |
Repair lodged with provider |
< 24 hours |
Re-order lodged with provider -
continence, Home Enteral Nutrition (HEN) |
< 2 days |
Quoted equipment request* to purchase
order |
<10 days |
Refurbished stock request* to delivery
bay |
<5 days |
*Assumes complete application
EXTERNAL
– AIDS AND EQUIPMENT
(ii) Equipment
request (order placement to delivery) |
KPI |
Order delivery – continence, Home
Enteral Nutrition (HEN) |
<
10 days |
Refurbished stock delivery bay to
home |
< 14 days |
INTERNAL
– PROSTHETIC LIMBS
(i) Prosthetic
Limb Service Metrics (request to approval/order) |
KPI |
Interim Limb (first limb
post-amputation surgery) approval |
< 24
hours |
Replacement limbs and sockets |
<14 days* |
Minor repairs under $700 |
Immediate |
Minor repairs ($700-$2000) – where
provider telephones EnableNSW for approval |
Immediate |
*NB: EnableNSW guidelines are published and consistent so many providers
commence work ahead of approval
EXTERNAL – PROSTHETIC LIMBS
(ii)
Prosthetic
Service Provider Metrics (funding approval to delivery) |
KPI |
Interim Limbs (metro) |
5 days |
Interim Limbs
(rural/regional) |
17 days |
Replacement limbs or
sockets (metro) |
10 days |
Replacement limbs or
sockets (rural/regional) |
15 days[66] |
|
|
|
|
3.71
Currently, in Victoria, SWEP is working 'within an informal 'business
as usual arrangement' with the Agency'[67] subject to ongoing discussions. This arrangement follows SWEP being the 'in-kind'
provider for the Scheme throughout the trial phase up until 2016.[68]
3.72
SWEP provided a late submission to the committee, outlining some of the
key features of their program. According to the submission the model is
designed to respond to funding bodies, and the needs of participants with a
model that:
...encompasses an integrated approach to provide assurance that
equipment provided to AT consumers is best fit for purpose and best value for
money. This approach also allows AT consumers to exercise choice and control
considering parameters such as safety, functionality and durability, within the
context of the funding body's requirements for dignity of personal risk for
their consumers.[69]
3.73
The SWEP system has some features which appear to address precisely many
of the problems the Agency is facing. Aside from the credentialing of providers
discussing earlier in this chapter, the SWEP submission highlights how it
operates in the following areas:
- Assessor Support;
- Infrastructure & Governance Framework;
- Repairs;
- Refurbished Equipment;
- Priority of Access;
- Strategic Procurement; and
- Organisational Agility.
3.74
In terms of waiting times, witnesses and submitters supported the claims
of SWEP and other state services, that their systems were significantly more
efficient and timely than the NDIS model.[70] For example:
...previously, under the State-wide Equipment Program, if
something was urgent, we were able to phone the SWEP program, speak to someone,
and equipment was often funded within 24 to 48 hours.[71]
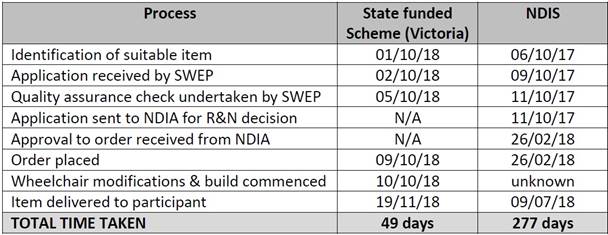
3.75
SWEP's submission provided a table[72] illustrating the difference in response times for the provision of a highly
customised powered wheelchair:
3.76
However, the committee did receive evidence from the Australian Orthotic
and Prosthetic Association that, in the case of orthotics and prosthetics, it
was the use of state schemes that was causing the extensive delays and called
for the practice to be halted. The Association provided the following example
of the system malfunctioning:
A participant in Victoria visited an orthotist for an
assessment to receive a knee-ankle-foot orthosis. An application for funding
was submitted to the Victorian State Scheme (State-Wide Equipment Program)
portal and was only forwarded to the NDIS after one month. After being approved
by the NDIS after another month, the order has been delayed in the SWEP
