Introductory Info
Date introduced: 18 September 2019
House: House of Representatives
Portfolio: Health
Commencement: Schedules 1 to 5 commence on 1 July 2020. Schedule 6 commences immediately after schedules 1–5. All other sections commence on Royal Assent.
Purpose of the Bill
The purpose of the Medical and Midwife Indemnity
Legislation Amendment Bill 2019 (the Bill) is to amend the Medical Indemnity
Act 2002 (MI Act), Medical Indemnity
(Prudential Supervision and Product Standards) Act 2003
(MI(PS&PS) Act) and the Midwife
Professional Indemnity (Commonwealth Contribution) Scheme Act 2010
(MPICCS Act) to:
- simplify the current legislative structure underpinning the
Government’s support for medical indemnity insurance
- repeal redundant legislation
- remove the existing contract requirements for the Premium Support
Scheme (PSS) and incorporate the necessary requirements in legislation
- require all medical indemnity insurers to provide universal cover
to medical practitioners
-
maintain support for high cost claims and exceptional claims made
against allied health professionals and enable exceptional cost claims to be
made, which is provided for in a separate scheme to medical practitioners
- support high cost claims and exceptional cost claims made against
private sector employee midwives not covered under the Midwife Professional
Indemnity Scheme (MPIS)
- clarify eligibility for the Run-off Cover Scheme (ROCS) and
permit access for medical practitioners and eligible midwives retiring before
the age of 65
- cause an actuarial assessment to report on the stability and
affordability of Australia’s medical indemnity market, with the report to be
laid before each House of Parliament and
- streamline reporting obligations and improve the capacity for
monitoring and information sharing.[1]
These amendments are designed to support the long-term
stability and affordability of medical indemnity premiums for medical
practitioners.
Structure of the Bill
The Bill contains six Schedules:
- Schedule 1 removes redundant legislation by repealing the Medical Indemnity
(Competitive Advantage Payment) Act 2005 (Competitive Advantage
Payment Act) and the Medical Indemnity
(UMP Support Payment) Act 2002 (UMP Support Payment Act) and
making associated consequential amendments to other legislation that refer to
those Acts
- Schedule 2 clarifies eligibility under existing claim schemes:
- Part
1 provides clarity for the claiming criteria under the High Cost Claims Scheme
(HCCS) relating to aggregation of claims (where the claim/s is/are against the
same medical practitioner or in relation to the same incident or series of
incidents)
- Part
2 amends relevant provisions in the MI Act to clarify that the HCCS and
the Exceptional Claims Scheme (ECS) are only intended to apply to medical
practitioners (as distinct from allied health professionals)
- Part
3 will allow greater access to the ROCS for medical practitioners and eligible
midwives who permanently retire before the age of 65 by removing the current
age restriction
- Part
4 provides that medical and midwife indemnity claims will only relate to
incidents that have occurred in connection with a health service
- Schedule 3 deals with administrative changes intended to
streamline and/or clarify the operation of the legislation, including more
efficient information sharing, the use of computerised decision-making by the
Chief Executive Medicare (CEM) and an actuarial evaluation of the affordability
and stability of the medical indemnity market by February 2021
-
Schedule 4 provides for the restructure and consolidation of
delegated legislation and creates the power of the Minister to make rules
required or permitted by the MI Act, or necessary or convenient for
carrying out or giving effect to that Act
- Schedule 5 sets out the requirements for universal cover and
- Schedule 6 creates high cost claim and exceptional claims schemes
for allied health professionals, including private sector midwives.
Background
Medical indemnity insurance provides financial protection ‘to
both medical practitioners and patients in circumstances where a patient
sustains an injury (or adverse outcome) caused by medical misadventure,
malpractice, negligence or an otherwise unlawful act’.[2]
In Australia, it is compulsory for all registered health professionals to hold medical
indemnity insurance under the Health
Practitioner Regulation National Law Act 2009 (National Law).[3]
Subsection 129(1) of the National Law provides:
A registered health practitioner must not practise the health
profession in which the practitioner is registered unless appropriate
professional indemnity insurance arrangements are in force in relation to the
practitioner’s practice of the profession.
Currently an exemption from this requirement applies under
section 284 of the National Law for privately practicing midwives who
provide intrapartum services (labour and delivery) for women having homebirths.
This exemption applies until 31 December 2019.[4]
Government
support for medical indemnity
Prior to 2002, medical indemnity insurance was
traditionally provided by medical defence organisations (MDOs), not-for-profit
mutual organisations that offered discretionary indemnity cover as a benefit to
members in return for an annual subscription.[5]
In May 2002, the largest MDO in Australia, United Medical Protection (UMP) and
its wholly owned subsidiary Australian Medical Protection Limited (AMIL), was
placed into provisional liquidation. It was estimated that the collapse of UMP
would leave up to 60 per cent of medical practitioners in Australia without
professional indemnity cover.[6]
At the same time, insurers were experiencing pressure due
to increased claim costs, a fall in investment returns and for some MDOs, a
failure to make sufficient provisions for ‘incurred but not reported claims’
(claims that may occur many years in the future). Further, medical
practitioners were facing increased premium costs (as high as one third of
their incomes) and considering leaving the profession or ceasing high-risk
procedures. [7]
As a result of these issues, between 2002 and 2010, the Australian
Government implemented a range of financial and regulatory measures designed to
support the medical indemnity insurance industry, including: premium subsidies;
government assistance for high-cost claims; and placing providers of medical indemnity
insurance under the regulatory supervision of the Australian Prudential
Regulatory Authority (APRA). These measures were underpinned by tort law
reform at the state and territory level.[8]
Indemnity
Insurance Fund
During the period 2003–10, seven discrete schemes to
provide medical and professional indemnity support for medical practitioners
and midwives were established (see Table 1). In 2011, these schemes were
consolidated under the Indemnity Insurance Fund (IIF), which is administered by
the Department of Health. The primary objective of the IIF is to streamline the
administration of the seven schemes with the following priorities:
- promote stability of the medical indemnity insurance market
- keep premiums affordable for doctors in private practice and
-
ensure availability of professional indemnity insurance for
eligible midwives.[9]
Table 1: schemes
within the Indemnity Insurance Fund
|
Scheme
|
Purpose and key features
|
|
Premium support scheme (PSS)a
|
The PSS assists eligible
doctors with the costs of their medical indemnity insurance through
reductions in the level of premiums charged to them by their medical
indemnity insurer. The PSS currently subsidises 60% of indemnity costs for
doctors whose premiums exceed 7.5% of their income from private practice.
The applicable subsidies under
the PSS have decreased since its introduction. Previous subsidies were:
-
80% from 2004 to 1 July 2012 and
- 70% from 1 July 2012 to before 1 July 2013.
Procedural
GPs working in rural areas (Rural, Remote and Metropolitan Areas 3-7b)
are eligible for PSS regardless of whether they meet other PSS eligibility
criteria. The PSS will cover 75% of the difference between premiums for these
doctors and those for non-procedural GPs in similar circumstances.
|
|
Run-off Cover Scheme (ROCS)c
|
The ROCS is designed to provide
secure ongoing insurance for doctors who have ceased private practice because
of retirement (after the age of 65), disability, maternity leave, death, or
if they discontinue working as a doctor in Australia.
The Australian Government pays
100% of the costs of valid claims (including the costs of managing claims) made
against eligible doctors.
The ongoing costs of the scheme
are met by the ROCS Support Payment, a levy on the premium income of medical
indemnity insurers.
Currently
a private medical practitioner who leaves the workforce for a reason other
than those outlined above, or who retires before the age of 65, will not be
eligible for ROCS for a period of three years. As such, those practitioners
must purchase run-off cover from their medical indemnity insurer for the
three year period if they wish to remain insured. This Bill seeks to permit
access to ROCS for medical practitioners and eligible midwives retiring
before the age of 65.
|
|
High Cost Claims Scheme (HCCS)d
|
The
HCCS is intended to place downward pressure on premiums, particularly for
doctors in high risk areas, by lowering the amount that insurers pay out and
reducing the amount of reinsurance medical indemnity insurers need to buy to
fund large claims.
Under
the HCCS, the Australian Government will reimburse medical indemnity insurers
50% of the insurance payout over $300,000 up to the limit of the
practitioner's cover, for claims notified on or after 1 January 2004.
From
1 July 2018, the threshold for claims under the HCCS was amended from
$300,000 to $500,000. The new threshold will be applied to claims notified to
insurers on or after 1 July 2018.
|
|
Exceptional Claims Scheme (ECS)e
|
The
ECS covers health practitioners for 100% of the cost of private practice
claims that are above the limit of their medical indemnity insurance
(generally $20 million), so that they are not personally liable for
exceptionally high claims. These claims can be either a single very large claim
or an aggregate of claims related to an incident that together exceed a
threshold for a contract's limit.
