Key points
- The Bill proposes amendments to the Aged Care Act 1997 to:
- require residential aged care and some flexible care approved providers to always have a registered nurse on site and on duty, starting from 1 July 2023
- enable the Government to limit prices associated with home care packages and remove the approved provider’s ability to charge an exit amount and
- require the publication of information about aged care services.
- These amendments respond to Recommendations 86 and 88 of the Final Report of the Royal Commission into Aged Care Quality and Safety and implement election commitments of the new Labor Government.
- Questions exist as to the number of registered nurses who will need to be recruited to work in aged care facilities to meet the new requirements.
- The proposals will impose a regulatory burden on aged care providers.
Introductory Info
Date introduced: 27
July 2022
House: House of
Representatives
Portfolio: Health
and Aged Care
Commencement:
Sections 1–3: Royal Assent
Schedule 1: 1 April 2023
Schedule 2: 1 January 2023
Schedule 3: 1 December 2022
The Bills Digest at a glance
The Final
Report of the Royal Commission into Aged Care Quality and Safety (Royal
Commission) was publicly released 1 March 2021 by the Morrison Government.[1] The Final
Report recommended a fundamental and systemic shift in aged care and
provided 148 recommendations outlining the Commissioners’ vision for the future
of aged care. To implement some of these recommendations, legislative change is
required.
Since the release of the Final Report 4 pieces of
legislation have been introduced into the Parliament:
The Bill is designed to partially respond to 2 of the
Royal Commission’s recommendations:
- Recommendation
86: Minimum staff time standard for residential aged care
- Recommendation
88: Legislative amendments to improve provider governance.[2]
In addition, it is also designed to meet several of the
Australian Labor Party’s aged care election commitments.[3]
To achieve this, the Bill contains 3 schedules that will
amend the Aged
Care Act 1997 and enable additional requirements to be introduced in
delegated legislation:
- Schedule
1 – Registered Nurses
- this
Schedule will introduce a requirement for residential aged care and some
flexible care approved providers to have at least 1 registered nurse on site,
and on duty, at all times at the facility from 1 July 2023, unless the approved
provider has been granted an exemption in accordance with the Quality of Care
Principles 2014.
- Schedule
2 – Capping home care charges
- this
Schedule will introduce a power enabling the Government to limit (cap) the fees
that approved providers can apply to home care package recipients and remove
the ability of approved providers to charge the care recipient an exit amount.
- Schedule
3 – Transparency of Information
- this
Schedule will require the Secretary to make information on aged care services
publicly available, in accordance with the Information Principles 2014.
Purpose of
the Bill
The purpose of the Aged
Care Amendment (Implementing Care Reform) Bill 2022 (the Bill) is to amend
the Aged Care
Act 1997 (the Act) to:
- require
residential aged care and some flexible care approved providers to always have
a registered nurse on site and on duty (Schedule 1)
- enable
the Government to limit prices associated with home care packages and remove
the approved provider’s ability to charge an exit amount (Schedule 2)
- require
the Secretary to publish information about aged care services (Schedule 3).
Background
Schedule 1–Registered
nurses in aged care homes
The Centre for Health Services Development was requested
by the Royal Commission to undertake research into international and national
staffing portfolios for residential aged care to better understand how staffing
can be improved in Australia.