administrative process for two months and the practitioner is unable to provide
the service. This delay is caused by both SWEP and the NDIS.[73]
3.77
This view is supported by other groups who reported that since Scheme
rollout, there have been considerable delays for AT for some participants
through these state-based equipment programs:
The transition in Victoria has caused a significant backlog
for AT provision for both NDIS and Department of Education and Training (DET)
funded clients. DET clients are now going on a SWEP waitlist, with the majority
being told they will not receive equipment until they receive their NDIS plan
(currently occurring in Bayside and Southern regions as they roll into the
NDIS).[74]
3.78
However, the model under state systems was different, and often
equipment provided under those systems was not fully funded, requiring the
participant to either contribute or access additional funding through charities:
Under the State-wide Equipment Program in Victoria, equipment
was funded based upon risk, so urgent equipment was funded fairly quickly; less
urgent equipment took longer. Some equipment, as I said before, could be funded
within 24 to 48 hours. The challenge that the State-wide Equipment Program had
in its funding model is that not all equipment was wholly funded. If we think
back a couple of years you might have a wheelchair where part of the wheelchair
was funded and then families were required to access charities, so the charity
part of the funding model would take anywhere up to a year or two years to gain
that funding. We appreciate, under the NDIS, that it is wholly funded, but the
time frames that we're looking at at the moment are anywhere above six to 12
months for that funding to come through.[75]
3.79
Dr Walker from the NDIA also pointed out that the NDIS facilitates a
much more holistic evaluation of the participant's needs, beyond simply the
assistive technology:
One of the big differences between the NDIS and state
programs is the NDIS is a funding program to give participants access to a
support. Most of the state programs focus on offering a fleet of equipment from
which the participants receive. You've heard from Ms Hiller about EnableNSW's pool
of equipment that they make available to participants. When a participant in
New South Wales wants to draw off EnableNSW, they put in a request for a
wheelchair, whereas, when they're approaching the NDIS, we are looking broadly
at what their range of supports might mean, which is a combination of whether
it's personal care support, a wheelchair, transfer equipment or modification of
a house—all of those are potentially in play. That sometimes adds to the length
of time in considering what the most appropriate option is.[76]
Committee view
3.80
The committee heard compelling evidence on the efficiency of the
operation of AT equipment services in states and territories prior to the NDIS.
The time periods between the necessary equipment being identified, provided and
used appropriately and safely, has blown out significantly under the NDIS.
According to evidence this is because of a duplication of application and
assessment processes.
3.81
The committee understands that the NDIA cannot completely outsource its
assessment procedures to state agencies, however the current situation is
unworkable, and is producing unacceptable delays. The Agency has to decide on
one process or the other. Given the experience, skills and expertise of the
state schemes, the committee suggests that the Agency enter into agreements, or
Memorandums of Understanding with them to process and manage applications
instead of the Agency.
Recommendation 7
3.82
The committee recommends the NDIA explore entering into agreements with
state schemes for the prescription, assessment, and delivery of Assistive
Technology to NDIS participants.