Health
practitioners are not required to make a contribution towards the ECS. It is
fully funded by the Government.
|
|
Incurred But Not Reported (IBNR)
Indemnity Schemef
|
The IBNR Indemnity Scheme
covers unfunded medical insurers’ liabilities that were incurred but not
reported as at 30 June 2002. The Government covers 100% of claims.
At present, only one insurer, United
Medical Protection Limited (now known as Avant Insurance Limited)
participates in the IBNR Scheme.
|
|
Midwife Professional Indemnity
(Commonwealth Contribution) Scheme (MPIS)g
|
The MPIS provides financial
assistance to eligible insurers who provide indemnity to eligible midwives. The
MPIS was introduced in 2010 to address concerns that privately practicing
midwives were unable to access professional indemnity insurance cover from
commercial insurers (see further information below).
Payment rates:
-
under the MPIS, the insurer pays the first $100,000 for each
claim
- Level 1 Commonwealth contribution payments – for each claim
over $100,000, the Government will pay, via the insurer, 80% of the cost that
exceeds the threshold, up to a ceiling of $2 million
- Level 2 Commonwealth contribution payments – for each claim
that exceeds $2 million, the Government will pay, via the insurer, at the
Level 1 rate for the first $2 million, plus 100% of the cost of the claim
above the threshold.
There is currently only one
provider of professional indemnity insurance for privately practising
midwives.
|
|
Midwife Professional Indemnity
Run-off Cover Scheme (Midwife ROCS)g
|
The Midwife ROCS provides
secure ongoing insurance for eligible midwives who have ceased private
practice because of retirement, disability, maternity leave, death or other
reasons, with 100% of costs covered by the Commonwealth.
|
Notes: (a) Further information on the PSS, including
eligibility criteria can be found at Department of Health (DoH), ‘ Premium
Support Scheme (PSS) – frequently asked questions’, DoH website, last
updated 1 March 2017;
(b) The Rural, Remote and Metropolitan Area (RRMA)
classification divides Australia into three zones and seven classes:
metropolitan zone (RRMA 1 and 2), rural zone (RRMA 3 to 5) and remote zone
(RRMA 6 and 7);
(c) Further information on the ROCS, including eligibility
criteria can be found at DoH, ‘Coverage
- doctors’, DoH website, last updated 4 April 2018;
(d) Further information
on the HCCS, can be found at Department of Human Services (DHS), ‘High
Cost Claim Indemnity Scheme’, DHS website, last updated 22 February 2019;
(e) Further information on the ECS, can be found at DoH, ‘Exceptional
Claims Scheme (ECS) – frequently asked questions’, DoH website, last
updated 31 January 2017;
(f) Further information on the IBNR Indemnity Scheme,
can be found at DHS, ‘Incurred
But Not Reported Indemnity Scheme’, DHS website, last updated 22 February
2019;
(g) Further information on the MIPS, can be found at DHS, ‘Midwife
Professional Indemnity Scheme’, DHS website, last updated 20 September
2019.
Source: DoH, ‘The
Indemnity Insurance Fund Schemes’, op. cit.; Australian National Audit
Office (ANAO), The
management, administration and monitoring of the Indemnity Insurance Fund, DoH
and DHS, Audit report, 20, 2016–17, ANAO, Barton, ACT, 2016, p. 17.
Midwife indemnity
insurance
Before
2009–10
Before 2010, there was no obligation for nurses or
midwives to have professional indemnity insurance as a condition of their
registration to practice. At this time, insurance arrangements for midwives
varied. Midwives employed with the public and private sectors were generally
indemnified under the employer’s insurance policies and, prior to 2001
privately practicing midwives were able to access indemnity insurance through
membership of industrial and professional organisations, such as the Australian
Nursing Federation. In 2000–01 professional indemnity insurance coverage was
withdrawn from privately practicing midwives. This was perceived to be in
response to the medical indemnity crisis of the late 1990s.[10]
As such, privately practicing midwives were unable to access indemnity
insurance as there were no insurers willing to offer suitable products for the
full range of maternity services.[11]
The lack of professional indemnity insurance for privately
practicing midwives was raised as a concern during a 2008 review into maternity
services, which found that the lack of insurance created a barrier to
implementing new models of maternity care. The report further noted that the planned
introduction of the health profession’s National Registration and Accreditation
Scheme in 2010 would pose problems for privately practicing midwives who could
not obtain the cover required for registration under state and territory laws.[12]
It recommended:
... while a risk profile for midwife professional indemnity
insurance premiums is being developed, consideration be given to Commonwealth
support to ensure that suitable professional indemnity insurance is available
for appropriately qualified and skilled midwives operating in collaborative
team-based models. Consideration would include both period and quantum of
funding.[13]
After
2009–10
In response to the review, the Government announced a
$120.5 million package of maternity measures in the 2009–10 Budget aimed at
giving access to Medicare Benefits Schedule and Pharmaceutical Benefits Scheme
benefits for services provided by eligible midwives and providing
government-supported professional indemnity insurance.[14]
The Government subsequently introduced and passed legislation which created a
framework for the Commonwealth’s involvement in an indemnity scheme for
midwives. Relevant legislation includes:
As noted previously, under an exemption in the National
Law, privately practicing midwives who provide intrapartum services (labour
and delivery) for women having homebirths are not required to hold professional
indemnity insurance, as there is currently no indemnity insurance product
available. This exemption applies until 31 December 2019.[15]
MIGA is currently the only provider of professional
indemnity insurance for privately practising midwives in Australia.[16]
Recent
reviews
In February 2014, the National Commission of Audit
recommended that the Commonwealth scale back its subsidies for medical
indemnity insurance. It reported that there was evidence that the market was
normalising, with premiums becoming more affordable and net assets and profits
for insurers increasing.[17]
At the time the Government announced that reforms to medical indemnity would be
considered following the 2014–15 Budget.[18]
Australian National
Audit Office
The Australian National Audit Office (ANAO) conducted a
performance audit of the IIF in 2016. The report made a number of
recommendations which were accepted by the Department of Health:
Recommendation No. 1: The Department of Health should conduct
a ‘first principles review’ of the Indemnity Insurance Fund and related schemes
prior to the 2017–18 Budget.
Health’s response: Agreed with qualification.
Recommendation No. 2: Subject to the outcome of this ‘first
principles review’, the Department of Health should develop and implement a
fit-for-purpose monitoring and reporting arrangement for the Indemnity
Insurance Fund, legislation, and related schemes that provides its Minister
with timely, robust analysis of the Indemnity Insurance Fund’s performance and
risks to government.
Health’s response: Agreed.
Recommendation No. 3: That the Department of Health establish
suitable governance and stakeholder engagement arrangements, including risk
management plans, to support its and other shared responsibilities for the
administration of the Indemnity Insurance Fund and related schemes.
Health’s response: Agreed.
Recommendation No. 4: That the departments of Health and
Human Services review their Indemnity Insurance Fund administrative
arrangements to:
(a) establish
a suitable set of public and internal key performance indicators that allow for
relevant, reliable and complete reporting of the Indemnity Insurance Fund
schemes’ performance;
(b) ensure
that public guidance materials are accurate, consistent and current;
(c) establish
suitable controls to improve data integrity, including monitoring and reporting
of any relevant matters under the bilateral programme agreement; and
(d) consult
with relevant insurers and the Australian Government Actuary to improve the
relevancy, consistency and accuracy of data used to inform projections of the
Commonwealth’s risks.
Health’s response: Agreed.
Human Services’ response: Agreed.[19]
First
Principles Review
In the 2016–17 Mid-Year Economic and Fiscal Outlook
(MYEFO) the Government announced that it would achieve savings of $35.9 million
over three years from 2017–18 by raising the eligibility threshold for claims
under the HCCS from $0.3 million to $0.5 million from 1 July 2018. At the same
time, the Government provided $0.2 million to conduct a review of the IIF and
associated schemes.[20]
Two reviews were conducted by the Department of Health:
-
the First Principles Review (FPR) of the IIF and
- a thematic review of the medical indemnity legislation.
The FPR of the IIF sought to answer three questions:
- To what degree has Commonwealth intervention been successful in
providing stability to the medical indemnity insurance industry, availability
of affordable indemnity insurance, and viability for professions, and patients,
particularly in relation to high cost claims?
- What is the appropriate level of Commonwealth support needed to
continue stability, affordability and accessibility of indemnity insurance for
medical practitioners and eligible midwives?