The Centre for Health Services Development observed that
there was limited evidence on the relationship between staffing and quality in
residential aged care (unlike in hospitals), and stated that the
‘methodological, definitional and cultural challenges within aged care have
limited its capacity to routinely measure quality’, as ‘the measures of quality
to date have primarily focused on relationships between inputs (dollars, staff
numbers) and outputs (client numbers, incident rates) rather than client
outcomes (quality of care)’.[4]
Using a nursing home quality rating system from the United States, the CMS 5
star system, which assigns a rating based on mandatory staffing levels and
minutes per resident, the authors found that 57.6% of people living in
Australian residential aged care homes received care in services that rated 2
stars or less. In other words, more than half of people living in residential
aged care in this study received less than 215 minutes care minutes and/or less
than 30 minutes with a registered nurse (RN) per day.[5]
In response to these findings, the Royal Commission stated
that ‘this is entirely unacceptable and partly explains the extent of
substandard care’ and made Recommendation 86, which is made up of 8 parts and
focuses on:
- introducing
a requirement for residential facilities to meet a quality and safety standard
on minimum staff time
- from
1 July 2022, the minimum staff standard should be at least 200 minutes of staff
time per day for the average resident, with at least 40 minutes being provided
by a RN
- this
standard should require, at a minimum, a RN to be on site for the morning and
afternoon shifts (16 hours per day)
- from
1 July 2024, the minimum staff time should increase to 215 minutes per resident
per day, with a minimum of 44 minutes being provided by a RN
- from
this date, a RN should always be required to be on site
- the
minimum staff time standard should be linked to the casemix-adjusted activity
based funding model
- some
exemptions to the staff skills mix requirement should be available by
application.[6]
Broader
financial considerations
StewartBrown, a chartered accountancy firm, undertakes
quarterly aged care
financial performance surveys with aged care services. In the most recent,
publicly available, report for the 9 months to March 2022, the authors state:
The Survey for the 9 month period ending March 2022 continues
to highlight the declining financial sustainability of the sector, with
residential aged care now being at a critical financial sustainability position.
The average operating results for residential aged care homes
in all geographic sectors was an operating loss of $12.85 per bed per day (March
2021 $6.10 pbd loss) despite the additional Basic Daily Fee supplement of
$10 per bed day…
It is the opinion of StewartBrown that after 5 years of
significant aggregate operating losses in the residential aged care sector,
that structural funding reforms (including care recipient co-contribution) are
essential. However, to avoid closure of homes and reduced service delivery,
especially in regional locations, an emergency funding package needs to be
delivered in the short term to ensure current viability and allow for the
necessary funding reforms to be properly implemented.[7] [emphasis in original]
The report provides a summary of the income and
expenditure for residential care, including the average expenditure on direct
care wages, which was $163.48 per bed day (85% of direct care revenue).[8]
The report goes on to state that services provide an average of 179 direct care
minutes per resident day.[9]
The EBITDAR (Earnings Before Interest, Taxation,
Depreciation, Amortisation and Rent) averaged at $2,679 per bed per annum (this
includes the $10
basic daily fee supplement) and is a decrease from March 2021, which was
$4,733.[10]
Nationally 38% of residential facilities are making an EBITDAR loss.[11]
Researchers from the University of Technology Sydney
undertook work analysing the results of the first 6 months of the 2020–21
financial year using the StewartBrown data, providing commentary on the
financial position and the major challenges for the aged care sector. In their
discussion on the implementation of the Australian
National Aged Care Classification (AN-ACC) funding model into residential
aged care,[12]
the researchers stated that that the impacts of the announced increase in funding
‘may not be as significant as the level of increase suggests’, as:
It is expected that the funding uplift will be largely
consumed by increases in total direct care staffing minutes to meet the minimum
staffing standards in force by October 2023. In the intervening period, the
sector will need to increase total direct care by an average of 22 minutes per
resident per day (approximately 12.4%) and RN minutes by 11.8 minutes (41.8%).
The AN-ACC amount already includes the $10 uplift in the
Basic Daily Fee announced as part of the 2021–22 Budget, which will need to be
allocated against everyday living costs to help reduce the losses on that
activity.
In the coming 18 months, providers potentially face further
increases in staffing costs if award rates are raised as a result of the Fair
Work Commission case and if new requirements to have an RN on-site 24/7 are
introduced. That is, these two factors have not been incorporated into the
initial AN-ACC price and would have to be funded separately if implemented.[13]
In a recent journal article that considered the
anticipated minimum staffing standards for introduction into residential aged
care (as committed to under the Morrison Government), the researchers
identified several policy considerations that should be factored into the
implementation of minimum staffing standards, drawing on international
evidence:
- the
cost associated with complying with new staffing standards
- the
possibility of input substitution where the regulation of one type of staff may
be offset by reducing the number of another type of staff, which can have a
negative impact on the quality of care and on the workload of the regulated
staff
- the
adequacy of the local labour market to meet the staffing requirements.[14]
Schedule 2–Home
care package costs (care and package management)
The Home
Care Package program aims to support older people with complex care needs
to live independently in their home.