State-based loan pools
3.83
The committee also heard suggestions that loan pools and leasing
arrangements should be utilised to assist some participants to access AT
temporarily in a cost effective way.[77]
3.84
Therapy for Kids et al argued that one of the reasons for delays to AT
is the purchasing of new equipment. It suggested wait times for AT could be
reduced by allowing NDIS funding to be used to access state-based loan pools of
equipment through the State-wide Equipment Program (SWEP):
SWEP has a reissue database. Especially for children, items
are often used for 4 years due to growth. SWEP's repairs and maintenance
program services the items and makes them available for reissue. Currently NDIS
participants 'own' the items and are giving them away or selling them after
they are no longer needed. Making use of existing state-based infrastructure to
reissue AT items would make a difference to times to receive AT in some
instances and would be a budget saver for the NDIA.[78]
3.85
The Australian Physiotherapy Association made a similar argument:
We understand that Victoria has an excellent and well established
re-issue system and pool of equipment with an excellent, well maintained
database for re-issue. This is easy to use and provides great solutions for
people with disabilities. It is a very cost effective way for this equipment
that is still in working order but not able to be used for another person.[79]
3.86
Dr Ken Baker, Principal Advisor, National Disability Services, argued
that these systems are valuable for urgent and short term use:
The second strength under some of the state systems, although
it was patchy, was access to recycled equipment for people, often either
children—children's needs for equipment can change quite rapidly, so it often
makes sense to get equipment, use it for a short term and then for that
equipment to be recycled and used by other children—or people with rapidly
deteriorating neurological conditions where they don't want to wait long for
equipment, they need equipment now and they won't need it for long. [80]
3.87
Speech Pathology Australia were also supportive of a loan system for AT.
According to their evidence, the NDIA should support:
...a 'library' system for AAC AT to provide participants with
the ability to trial equipment, to ensure they are able to identify the best
AAC AT solution for them.[81]
3.88
The NDIA explained that, for participants with degenerative conditions,
planners can include a funding budget for accessing AT pools operated by
specialist organisations (such as the Motor Neurone Disease Association of NSW)
or state and territory AT programs.[82]
3.89
However, it pointed out that not all participants will be able to access
state-based equipment loan pools. This is because delegates must consider the
cost of purchasing or leasing equipment when determining whether AT supports
represent value for money.[83] It also highlighted that not all government-operated state-based loan pools
offer a hire service, some state programs do not provide supports to 'self-managed'
NDIS participants, although, in these cases, participants can have AT supports 'agency
managed' so they can hire through these programs.[84]
3.90
Ms Suzie Green, Team Leader and Senior Physiotherapist, Noah's Ark,
noted that, in Victoria, NDIS participants were no longer allowed to access the
SWEP loan of equipment:
In the current system in Victoria we have the State-wide
Equipment Program, which previously had a very large loan pool. Recently their
rules changed in terms of: if you were NDIS funded, you were not able to access
the loan pool. So, there is a very large loan pool at the State-wide Equipment
Program which is available for SWEP funded clients but not for NDIS funded
participants. I think they're expecting that, as more equipment is purchased by
the NDIS, that pool will increase, but at this point it's very small.[85]
3.91
With the introduction of the NDIS, EnableNSW ceased its communication
devices loan pool:
We don't any longer, but we did run a communication devices
loan pool, and that particularly helped with some of the issues that have been
addressed this morning about the need for items to be in place and used for a
good long period. We had a month where allied health professionals could get
them out of the pool and work with them themselves and become familiar with
them but also could leave them with a participant for a month and have them
programmed for them to give them time to prove they could use them and that
they were effective for them before they would go on to actually request the
item... The demand for that fell away with the NDIS. As we slowly assessed that
situation, we returned the remaining items to clinical services that had a need
for them for people who were outside of the NDIS, particularly in the area of
degenerative conditions, because it was not being accessed.[86]
3.92
While the Agency has not yet had discussions with Enable NSW regarding
its plans to establish a coordinated pool of common AT across NSW community