- Are the seven schemes that collectively comprise the IIF fit for
purpose or might improvements be made?[21]
The report made a number of recommendations aimed at
improving efficiency, targeting and transparency of the IIF. This Bill puts in
place the legislative framework to implement a number of these recommendations.
The complete list of recommendations can be found at Appendix A of this
Bills Digest.
Thematic
Review
The Thematic Review of Commonwealth Medical and Midwife
Indemnity Legislation examined 17 legislative instruments supporting the
IIF. The review focussed on identifying opportunities to:
- consolidate instruments wherever possible
-
remove redundant or inoperable legislation
-
ensure the instruments are consistent with the broader legal and
policy context and with the clearer laws principles and
- simplify the legislation wherever possible.[22]
A summary of the key findings of the review can be found
at Appendix B of this Bills Digest.
Committee consideration
Senate Selection
of Bill Committee
In its report on 17 October 2019, the Senate Selection of
Bills Committee recommended that the Bill not be referred to a committee for
inquiry.[23]
Senate
Standing Committee for the Scrutiny of Bills
In its report on 16 October 2019, the Senate Standing
Committee for the Scrutiny of Bills (the Committee) raised three concerns
relating to the Bill about which it requested further Ministerial advice.
Computerised
decision-making
The Committee noted:
Items 15 and 26 of Schedule 3 to the bill seek, respectively,
to insert sections 76A into the Medical Indemnity Act 2002 (Indemnity
Act) and section 87A into the Midwife Professional Indemnity (Commonwealth
Contribution) Scheme Act 2010 (MPI) Scheme Act) [that would allow the Chief
Executive Medicare] to arrange for the use of computer programs for any purpose
for which the CEM may or must take administrative action.[24]
The Committee questioned whether this was ‘necessary and
appropriate’ and whether consideration had been given to requiring that certain
administrative actions (for example, complex or discretionary decisions) be
taken by a person rather than by a computer.[25]
Reversal of
evidential burden of proof
The Committee noted:
Subsection 77(2) of the Indemnity Act and subsection 88(2) of
the MPI Scheme Act provide that a person commits an offence if they copy,
record, disclose or produce protected information or a protected document to
another person, where the first person is not performing or exercising duties,
powers or functions under specified legislation. The offence is punishable by
two years' imprisonment.
Items 18 and 29 of Schedule 3 to the bill seek, respectively,
to insert subsections 77(2A) and (2B) into the Indemnity Act, and subsections
88(2A) and (2B) into the MPI Scheme Act. The new provisions would provide that,
despite subsections 77(2) and 88(2), certain listed persons may copy, record,
or disclose protected information or a protected document, for the purposes of
monitoring, assessing or reviewing the operation of the medical indemnity
legislation. In this respect, they would create offence-specific defences to
the offences in subsections 77(2) and 88(2). The defences reverse the
evidential burden of proof.[26]
The Committee requested the Minister’s advice as to
whether the proposed reversal of the evidential burden of proof was necessary
and appropriate.[27]
Broad
delegation of legislative power
The Committee also noted that Schedule 6, item 26,
proposed paragraphs 34ZZG(2)(b) and 34ZZZD(2)(b), and proposed subsections
34ZZZF(1) and (2) allow regulations to modify and exempt matters from the
operation of the primary legislation and questioned whether it would be
appropriate to amend the Bill to insert high-level guidance concerning the
making of regulations:
Item 26 of Schedule 6 to the bill seeks to insert new
Divisions 2C and 2D into the Indemnity Act, to provide for the operation of the
allied health high cost claim indemnity scheme and the allied health exceptional
claims indemnity scheme.
Proposed paragraphs 34ZZG(2)(b) and 34ZZZD(2)(b) seek to
allow regulations to provide, respectively, that Divisions 2C and 2D apply,
with specified modifications, to certain liabilities associated with costs
which have been paid.
Additionally, proposed subsection 34ZZZF(1) seeks to allow
the regulations to provide that Division 2D applies, with specified
modifications, in relation to a specified class of claims, a specified class of
contracts of insurance, or a specified class of situations in which a liability
is wholly or partly covered by more than one contract of insurance. Proposed
subsection 34ZZZF(2) further seeks to allow the regulations to provide that
Division 2D does not apply, or applies with specified modifications, in
relation to a specified class of liabilities or payments.
Provisions enabling delegated legislation to modify the
operation of primary legislation are akin to Henry VIII clauses, which
authorise delegated legislation to make substantive amendments to primary
legislation (generally the parent Act). The committee has significant scrutiny
concerns with Henry VIII-type clauses, as such clauses impact parliamentary
oversight and may subvert the appropriate division of powers between the
Parliament and the executive. The committee will also have concerns about
provisions that enable delegated legislation to create exemptions from primary
legislation, as these provisions may have the effect of limiting, or in some
cases removing, parliamentary scrutiny.
In light of these matters, the committee expects a sound
justification in the explanatory materials for any provision that allows
delegated legislation to modify, or to exempt matters from, the operation of
primary legislation. The committee notes that, in this instance, no such
justification is provided in the explanatory memorandum.
The committee requests the minister's advice as to:
- why it is proposed to allow regulations to modify and exempt
matters from the operation of the primary legislation; and
- whether
it would be appropriate to amend the bill to insert at least high-level
guidance concerning the making of such regulations.[28]
At the time of writing the Ministerial response had been
received but not published.[29]
Policy
position of non-government parties/independents
Australian
Labor Party
The Australian Labor Party (Labor) is broadly supportive
of the Bill, but has raised concerns regarding two main issues: the continued
lack of insurance coverage options for private midwives providing intrapartum
services (labour and delivery) for women having homebirths and the continuation
of a single insurance provider for midwives, limiting individual choice.[30]
Independents
The Member for Indi, Dr Helen Haines MP, supports the Bill
but also considered that the inclusion of insurance options for private
midwives providing intrapartum services for homebirths would be beneficial.[31]
Position of
major interest groups
Australian
Medical Association
The Australian Medical Association (AMA) is strongly
supportive of the Bill, noting its continued advocacy in the space since 2002:[32]
The Medical and Midwife Indemnity Legislation
Amendment Bill 2019 will ensure the AMA’s hard-won medical indemnity
reforms of 2002 will continue to provide confidence for doctors, their patients,
and insurers.
...
The ability of doctors to continue to practise medicine
securely into the future has been strengthened.
The AMA played a critical role steering two indemnity reviews
over the past two years.
AMA President Dr Tony Bartone said bringing the reviews to
their conclusions was both challenging and rewarding.
“The AMA has fought hard to maintain the stability of our
medical indemnity system and preserve the underwriting from the Commonwealth,
which we achieved well over a decade ago,” Dr Bartone said.
“In 2016, there was a sudden and substantial cut to medical
indemnity schemes, followed by the announcement of the two reviews.
“Concerned about the Government’s ongoing commitment to these
schemes, the AMA advocated forcefully at each and every consultation, meeting,
roundtable, and re-draft of the schemes.
“On behalf of the entire profession, we have worked with
indemnity insurers, other peak groups, the Department of Health, the Minister’s
office, and the Australian Financial Complaints Authority, to name but a few.”
...
“This should ensure that the premium stability we have
enjoyed continues.”[33]
Financial
implications
The Explanatory Memorandum states that the legislative
changes have nil financial impact.[34]
Statement of Compatibility with Human Rights
As required under Part 3 of the Human Rights
(Parliamentary Scrutiny) Act 2011 (Cth), the Government has assessed
the Bill’s compatibility with the human rights and freedoms recognised or
declared in the international instruments listed in section 3 of that Act. The
Government considers that the Bill is compatible.[35]
Parliamentary
Joint Committee on Human Rights
At the time of writing, the Parliamentary Joint Committee
on Human Rights has not commented on the Bill.
Schedule
1—Competitive advantage payment and UMP support payment
Part 1 –
Repeals
Items 1 and 2 repeal the Competitive
Advantage Payment Act and the UMP Support Payment Act respectively.
Both Acts are being repealed as they are considered redundant.
The Competitive Advantage Payment Act provides for
an annual tax (competitive advantage payment) to be imposed on a MDO
participating in the Incurred But Not Reported (IBNR) Indemnity Scheme.[36]
The annual tax is imposed to neutralise any competitive advantage the MDO may
have due to its participation in the IBNR Indemnity Scheme.
Avant Mutual Group Limited (Avant) and its predecessor UMP
was the only MDO subject to the competitive advantage payment. According to the
Explanatory Memorandum, in 2006, the only MDO (UMP, now Avant) entered into a
deed of agreement with the Commonwealth, to pay a lump sum in order ‘to redress
the competitive advantage received by the insurer through participation in the
IBNR Indemnity Scheme’.[37]
The effect of this arrangement means that under section 25A of the Medical Indemnity
Regulations 2003, the MDO is exempt from having to make the annual
competitive advantage payment. This has therefore rendered the Competitive
Advantage Payment Act redundant.