In February 2017, the Government introduced stage 1 of the
Increasing
Choice in Home Care reforms, which, among other things, resulted in home
care packages being allocated to the consumer (rather than the home care
provider).[15]
With the shift away from home care packages being
allocated to the provider, the Department of Health released guidelines for
exit amounts:
An exit amount is a charge that a provider can deduct from a
client’s unspent home care package funds if the client leaves their care
(either because the client decides to change to another home care provider, or
the client leaves home care). The exit amount is intended to allow providers to
recover administrative costs associated with determining and making payment of
unspent home care amounts.[16]
An approved provider is required to enter into a home
care agreement with the person who will receive care (or their
representative) before they can provide services to that person. The agreement
sets out the services the organisation will provide (or organise to be
provided) and how much it will cost, including the exit amount. The
requirements of the agreement are outlined in the Act and the User Rights Principles
2014.[17]
Alongside the home care agreement, the approved provider also needs to provide
a care
plan and an individualised
budget.
Administration
costs
In 2019, the Government mandated pricing
transparency for home care package costs and charges with all approved providers
required to publish information on common services and costs using a
standardised format on the My Aged Care Service
Finder and also provide a copy of their pricing schedule to potential
consumers, with costs also being required to be outlined in the home care
agreement.
The Department provides information on the price
transparency requirements for home care packages, including administration
fees charged by the provider:
- Care
management (or case management), is a component of every home care package,
with the cost of care management services to be included in the pricing
schedule. Care management may include services such as:
- reviewing
the Home Care Agreement and care plan
- ensuring
care is culturally appropriate
- ensuring
the care is aligned with other supports.
- Package
management is a fortnightly cost to cover the ongoing organisational
activities associated with the delivery and management of the home care
package. It does not include business associated costs (e.g. marketing, office
rent). Business associated costs need to be included in the unit price for
specific care services rather than being a separate cost, and ‘must be
reasonable’.[18]
Table 1 provides a sector wide overview of home care
provider income per care recipient per day and indicates that in 2019-20,
management and administration fees formed almost 30 per cent of provider income
per care recipient.
Table 1 Home care provider income per consumer per day, 2017–18 to 2019–20

Source: Aged Care Financing Authority (ACFA), Ninth Report on
the Funding and Financing of the Aged Care Sector, (Canberra: DoH,
2021), 47.
In 2021, the Department started releasing national
summaries of home care prices. The national median price for select fees are
summarised in Table 2 from 31 December 2021, the most recent report. In
addition, the report indicates that 41% of services publish an exit amount of
more than $0 with the median exit amount for these services being $400.[19]
Table 2 National
summary of select home care package prices (31 December 2021)
| Pricing types and package level |
National median prices |
| Care management (cost per fortnight): fully managed by provider |
| Level 1 |
$58 |
| Level 2 |
$103 |
| Level 3 |
$212 |
| Level 4 |
$310 |
| Care management
(cost per fortnight): self-managed |
| Level 1 |
$37 |
| Level 2 |
$52 |
| Level 3 |
$95 |
| Level 4 |
$125 |
| Package
management (cost per fortnight) |
| Level 1 |
$35 |
| Level 2 |
$61 |
| Level 3 |
$133 |
| Level 4 |
$199 |
Source: Department of Health (DoH), National
Summary of Home Care Package Prices – 31 December 2021, (Canberra: DoH,
2022).
Concerns were raised to the Royal Commission about the
(in)adequacy of funding through the home care package program, including ‘that
a considerable portion of an older person’s Home Care Package allocation often
goes to care management and administration fees, rather than its intended
purpose of direct care’.[20]
Schedule 3–Information
available to the Department
Approved providers have responsibilities under the Act and
the Aged Care
Quality and Safety Commission Act 2018 to submit different types of
information to the Department and the Aged Care Quality and Safety Commission.
Some of these reporting requirements are briefly outlined below.