health facilities by July 2019,[87] it is considering whether to extend arrangements to assist participants to
access government coordinated stock equipment and the impact this may have on
the market.[88]
Recycling of equipment
3.93
The committee heard there is not currently a centralised system to
recycle AT equipment that has been bought through the NDIS but is no longer
required by the participant.[89] Mr Enis Jusufspahic, National Manager, Sector Development, ECIA, explained that
families and business are simply running their own informal loan pools:
There's no formal way of recycling it, so, at the moment,
providers take it upon themselves, with the families that they work with, to
ask them to bring in the equipment that they're not using, and then they would
maintain it and repair it and loan it back out to other families. They would
run their own loan pools, essentially, but there is no formal way of managing
this, from a scheme perspective.[90]
3.94
The committee heard that families are selling and buying AT through
platforms such as eBay, as a way to circumvent the delays of the NDIS:
If it's an item that they've seen for sale that someone else
has had, they'll say: 'I've seen that on eBay, I know that's what we want and I
know we're about to go through all the trials and all the documents in the next
12 months. What if I just sell this and buy that?' If it's an item that they
can readily access second-hand, they'll often choose that.[91]
3.95
EnableNSW noted that access to its equipment recycling and reissue
program would save the Scheme a considerable sum of money each year:
...at the request of the NDIA, we provide some services under
working arrangements as a registered provider. These working arrangements
expire on 30 June 2019. New South Wales accepted the request to provide these
services in order to share our expertise in assistive technology provision, and
to support access to cost-effective assistive technology through our equipment
recycling and reissue program and our contract arrangements. At the time of the
initial request, the NDIA found that in relation to AT access to information,
some specific contracted items, and recycling and reissuing equipment that the
NDIS could save $161 million per annum. This would clearly assist scheme
sustainability, and those details are in the NDIS AT strategy.[92]
3.96
The program in NSW drew from more mature programs in South Australia,
and from New Zealand:
The most developed program is in South Australia. We and
South Australia probably based a lot of our learnings on Enable New Zealand,
which has had a very mature recycle and reissue program, but there are also
programs throughout Europe and the UK.[93]
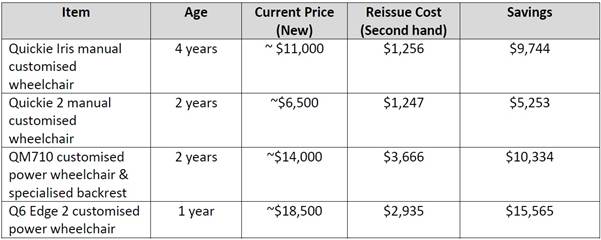
3.97
SWEP in Victoria compared the typical cost of buying new wheelchairs,
with the cost of refurbishing them:[94]
3.98
Speech Pathology Australia were strongly of the view that the expertise
and experience of the state specialised equipment services should be retained,
and accessible to NDIS participants:
We feel it is essential that the NDIA ensures continued
access to supports such as those provided by the former specialised equipment
services including: - a 'one-stop' centre of support, providing access to AT
Advisors who can offer independent advice as well as direct supports (i.e.
assessment, training, set up and support for equipment trial, individualised
set up of AT) and/or capacity building supports to participants, primary
therapy providers and others.[95]
3.99
The NDIA is consulting and engaging with the AT provider sector to
develop a coordinated approach to services that can acquire, refurbish, resell
and when appropriate, recycle used AT. It advised that the next workshop with
AT providers on this topic is scheduled for late November 2018.[96]
Committee view
3.100
Loan pools, recycling and refurbishment of assistive technology have
long since been a feature of any aids and equipment programs. The NDIS model,
with an emphasis on an individual bespoke solution for each participant, does
not sit easily within those previous systems.
3.101
However not every AT solution is a fully customised piece of technology
that can only be utilised by its intended recipient. There are thousands of
standard items that the committee heard were being purchased at high cost, on
an individual basis, and not being recycled or res-used afterwards. Evidence to
the inquiry suggested that there were improvements and efficiencies possible
across the board, on processes and procedures, as well as significant cost
saving opportunities.
Recommendation 8
3.102
The committee recommends that the NDIA undertake an urgent review of all
aspects of its AT delivery model, with specific focus on how it can utilise current
state and territory equipment schemes, including bulk-purchasing, loan and
recycling programs.
Hon Kevin Andrews MP
Chair
Senator Alex Gallacher
Deputy Chair
Navigation: Previous Page | Contents | Next Page
|