The Explanatory Memorandum states:
The Medical Indemnity (UMP Support Payment) Regulations 2002
(established under the Medical Indemnity (UMP Support Payment) Act 2002)
declare that the financial year starting on 1 July 2006 is the last
contribution year for UMP (now Avant). As UMP support payment is no longer
payable, the legislation and regulations are redundant.[38]
Part 2 –
Amendments
Part 2 of Schedule 1 to the Bill amends a number of
statutes which are affected by the repeal of the two pieces of legislation in
Part 1 of Schedule 1 by, among other things, removing reference to the
Competitive Advantage Payment Act and the UMP Support Payment Act.
Amendments are also made as a consequence of changes to the run-off cover in Part
3 of Schedule 2 to the Bill which is discussed below. Other amendments include
changes to the objects of the MI Act, and also to the IBNR annual assessment
and reporting requirements, shifting from a contribution year to a financial
year.
Medical
Indemnity Act 2002
Items 8–52 in Part 2 of Schedule 1 to the Bill
amend the MI Act. Existing section 3 of the MI Act outlines the
objects of the Act.
Item 8 inserts a new subheading ‘Availability of
medical services’ in the Objects provision, just above subsection 3(1), which
refers to the object of contributing towards the availability of medical
services in Australia.
Existing subsection 3(4) states that an object of the MI
Act is to allow the Commonwealth:
- to recover the costs of providing the assistance referred to in
paragraph (2)(c)[39]
by requiring payments from persons who were members of relevant organisations
on 30 June 2000
- to recover the costs of providing the assistance referred to in paragraph
(2)(ab)[40]
by requiring payments from medical indemnity insurers and
-
to require a payment from medical indemnity insurers to ensure
that the assistance referred to in paragraph (2)(c) does not give a competitive
advantage to the organisations that receive that assistance.
Item 9 repeals and replaces subsection 3(4) to re-shape
the currently stated object to provide that it is ‘to allow the Commonwealth to
recover costs of providing the assistance referred to in paragraph (2)(ab) by
requiring payments from medical indemnity insurers’.
Item 21 in Part 2 of Schedule 1 to the Bill inserts
proposed Subdivision G—IBNR exposure into Division 1 of Part 2 of the MI
Act. Within new Subdivision G, proposed section 27C sets out the
process for annually reassessing IBNR exposure. The IBNR Indemnity Scheme funds
the IBNR liabilities of MDOs where they do not have enough reserves to cover
their liabilities. ‘IBNR is a type of reserve account used in the insurance
industry as the provision of funds for claims and/or events that have
transpired, but have not yet been reported to an insurance company.’[41]
An insurer knows neither how many of these losses have occurred, nor the
severity of each loss, thus the IBNR figure is an estimate which is tested
using actuarial and statistical techniques.[42]
Report by
the Actuary
Proposed subsection 27C(1) of the MI Act provides
that for each financial year, the Actuary[43]
must give the Minister for Health a written report that:
- states the Actuary’s assessment of the participating MDO’s IBNR
exposure as at the end of the financial year and
- sets out the reasons for the assessment.
In preparing the report, the Actuary must take into
account any information that the CEM gives the Actuary in relation to the
participating MDO, which has been given by the MDO for the purposes of
preparing the report for the Minister for Health.
Chief
Executive Medicare’s information gathering powers
Proposed subsection 27C(3) of the MI Act provides
that if the CEM believes on reasonable grounds that the participating MDO is
capable of giving information that is relevant to assessing the participating
MDO’s IBNR exposure as at the end of a financial year, the CEM may request the
participating MDO to give him, or her, the information. Without limiting the
type of information that may be requested, by way of example it may include financial
statements, and a report prepared by a suitably qualified actuary assessing the
participating MDO’s IBNR exposure as at the end of a financial year.[44]
Currently section 45 of the MI Act provides that a
failure to provide information under specified provisions gives rise to an
offence of strict liability.[45]
Item 27 of Part 2 of Schedule 1 to the Bill amends subsection 45(1) so
that the failure to comply with a request for information under proposed
subsection 27C(3) is an offence under the MI Act.[46]
Schedule
2—Indemnity scheme payments
Part 1 –
Aggregation of claims for high cost claim indemnity schemes
The provisions in Part 1 of Schedule 2 to the Bill amend
the MI Act.
The MI Act aims to contribute towards the
availability of medical services in Australia, by providing Commonwealth
assistance to support access by medical practitioners to affordable arrangements
that indemnify them for claims arising in relation to their practice of their
medical professions.[47]
It seeks to maintain the affordability of medical indemnity insurance premiums.
The Explanatory Memorandum states that amendments proposed
under this part are aimed at providing greater ‘clarity around the claiming
criteria under the High Cost Claim Scheme (HCCS) when claims [or a claim] have
more than one defendant’.[48]
The amendments will also apply to the new Allied Health High Costs Claim Scheme
(AHHCCS) (see Schedule 6).
Item 1 amends subsection 4(1) of the MI
Act to insert a reference to the definition of eligible related
claims.
Item 2 repeals and replaces section 8A to set out
the criteria for eligible related claims in relation to a high
cost claim indemnity or allied health high cost claim indemnity. A claim or
claims will be eligible related claims for the purposes of aggregation, where
the claim is against the same medical practitioner, in relation to the same
incident, or series of incidents, and either:
- all
the claims are part of the same class action or representative proceeding or
- the
incident, or series of incidents, occurred in connection with a pregnancy or
birth of a child or children (that is, in respect of a single birth event)[49]
and
-
the application is the only application for a high cost claim indemnity
or allied health high cost claim indemnity that has been made in relation to
any of the claims and
-
none of the claims are eligible related claims in relation to another
claim for which an application for a high cost claim indemnity or allied health
high cost claim indemnity has been made.
The Explanatory Memorandum states:
The policy intent is that the aggregation of claims can only
apply in respect of the same individual practitioner. A single high cost claim
threshold cannot be applied across multiple practitioners in relation to the
same event.[50]
Section 30 of the MI Act sets out the circumstances
in which high cost claim indemnity is payable.
Item 3 of Part 1 in Schedule 2 to the Bill repeals and
replaces subparagraphs 30(1)(d) to (f) which provide for a new payability rule.
In addition to the existing criteria for payment of a high
cost claim indemnity to a MDO or insurer, the amendment also requires that:
- the MDO or insurer is first notified of the incident, claim or
eligible related claim between 1 January 2003 and the date specified
in the rules as the termination date for the high cost claim indemnity scheme[51]
- the MDO or insurer has a qualifying payment in relation to the
claim, or qualifying payments in relation to the claim, or the claim and one or
more eligible related claims[52]
and
-
the amount of the qualifying payment, or the sum of the amounts
of the qualifying payments, exceeds what was the high cost claim threshold at
the earliest of the following times:
- when
the MDO or insurer was first notified of the incident
- when
the MDO or insurer was first notified of the claim or
- when
the MDO or insurer was first notified of an eligible related claim.[53]
Subsection 31(1) of the MI Act sets out the
circumstances in which aggregating amounts for eligible claims are paid or
payable by a MDO and insurer. Currently, the section applies if a MDO pays, or
is liable to pay, an amount in relation to a claim, and an insurer pays or is
liable to pay ‘an amount in relation to the same claim (the insurer
amount)’, and the other limbs of that section are satisfied. [Emphasis added]
Item 6 amends paragraph 31(1)(b) by removing the reference
to ‘an amount in relation to the same claim (the insurer amount)’. This
is substituted with a reference to ‘an amount (the insurer amount) in relation
to the same claim or an eligible related claim’. [Emphasis added]
Item 9 inserts proposed subparagraph
31(2)(a)(iii) into the MI Act which deems the MDO to have received
notification of the incident, claim or eligible related claim when the insurer
was first notified. The Explanatory Memorandum clarifies that if the MDO was
first notified (before the insurer), then that time will be the relevant time
of notification for the purposes of satisfying proposed paragraphs 30(1)(d)
and (f) in relation to payability and timing.[54]
Item 10 provides that the amendments made by this
Part of the Bill apply in relation to any application for an indemnity scheme
payment made on or after Schedule 2 commences (whether in relation to a claim
made before or after that commencement).