In addition, the Aged
Care and Other Legislation Amendment (Royal Commission Response) Bill 2022,
which recently passed the Parliament, will make changes to the governance of
approved providers (under Schedule 5), including changes to the key personnel
requirements and a new obligation for an approved provider to prepare an annual
statement that meets the requirements to be outlined in the Accountability
Principles 2014 and provide a copy to the Secretary of the Department.[21]
The Explanatory Memorandum provides a list of proposed
items for inclusion in the annual statement, which include:
- details
of key personnel
- information
on staffing
- financial
information
- complaints.[22]
In addition, an Information Technology solution is being developed
to, where practicable, prevent duplication where information is reported
elsewhere.[23]
Financial
reporting
As part of their obligations, approved providers are
required submit an Aged
Care Financial Report to the Department of Health and Aged Care at the end
of each financial year, with the specific requirements dependent on the type of
service provided. As outlined by the Department, residential aged care
providers are required to supply:
- information
on income and expenses for care services and other activities for each
facility, including information on labour costs and hours
- an
approved provider level balance sheet, income statement and cash flow statement
(non-government providers only)
- movement
schedules to accompany the financial statements
- a
consolidated parent level segment report covering all residential services
(non-government providers only)
- an
Annual Prudential Compliance Statement.[24]
As of the 1 July 2022, approved providers are also
required to submit quarterly
financial reports to the Department. As part of these reports, providers
will be required to report the care staffing minutes provided by RNs, enrolled
nurses and personal care workers.[25]
Reporting
on key personnel
Key personnel is defined under section 8B of
the Aged Care
Quality and Safety Commission Act 2018 and generally refers to:
- a
person who is responsible for the executive decisions of the organisation (this
will include members and directors of boards)
- a
person who has authority or responsibility for, or significant influence over,
planning, directing or controlling the activities of the organisation
- a
person who is responsible for the nursing services provided by the organisation
(if they hold a nursing qualification)
- a
person that is responsible for the day-to-day operations of an organisation.
As part of the 2016 deregulation reforms, the key
personnel requirements were scaled back and the Department advised that key
personnel did not generally need to be reported. However, this was later
modified and in late 2019 the Department of Health advised providers they would
need to notify the Secretary of any changes to key personnel that could
materially affect the provider’s suitability to provide aged care.[26]
Royal
Commission recommendation
The Royal Commission stated that the governance
requirements in the aged care legislation were insufficient for the governance
and leadership of aged care providers. As part of the changes, it recommended
to enhance the governance of the aged care system, the Royal Commission made
Recommendation 88 (see Figure 1), which Schedule 3 of this Bill is
designed to partially respond to.
Figure 1 Royal Commission’s Recommendation 88

Source: Royal Commission into Aged Care
Quality and Safety (Royal Commission), Final
Report: Care, Dignity and Respect, Volume 3B: The New System, (Adelaide:
Royal Commission, 2021), 456.
Committee consideration
Senate Community Affairs
Legislation Committee
The Bill has been referred to the Senate Community Affairs
Legislation Committee for inquiry and report by 31 August 2022. Details of the
inquiry are available on the inquiry
homepage.
Position of
major interest groups
The interim CEO of Aged & Community Care Providers
Association, Paul Sadler, has said the Association supports the Bill
in-principle and looks forward to having the opportunity to scrutinise the
implementation of the measures. One of the Association’s concerns is how the
changes to home care charges will impact both consumers and service providers.[27]
Statement of Compatibility with Human Rights
As required under Part 3 of the Human Rights
(Parliamentary Scrutiny) Act 2011 (Cth), the Government has assessed the
Bill’s compatibility with the human rights and freedoms recognised or declared
in the international instruments listed in section 3 of that Act.
The Government considers that the Bill is compatible with
human rights, noting that ‘the extent that the Bill may limit human rights…is
reasonable, necessary and proportionate to protect the rights of older
Australians’.[28]
Parliamentary
Joint Committee on Human Rights
The Committee had not reported on the Bill at the time of
writing.
Key issues
and provisions
To achieve the proposed changes for all 3 schedules, the
Bill will amend the Aged
Care Act 1997.