Part
2—Medical Professions
Medical Indemnity
Act 2002
Part 2 of Schedule 2 to the Bill makes amendments to the MI
Act which clarify the eligibility of medical practitioners, as distinct from
allied health professionals, in relation to the HCCS and the ECS.[55]
Items 12 to 15 make necessary amendments to
relevant provisions of the MI Act by removing reference to individuals
who fall under the rubric of allied health professionals. This is done to
clarify that the HCCS and ECS only have application in relation to medical
practitioners.
Item 16 contains an application provision
specifying that despite the amendments made under this Part, those sections
will continue to apply in respect of a claim if that claim relates to an
incident that occurred prior to 1 July 2020, or a series of incidents, at least
one of which occurred before 1 July 2020, in the course of or in connection
with, the practice by a practitioner of a medical profession (other than
practice as an eligible midwife or medical practitioner). Thus those who were
eligible for the HCCS and ECS prior to 1 July 2020 will continue to have their
claims assessed under the HCCS or ECS.
Part
3—Run-off cover on retirement
Run-off Cover is a niche class of insurance held within a
Professional Indemnity Insurance policy which provides liability cover for work
done by a person or business in the past, prior to adopting the run-off cover. This
type of cover is provided by an insurer when a particular person retires or
when a business is sold.[56]
The ROCS ‘is a scheme designed to provide secure insurance for doctors who have
left private practice’.[57]
Medical
practitioners
Currently, if a medical practitioner retires before the
age of 65, an insurer must offer them run-off cover on the same terms and
conditions as their last cover[58]
(other than terms as to price).[59]
After three years of not engaging in private medical practice, the practitioner
becomes eligible for ROCS and is no longer charged for run-off cover.
Thus, in the interim three year period, insurers can
charge a nominal amount for run-off cover offered to medical practitioners who
permanently retire from private medical practice under the age of 65.
Midwives
A parallel scheme with the same three year waiting period
applies to midwives who permanently retire from private practice before the age
of 65.[60]
Effect of
Amendments
The amendments proposed by this Part of the Bill will have
the effect that on expiry of the medical practitioner's or midwife’s insurance
contract, an insurer will not be able to charge a premium for the run-off cover
despite a medical practitioner or midwife retiring before the age of 65.[61]
The Bill amends the ROCS eligibility requirements to
provide that medical practitioners and midwives who have retired permanently
from private medical practice (regardless of their age) are eligible for the
ROCS, without requiring them to wait three years.
Subsection 39(1A) of the Age Discrimination Act provides
that anything done in direct compliance with a provision of an Act listed in
the table contained in Schedule 2 of the Age Discrimination Act is not
unlawful. This is because the statutes listed in that table are those for which
an exemption is provided by subsection 39(1A). Currently, items 6 and 7 of the
table are the MI(PS&PS) Act (Part 3) and the Medical Indemnity
(Prudential Supervision and Product Standards) Regulations 2003 (Part 3),
respectively.
Item 17 repeals table items 6 and 7 from Schedule 2
of the Age Discrimination Act, thus removing the age discrimination
exemption in relation to run-off cover for medical practitioners and midwives.
Medical
Indemnity Act 2002
Section 34ZB of the MI Act sets out the eligibility
criteria for run-off claims. One of the eligibility criteria in existing paragraph
34ZB(2)(a) is that the person against whom the claim is made is aged 65 years
or over and has retired permanently from private medical practice.
Item 19 amends paragraph 34ZB(2)(a) by removing the
‘aged 65 years or over’ requirement, and simply requiring that the person has retired
permanently from private medical practice regardless of age.
Item 20 contains transitional provisions specifying
that the amendments made to the Age Discrimination Act made by this Part
apply in relation to anything done after the commencement of subitem 20(1).
Subitem 20(2) provides that the amendments to subsection 34ZB(2) of the MI Act
made by this Part apply in relation to:
- any claim made after the commencement of this item against a
person who has retired permanently from private medical practice and
- any requirement under Division 2A of Part 3 of the MI(PS&PS)
Act to provide medical indemnity cover after the commencement of this item
for a person who has retired permanently from private medical practice
whether the person retired before or after the
commencement of this item.
However, if before item 20 commences:
- a person less than 65 years has permanently retired from medical
practice and
-
they have accepted an offer to provide medical indemnity cover
because of a particular event prescribed by the regulations, or they have
accepted an offer to renew because of those circumstances, and that cover has
not expired
that person cannot enjoy relief from premium for that
indemnity until that cover expires.
Midwife
Professional Indemnity (Commonwealth Contribution) Scheme Act 2010
Paragraph 31(2)(a) of the MPICCS Act sets out the
eligibility criteria for run-off claims. One of the eligibility criteria in existing
paragraph 31(2)(a) is that the person against whom the claim is made is aged 65
years or over and has retired permanently from private practice as an eligible
midwife.
Item 21 amends paragraph 31(2)(a) of the MPICCS
Act by removing the ‘aged 65 years or over’ criterion, and
simply requiring that the person has retired permanently from private practice as
an eligible midwife, regardless of age. This amendment enables them to access
the ROCS without paying a premium for the run-off cover.
Item 22 contains an application provision
specifying that midwives who have permanently retired from private practice
under the age of 65 before or after the commencement of item 21, will be
entitled to access the ROCS in relation to claims made after the commencement
of amendments in item 21.
Part
4—Health service incidents
Medical
Indemnity Act 2002
The proposed amendments in this Part are intended to
provide clarification about the purpose and scope of the IIF. The Explanatory
Memorandum states that ‘payments will only be made if the claim relates to the
provision of a health service (for example rather than a workplace or
occupier’s liability issue)’.[62]
Two amendments are made to the definitions subsection 4(1) of the MI Act
to ensure the payment of claims clearly align with this intent.
Item 23 inserts a definition of health
service into subsection 4(1) of the MI Act to more clearly
delimit it to its practical professional meaning. The proposed definition of
health service is ‘any service, care, treatment, advice or goods provided in
respect of the physical or mental health of a person’.
Item 24 repeals the existing definition of incident
in subsection 4(1) of the MI Act and substitutes it with a new
definition so that incident will mean ‘any incident (including
any act, omission or circumstance) that occurs, or that is claimed to have
occurred, in the course of, or in connection with, the provision of a health
service’.
Midwife
Professional Indemnity (Commonwealth Contribution) Scheme Act 2010
Amendments proposed to the definitions section of the MPICCS
Act by items 25 and 26, mirror the amendments
made by items 23 and 24 in this Part. Correspondingly, the intent of the
amendments is to ensure that ‘payments will only be made if the claim relates
to the provision of a health service (for example rather than a workplace or
occupier’s liability issue)’.[63]
Item 27 of Part 4 in Schedule 2 to the Bill contains
an application provision stating that the amendments made by this part apply in
relation to an incident that occurs or is claimed to have occurred after the
commencement of this Part.
Schedule
3—Administration
The Explanatory Memorandum states that the amendments
proposed in this Schedule ‘deal with administrative changes that streamline
and/or clarify the operation of the legislation’.[64]
The Explanatory Memorandum provides a good summary of the
key changes as follows:
- insert subsection headings to improve readability
- enable
the Chief Executive Medicare to treat an application as having been withdrawn
if further information requested is not provided by the date specified (items
4 and 11)
- streamline
the process for annual reporting on the ROCS to enable the Secretary to publish
the Actuary’s report on the Department of Health’s website (items 5-7
and 22-24)
- enable more efficient information
sharing between relevant agencies by specifying the circumstances in which it
will not be an offence to share protected information and documents where it is
for the purposes of monitoring, assessing or reviewing operation of the medical
indemnity legislation (items 18 and 29). Specifically, it will
not be an offence for the Secretary of the Department, the Chief Executive
Medicare, the Actuary, Australian Prudential Regulation Authority or Australian
Securities and Investments Commission to share information where it is for the
purposes of the medical indemnity legislation or the midwife professional
indemnity legislation, in particular to monitor and report to Parliament on the
effectiveness of Government financial support for the medical indemnity sector
- confirm
that the Chief Executive Medicare may use a computer program to make decisions
etc. under the Medical Indemnity Act 2002 and the Midwife
Professional Indemnity (Commonwealth Contribution) Scheme Act 2010 (items
15 and 26)
- confirm
the Secretary’s ability to delegate powers and functions under the Medical
Indemnity Act 2002 and the Midwife Professional Indemnity (Commonwealth
Contribution) Scheme Act 2010 to persons prescribed in those Acts (items
15 and 26).[65]
In 2016, the ANAO released its report on The
Management, Administration and Monitoring of the Indemnity Insurance Fund.[66]
In its report the ANAO made a number of observations and recommendations. Among
its findings was:
The Department of Health does not have fit-for-purpose
monitoring and reporting arrangements in place to assess the impact of the
measures—including regulatory and other legal reforms on the stability of the
indemnity insurance market, the affordability of premiums or importantly, the
government’s exposure to risk.[67]
In response to these findings, particular amendments are
proposed in Schedule 3 to the Bill which make provision for ‘an evaluation of
the affordability and stability of the medical indemnity market’.[68]
The Explanatory Memorandum states:
The intent of these provisions is to evaluate and report to
Parliament on the effectiveness of the Government’s support for medical
indemnity insurance and whether objectives are being achieved.[69]
Item 14 inserts at the end of Part 2 of the MI
Act, proposed Division 8—Monitoring. Under this Division, proposed
section 50 outlines the circumstances under which a medical indemnity
insurer may be required to provide information to the Secretary about any of
the following matters:
- premium costs of medical indemnity cover provided by contracts of
insurance with the insurer[70]
- the income of medical practitioners, or persons who practise an
allied health profession, for whom contracts of insurance with the insurer
provide medical indemnity cover[71]
- the profitability of the insurer[72]
- the insurer’s reinsurance arrangements and costs.[73]
Midwife
Professional Indemnity (Commonwealth Contribution) Scheme Act 2010
Item 25 inserts at the end of Part 4 of Chapter 2
of the MPICCS Act, proposed Division 9— Monitoring.
Under this Division, proposed section 71A outlines the
circumstances under which an eligible insurer may be required to provide
information to the Secretary about any of the following matters:
- premium costs for midwife professional indemnity cover provided
by contracts of insurance with the insurer[74]
- the income of eligible midwives for whom contracts of insurance
with the insurer provide midwife professional indemnity cover[75]
- the profitability of the insurer[76]
- the insurer’s reinsurance arrangements and costs.[77]
Schedule
4—Instruments
Part 1—Amendments
Medical
Indemnity Act 2002
The amendments in Part 1 of Schedule 4 to the Bill are
mainly ‘minor and machinery in nature’.[78]
For example, there are amendments to remove redundant references, but also to
insert new and necessary definitions.
Item 6 repeals the existing definition of participating
MDO and substitutes it with a new definition such that participating
MDO means UMP. This is to provide clarity that there is only one
participating MDO.[79]
As already mentioned, the thematic review of Commonwealth medical
and midwife indemnity legislation identified opportunities to, and recommended
the consolidation and streamlining of multiple instruments, simplifying the law
and ensuring the instruments are properly aligned with the broader legal and
policy context. The amendments in this Part of the Bill enable these changes to
occur, reducing ‘the number of separate legislative instruments used for the
purpose of regulating the Government’s support for medical indemnity’.[80]
Of note is that all matters prescribed under the powers in
the MI Act will be consolidated into one of two instruments: the Medical
Indemnity Rules or Medical Indemnity Regulations.
Minister’s
Rule Making power
Item 138 in Part 1 of Schedule 4 to the Bill inserts
proposed section 80 at the end of the Part 4 of the MI Act titled
‘rules’.
Proposed subsection 80(1) empowers the Minister to
make rules by legislative instrument prescribing matters:
- required or permitted by the MI Act to be prescribed by
the rules or
-
necessary or convenient to be prescribed for carrying out or
giving effect to the MI Act.
Proposed subsection 80(2) of the MI Act states
that these rules may not do any of the following:
- create an offence or civil penalty
- provide powers of arrest, detention, search or seizure
- impose taxes
- set an amount to be appropriated from the Consolidated Revenue
Fund under an appropriation in the MI Act
- directly amend the text of the Act.
Rules that are inconsistent with the regulations will have
no effect to the extent of the inconsistency. Rules are taken as being
consistent with the regulations, where they are capable of operating
concurrently with the regulations (proposed subsection 80(3)).
Records to
be retained for a certain period
Section 40 of the MI Act imposes particular record
keeping requirements on participating MDOs.
Item 122 repeals subsections 40(2) to (4),
replacing them with proposed subsections 40(2) to (3).
Proposed subsection 40(2) of the MI
Act states that records must be retained for a period of five years (or any
other period specified in the rules) starting on the day on which the records
were created. Failure to do so gives rise to an offence of strict liability under
section 47 of the Act.
Proposed section 40(3) provides that
rules made for the purposes of paragraph 40(1)(e)[81]
must not commence earlier than 14 days after the day on which the rules are
registered on the Federal Register of Legislation.
Requirements
for the terms of medical cover
Medical
Indemnity (Prudential Supervision and Product Standards) Act 2003
Section 26A of the MI(PS&PS) Act deals with the
provision of run-off cover to certain medical practitioners. Subsection 26A(4)
provides that this medical indemnity cover must meet the requirements of the
subsection. Existing paragraph 26A(4)(d) requires that the cover is provided on
such terms and conditions (if any) determined, by legislative instrument, by
the Minister administering the MI Act.
Item 141 repeals paragraph 26A(4)(d), substituting
it with a new paragraph 26A(4)(d) which states that medical indemnity cover
meets the requirements of the subsection if it is provided on the terms and
conditions on which the last medical indemnity cover provided for the
practitioner was provided, to the extent they are relevant to the provision of
medical indemnity cover.
Part
2—Application and Transitional
‘Part 2 of Schedule 4 specifies when the various changes
made by Part 1 of Schedule 4 to the Bill will take effect.’[82]
The Explanatory Memorandum provides a good high level explanation of these in
relation to the various proposed changes.[83]
Schedule
5—Universal cover
Medical
Indemnity Act 2002
Item 1 inserts a proposed subsection 3(3A)
into the ‘objects’ section of the MI Act adding:
The Act also supports access by medical practitioners to arrangements
that indemnify them for claims arising in relation to their practice of their
medical professions by limiting when medical indemnity insurers can refuse to
provide medical indemnity cover.
Item 2 inserts new key definitions for the
Australian Financial Complaints Authority (AFCA), Health Practitioner
Regulation National Law, private medical practice, professional indemnity
cover, and risk surcharge. The need for these definitions arises so as to
facilitate the integration of universal cover into the MI Act.
Private medical practice means practice
as a medical practitioner other than:
- practice consisting of treatment of public patients in a public
hospital
- practice for which the Commonwealth, a state or a territory, a
local governing body, or an authority established under a law of the
Commonwealth, a state or a territory, indemnifies medical practitioners from
liability relating to compensation claims
- practice conducted wholly outside both Australia and the external
Territories or
- practice of a kind specified in the rules.
A contract of insurance with a medical practitioner
provides professional indemnity cover if it provides medical
indemnity cover for the practitioner in relation to the practitioner’s private
medical practice.
Item 4 inserts proposed Part 2A—Universal cover
obligation comprising three new Divisions into the MI Act.
This Part imposes an obligation on medical indemnity
insurers to provide medical indemnity cover for medical practitioners in
relation to private medical practice (subject to limited exceptions). It
specifies the circumstances in which a medical indemnity insurer may require a
medical practitioner to pay a risk surcharge, and it imposes record keeping
requirements on medical indemnity insurers in relation to the obligation to
provide universal medical indemnity cover.
Within new Part 2A, proposed section 52 states that
a medical indemnity insurer is not required to comply with Division 2 (Requirements
in relation to providing professional indemnity cover) other than for the
purposes of the AFCA scheme.[84]
The Explanatory Memorandum states:
Universal cover obligations will be managed under existing
AFCA arrangements whereby a practitioner can make a complaint to AFCA about a
potential breach of this Division.[85]
Universal
cover obligation
Proposed section 52A provides that a medical indemnity
insurer must not refuse to enter into a contract of insurance with a medical
practitioner to provide professional indemnity cover unless one of the
following circumstances applies:
-
in relation to a medical professional indemnity insurance
contract between the practitioner and the insurer, the practitioner:
- failed
to comply with the duty of the utmost good faith or the duty of disclosure
(within the meaning of the Insurance Contracts
Act 1984)
- made
a misrepresentation to the insurer during the negotiations for the contract but
before it was entered into
- failed
to comply with a provision of the contract, including a provision with respect
to payment of the premium or
- made
a fraudulent claim under the contract
-
the practitioner places the public at risk of substantial harm in
the practitioner’s private medical practice because the practitioner has an
impairment (within the meaning of the Health
Practitioner Regulation National Law)
- the practitioner poses an unreasonable risk of harm to members of
the insurer’s staff because of persistent threatening or abusive behaviour
towards members of the insurer’s staff
-
the practitioner has persistently failed to comply with
reasonable risk management requirements of the insurer or
- additional circumstances in which cover may be refused may also
be specified in the rules. [86]
These rules made will be a legislative instrument, and
thus subject to Parliamentary scrutiny.