Schedule
1–Registered nurses
Current
staffing requirements
The Act requires aged care providers ‘to maintain an
adequate number of appropriately skilled staff to ensure that the care needs of
care recipients are met’.[29]
The Aged Care Quality
Standards, which approved
providers must comply with, require the approved provider to have ‘a
workforce that is sufficient, and is skilled and qualified, to provide safe,
respectful and quality care and services’, but the Standards do not prescribe
the qualifications needed nor the number of staff required.[30]
The Aged
Care and Other Legislation Amendment (Royal Commission Response) Bill 2022,
which recently passed the Parliament, changes governance arrangements for
approved providers (see Schedule 5), including a new responsibility for the
approved provider to require the governing body to ensure the provider’s staff:
- have
appropriate qualifications, skills or experience to provide the care and/or
services offered by the provider and
- are
given the opportunity to develop their capability to provide care and services.[31]
New
responsibility relating to registered nurses
Section 54-1 of the Act outlines the responsibilities of
approved providers in relation to the quality of aged care that must be provided
and includes requirements such as complying with the Aged Care Quality
Standards (paragraph 54-1(1)(d)). Item 1 of Schedule 1 inserts proposed
paragraph 54-1(1)(ba), which provides that if a provider meets the
criteria set out in proposed section 54-1A then they must comply with
the requirements in proposed subsection 54-1A(2).
Item 2 inserts proposed section 54-1A, which
outlines a new responsibility for some approved providers in relation to RNs.
Proposed subsection 54-1A(2) will require certain
approved providers from 1 July 2023, to ensure at least one RN is on site, and
on duty, at all times at a residential facility. This subsection draws on the
definition of ‘registered nurse’ from the Health Insurance
Act 1973, which defines registered nurse as ‘a person who is registered
under the National Law [Health Practitioner Regulation National Law] in the
nursing profession as a registered nurse’.[32]
Proposed subsection 54-1A(1) identifies the
providers that will need to meet this new responsibility:
- providers
that provide residential aged care to care recipients in a residential facility
- providers
of flexible care of a kind specified in the Quality of Care
Principles 2014 who provide care to care recipients in residential aged
care.[33]
Proposed subsection 54-1A(3) allows for the Quality
of Care Principles to provide a mechanism for granting an exemption to certain providers
in relation to the requirement to have an RN on site, and on duty, at all times
at a residential facility. Without placing restrictions on this power to
provide exemptions, proposed subsection 54-1A(4) allows the Quality of
Care Principles to provide for any or all of the following:
- the
process for the making of applications for the grant of an exemption in
relation to a residential facility
- the
circumstances in which an exemption may be granted
- the
conditions that apply to an exemption.
Estimated
impacts
The financial impact statement suggests that the
indicative financial impact of Schedule 1 will be $450.7 million over the
forward estimates.[34]
However, additional information on potential financial support for approved
providers to meet this new responsibility does not appear to be available.
The Government has estimated that approximately 80% of
residential facilities already fulfil or nearly fulfil the proposed
responsibility of having a RN on duty and on site 24 hours a day, 7 days a
week.[35]
In addition, the Government has estimated that this proposed responsibility
would require an additional 869 RNs in aged care.[36] The Aged & Community Care
Providers Association has estimated that the sector will need an additional
1,440 RNs to fill the gap.[37]
The Explanatory Memorandum includes the supplementary
regulatory impact analysis for the introduction of Schedule 1 and the increased
minimum care minute requirements, which outlines the following implementation
timeframes:
- from
1 October 2022: providers will be funded for a care minute target of an average
of 200 minutes, including 40 minutes with a RN, per resident per day
- from
1 July 2023: through this Bill, it will become mandatory to have a RN on site
and on duty at all times
- from
1 October 2023: providers will be required to provide an average of 200 care
minutes, including 40 minutes with a RN, per resident per day
- from
1 October 2024: providers will be required to provide am average minimum of 215
care minutes, including 44 minutes with a RN, per resident per day.[38]
The Explanatory Memorandum state that ‘the care minute
targets will form new care minute standards that will be mandatory from 1 October
2023’ and ‘this requirement will be set in subordinate legislation’.[39]
The implementation timeframe deviates from the Royal
Commission’s recommendation, that providers be required to have a RN onsite 16
hours per day (morning and afternoon shifts) by 1 July 2022, and an
RN onsite at all times from 1 July 2024.[40]
In the 2021–22 Budget, the Morrison Government provided
$3.9 billion in funding for providers to meet the minimum staff time standard
that it had planned to introduce, with its implementation plan at the time
going as far as October 2023, when it would introduce a new standard that would
require an average of 200 care minutes, with a minimum of 40 minutes with a RN,
per resident per day, along with a RN being on site for a minimum of 16 hours
per day.[41]
It is anticipated that care minutes and the requirements
to have a RN onsite at all times will inform the new star rating system, set
out in Schedule 2 of the Aged
Care and Other Legislation Amendment (Royal Commission Response) Bill 2022,
which passed the Parliament on 2 August 2022.[42]
In addition, the supplementary regulatory impact analysis
states that the Department is planning a multi-level evaluation strategy for
the AN-ACC reforms, which will use qualitative and quantitative metrices to
measure the ‘success against the objectives of the 24/7 RN and average minimum
care minutes reforms’.[43]
The Department will monitor the financial implications of
these new requirements through the payment system data from Services Australia.