Medical
indemnity insurer to notify of refusal to indemnify
Proposed section 52B requires a medical indemnity
insurer to notify a medical practitioner in writing in relation to a decision
to refuse to enter into a contract for insurance. This notice in writing must
comply with any requirement specified in the rules.
Risk
surcharge requirements
Proposed subsection 52C(1) of the MI Act enables
a medical indemnity insurer to require that a medical practitioner, pays a risk
surcharge as part of the amount payable for professional indemnity
cover provided by a contract of insurance with the practitioner. This risk
surcharge is to reflect the fact that if the practitioner engages, or has
engaged, in conduct that deviates from good medical practice, the
practitioner’s private medical practice is likely to pose a higher risk to
patients than similar practices.[87]
Additional circumstances for the imposition of this surcharge are to be
specified in the rules.[88]
The imposition of the risk surcharge is subject to
parameters contained in proposed subsections 52C(2) and 52C(3). Proposed
subsection 52C(2) provides that the private medical practice of another
medical practitioner (the comparison practitioner) is a similar
practice if the insurer reasonably considers that the practitioner and the
comparison practitioner have similar practice profiles for the purposes of calculating
premiums for professional indemnity cover, except that the comparison
practitioner does not engage, and has not engaged, in conduct that deviates
from good medical practice. Proposed subsection 52C(3) states the risk
surcharge must not exceed the amount articulated in the rules.
Proposed subsection 52D(1) of the MI Act
provides that an indemnity insurer may be required to offer interim cover to a
medical practitioner until complaint to AFCA is finalised, where that
complaint relates to a refusal by the insurer to enter into a subsequent contract
of insurance with a practitioner who has an existing contract for professional
indemnity cover with that insurer.
Proposed subsection 52D(4) specifies that a
complaint is finalised when any of the following circumstances are
applied:
-
the complaint is resolved by agreement between the insurer and
the practitioner
- the complaint is withdrawn
- AFCA closes the complaint or
- the complaint otherwise ceases to be dealt with by AFCA.
Proposed subsection 52D(2) of the MI Act provides
that the interim offer must comply with any requirements specified in the rules.
Records,
reporting and information
New Division 3—records, reporting and information
sets out record keeping requirements and the consequences of a failure to keep
records as required. It also imposes annual reporting requirements on the medical
indemnity insurer in relation to specific matters, and it empowers the
Secretary of the Department of Health (the Secretary) to request particular
information, and imposes a penalty for a failure to comply with such a request.
Proposed subsection 53(1) provides that the rules
may require a medical indemnity insurer to keep records relating to the
following:
-
a refusal to enter into a contract or insurance with a medical
practitioner to provide professional indemnity cover
- a requirement by the insurer that a medical practitioner pay a
risk surcharge.
The subsection contains a note stating that a failure to retain
the records is an offence under proposed section 53A.The offence is an
offence of strict liability.[89]
Medical
indemnity insurer must report annually
Proposed subsection 53B(1) of the MI Act provides
that if, in a financial year, a medical indemnity insurer refuses to enter into
a contract of insurance with a medical practitioner to provide professional
indemnity cover, the insurer must notify the Secretary within two months after
the end of the financial year of:
-
the number of times in the financial year the insurer refused to
enter into a contract of insurance with a medical practitioner to provide
professional indemnity cover and
- any other matter that relates to the insurer’s obligations under
Division 2 of new Part 2A and that is specified in the rules.
The subsection contains a note stating that a failure to notify
the Secretary is an offence under proposed section 53C. The offence is
an offence of strict liability.[90]
Secretary
may request information
Proposed subsection 53D(1) provides that the
Secretary may request a medical indemnity insurer to give the Secretary the
following information, in the form requested by the Secretary:
- the number of times in a period the insurer refused to enter into
a contract of insurance with a medical practitioner to provide professional
indemnity cover
- the number of times in a period the insurer required a medical
practitioner to pay a risk surcharge
- other information that relates to the insurer’s obligations under
Division 2 of new Part 2A and that is specified in the rules.
Proposed subsection 53D(2) sets out the manner and
form requirements in relation to the Secretary’s request for information:
- must be made in writing
- may require the information to be verified by statutory
declaration
- must specify the day on or before which the information must be
given (at least 28 days after the day on which the request is made)
- must contain a statement to the effect that a failure to comply with
the request is an offence.
Schedule
6—Allied health professionals
The Explanatory Memorandum states:
In the 2018-19 MYEFO, the Government decided to continue to
provide support for insurers currently providing professional indemnity
insurance to registered privately practising allied health professionals, and
that these schemes would be independent to schemes available to medical
practitioners.[91]
The provisions in Schedule 6 establish high cost claim and
exceptional claims schemes in new Divisions of Part 2 of the MI Act
specifically tailored for access by allied health professionals (rather than
medical practitioners). The makeup of these schemes significantly reflects ‘the
provisions in the existing HCCS and ECS as they apply to medical practitioners’.[92]
The Explanatory Memorandum further states:
It is Government’s intent that the new allied health schemes
will initially only be accessed by those medical indemnity insurers that are
currently providing medical indemnity cover for both medical practitioners and
for persons who practise an allied health profession. The rules are therefore
intended to prescribe those medical indemnity insurers that currently access
the HCCS.[93]
Medical
Indemnity Act 2002
Item 1 inserts at the end section 3 (the Objects
provision in the MI Act), another objective of the Act, which is:
... to contribute towards the availability of certain health
services in Australia by providing Commonwealth assistance to support access by
persons who practise allied health professions to arrangements that indemnify
them for claims arising in relation to their practices.[94]
Proposed subsection 3(6) of the MI Act states
that the Commonwealth provides that assistance under the MI Act by:
a) meeting
part of the costs of large settlements or awards paid by organisations that
indemnify persons who practise allied health professions and
b) meeting
the amounts by which settlements and awards exceed insurance contract limits,
if those contract limits meet the Commonwealth’s threshold requirements.
Item 2 inserts new definitions relevant to the new
schemes in subsection 4(1) of the MI Act. For example, allied health
exceptional claims indemnity, allied health high cost claim indemnity, allied
health high cost claim threshold, and allied health profession. The inclusion
of these new definitions is necessary in order to integrate the AHHCCS and the allied
health exceptional claims scheme (AHECS) into the medical indemnity legislation.
Allied
health high cost claim indemnity scheme
Item 26 inserts Division 2C—Allied health high
cost claim indemnity scheme into Part 2 of the MI Act.
Within new Division 2C, proposed subsection 34ZY(1)
sets out a Guide to the Allied Health high Cost Claim Indemnity provisions.
Proposed subsection 34ZY(1) states that Division 2C
provides that an allied health high cost claim indemnity may be paid to an
eligible MDO or eligible insurer that pays, or is liable to pay, more than a particular
amount (referred to as the allied health high cost claim threshold[95])
in relation to a claim against a person in relation to an incident that occurs
in the course of, or in connection with, the practice by the person of an
allied health profession.
Proposed subsection 34ZY(2) provides for the making
of regulations and rules to deal with other matters or incidents relating to
incidents covered by the allied health high cost claim indemnity scheme.
Proposed subsection 34ZY(3) of the MI Act provides
a useful table (see below) in relation to where to find the provisions on various
key issues in relation to the scheme, eligibility of MDOs and insurers, claim
threshold, the amount of the AHHCC indemnity etc.
Guide to
the allied health high cost claim indemnity provisions
| Where to find
the provisions on various issues
|
| Item |
Issue |
Provisions |
| 1 |
which
MDOs and insurers are eligible? |
section
34ZZ |
| 2 |
what
is the allied health high costclaim
threshold?
|
section
34ZZA |
| 3 |
what conditions must be satisfied for
an MDO or insurer to get the alliedhealth high cost claim indemnity?
|
sections 34ZZB to 34ZZD |
| 4 |
what happens if the incidents occurred
during treatment of a publicpatient in a public hospital?
|
paragraph 34ZZD(a) and section 34ZZE |
| 5 |
how
much is the allied health highcost claim indemnity?
|
section
34ZZF |
| 6 |
what
regulations can deal with |
section
34ZZG |
| 7 |
how do MDOs and insurers apply for the
allied health high cost claimindemnity?
|
section
36 |
| 8 |
when
will the allied health high costclaim indemnity be paid?
|
section
37 |
| 9 |
what information has to be provided to
the Chief Executive Medicare about allied health high costindemnity
matters?
|
section
38 |
| 10 |
what
records must MDOs andinsurers
keep?
|
section
39 |
| 11 |
how
are overpayments of allied health high cost claim indemnity recovered? |
sections
41 and 42 |
According to the Minister for Health, Greg Hunt, ‘the
allied health schemes will mirror the existing high cost claims and exceptional
claims schemes’.[96]
Appendix A: Recommendations
from the First Principles Review (FPR) of
the Indemnity Insurance Fund (IIF)
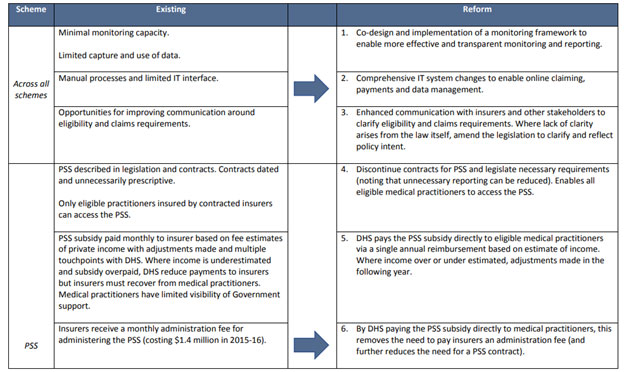
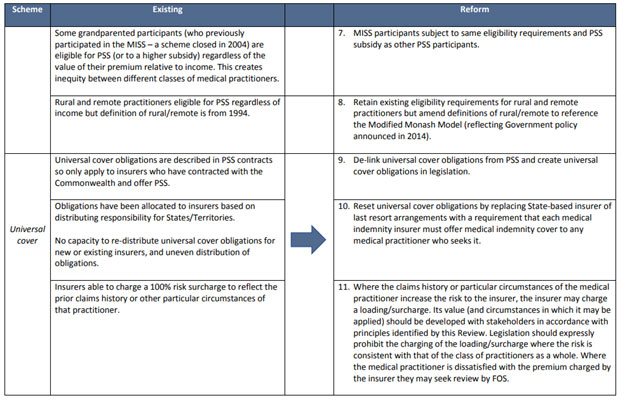
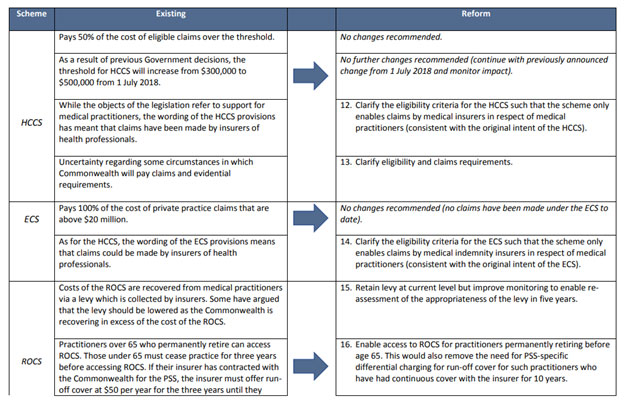
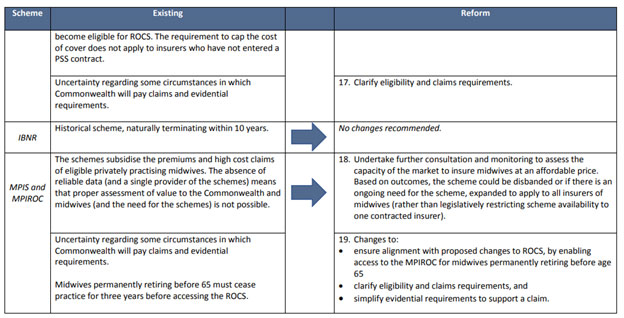
Source: MP Consulting, First
principles review of the Medical Indemnity Insurance Fund, report
prepared for the DoH, April 2018, pp. 53– 56.
Appendix B: Recommendations from the Thematic Review of Commonwealth
Medical and Midwife Indemnity Legislation
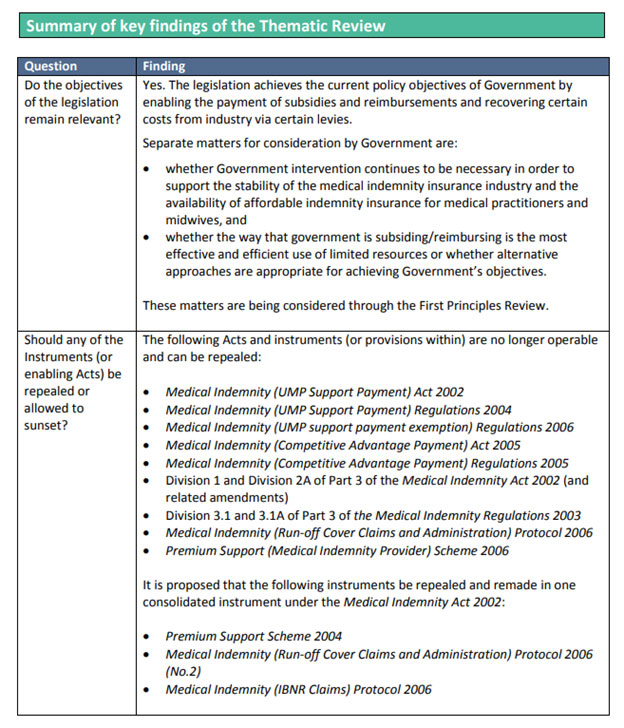
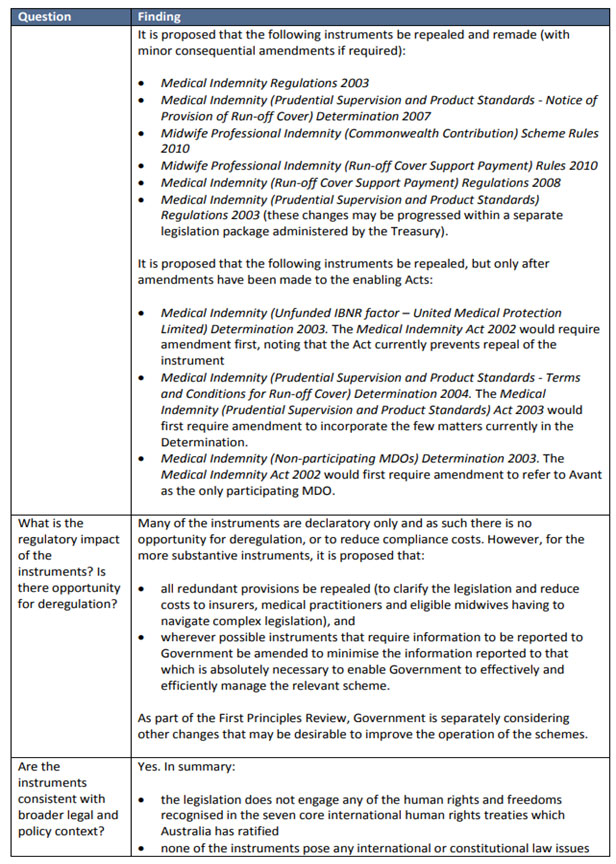
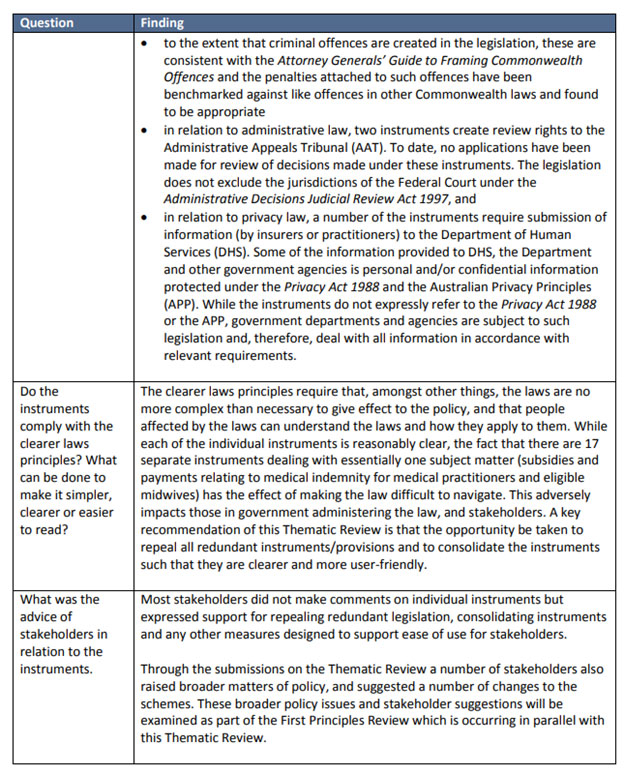
Source: MP Consulting, Thematic
review of Commonwealth medical and midwife indemnity legislation,
report prepared for the DoH, February 2018, pp. 5–7.