No offsets were identified to offset the regulatory burden for affected
stakeholders with the Department predicting a total change in cost of $131
million (see Table 3).[44]
Table 3 Estimated regulatory burden for 24/7 RN and minimum 215 care
minutes per resident per day
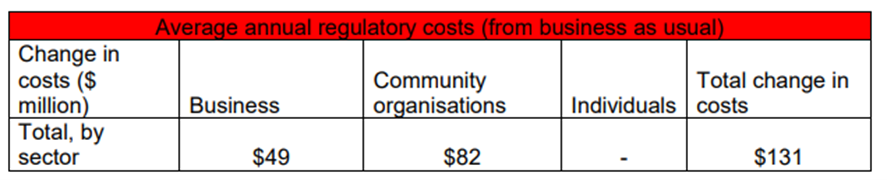
Source: Explanatory
Memorandum, Aged Care Amendment (Implementing Care Reform) Bill 2022, 26.
Schedule
2–Capping home care charges
The User Rights Principles
2014 currently enable approved providers to charge an exit amount to home
care package recipients exiting their service and specifies the rules and
responsibilities around home care pricing.
Section 56-2 of the Act outlines the responsibilities of
approved providers in relation to the provision of home care to a care
recipient. Item 1 of Schedule 2 will insert proposed paragraphs
56-2(aa) and (ab) into the Act, creating 2 new responsibilities for
home care providers that will:
- prevent
them from charging a care recipient an amount for ceasing their service and
- require
them to comply with the prices that can be charged, which will be specified in
the User Rights Principles.
In effect, this will prevent home care providers from
charging an exit amount and limit the prices a provider can charge for home
care packages.
Item 2 specifies that the 2 new responsibilities
are to be applied from the day of commencement. As such, some arrangements
agreed to in people’s existing home care agreements may no longer be applicable
from 1 January 2023.
Schedule
3–Transparency of information
Division 86 in Part 6.2 of the Act provides for the
protection of information acquired under or for the purposes of the Act or the Aged
Care (Transitional Provisions) Act 1997 that is either:
- personal
information (as defined in the Privacy Act 1988)[45]
- information
that relates to the affairs of an approved provider or
- information
that relates an applicant for a grant under Chapter 5 of the Act.
Item 1 inserts proposed section 86-10, which
requires the Secretary to make information in relation to aged care services
publicly available, in accordance with the Information Principles
2014. Without limiting the information that may be required to be made
publicly available, proposed subsection 86-10(2) enables the
Information Principles to provide for any or all the following:
- information
about the aged care provided through an aged care service that must be made
publicly available
- information
about the approved provider that must be made publicly available
- the
way the information is to be made publicly available
- the
period in which specified information must be publicly available.
Proposed subsection 86-10(3) specifies that
personal information must not be made publicly available, with the exception of
personal information about an individual who falls within the definition of key
personnel (discussed above).
According to the Explanatory Memorandum, the information
that is expected to be published following the introduction of these changes
will include:
- financial
information, including expenditure on care, nursing, food, maintenance,
cleaning, administration, and profits
- care
time provided
- key
personnel details
- information
about the staffing of the service.[46]