Stillbirth research in Australia
5.1
Research plays a critical role in identifying the causes, risk factors
and preventative measures for stillbirth and, together with innovation and education,
holds the key to understanding the best ways to reduce the rate of stillbirth
in Australia.
5.2
However, there is currently a lack of coordination and planning in
determining national research priorities and appropriate funding for stillbirth
research, as well as a lack of collaboration between the government, private
sector and philanthropic supporters.[1]
5.3
This issue is compounded by the stigma and silence that surrounds
stillbirth in the community more generally. Mr Bruce McMillan stated that,
whilst he had been aware of stillbirth prior to the stillbirth of his own baby,
he was shocked to learn of the magnitude of the problem.
As we know, there are over 2,000 stillbirths a year. Our
national road toll has not been over 2,000 since 1991. If governments of all
persuasions had allowed the national road toll to carry on for 27 years with no
reduction, there would be a national outcry at the failure of governments to
act. Yet here we are, in 2018, with virtually no government money being spent
on research into an area that impacts on so many lives and probably even less
money being spent on supporting organisations who support those of us who have
suffered the loss of a child.[2]
5.4
The impact of this lack of coordinated stillbirth research planning and
funding has significant consequences for individual families who have experienced
stillbirth. As Ms Lyndel Carbone stated, the lack of stillbirth research
hampers efforts to determine the cause of death and 'leads to huge levels of
stress and anxiety for subsequent pregnancies'.[3]
5.5
This chapter considers stillbirth research and funding issues, and
opportunities for innovative technology and corporate sector partnerships.
Government funding for stillbirth research
National Health and Medical
Research Council
5.6
The National Health and Medical Research Council (NHMRC) provides advice
to the Australian government on health and medical research, including research
into stillbirth, and approves clinical practice guidelines for use in
Australian heath care settings. It also manages research support and funding, including
grants for individual specific research projects and broad programs of research.[4]
5.7
Since 2007, the NHMRC has expended $5.9 million for grants relating to
stillbirth research, with a current commitment of grants of $13.4 million.[5]
This funding commitment includes $2.6 million over five years from 2016 for the
NHMRC Centre of Research Excellence in Stillbirth (Stillbirth CRE) at the
University of Queensland.[6]
5.8
The NHMRC has announced a new grant program which 'offers increased
flexibility to invest in areas of particular research need'. The program
includes Investigator Grant and Synergy Grant schemes, the latter of which
encourages joint-funding of research, and the Targeted Call for Research scheme
which 'focuses on research that has the potential to improve health outcomes for
the community, reduce the burden of disease on the health system and Australian
economy and contribute to the global research effort'.[7]
5.9
The NHMRC has also developed the NHMRC International Engagement Strategy
2016−2019
which outlines its approach to working with international partners.[8]
5.10
However, the NHMRC stated that applications for stillbirth research
funding have been few in number and numbers fluctuate from year to year, with
the level of funding for any particular disease dependent on 'the number and
quality of the research proposals received by the NHMRC'.[9]
Medical Research Future Fund
5.11
The Medical Research Future Fund (MRFF), established in 2015−16, is administered
by the Department of Health. It provides financial assistance to support health
and medical research and innovation, although it is not clear whether funding
has been provided for stillbirth research under this grant program.[10]
5.12
One of the MRFF priority areas, for which $17.5 million in funding is
being made available, is Maternal Health and First 2000 Days, which will
provide investment in research to improve health interventions between a woman's
pregnancy and the first five years of a child's life.[11]
5.13
The Australian Medical Research Advisory Board, which provides advice to
the government on the MRFF, has been conducting public consultations to inform
the development of the second round of MRFF priorities for 2018–2020, which
help to inform the government's decisions around how the MRFF is allocated.[12]
5.14
The National Perinatal Epidemiology and Statistics Unit (NPESU), University
of New South Wales (UNSW), recommended that targeted funding should be made
available for collaborative research partnerships, potentially through the
MRFF, which has the advantage of bringing together experts in perinatal
epidemiology, academic units, clinicians, parents and governments.[13]
Government research funding issues
5.15
Government funding for stillbirth research was lagging well behind other
areas of health research in Australia, even though stillbirth remains the
greatest cause of infant mortality. For example, cancer research received
$187 million between 2006 and 2018, and mental health research has been
allocated $331.81 million over the next four years.[14]
5.16
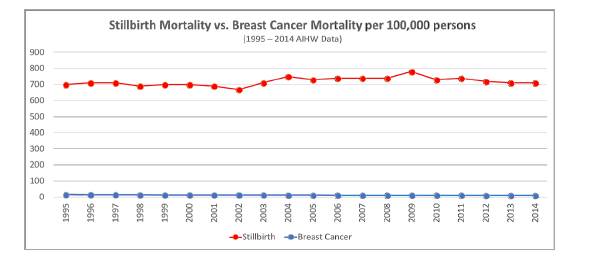
Using Australian Institute of Health and Welfare (AIHW) data, Red Nose
compared the number of deaths from breast cancer between 1994 and 2014 with
stillbirths per 100 000 persons (see Figure 5.1). In 2014, there were 2844
deaths from breast cancer from the Australian population of 23.5 million, and
2225 stillbirths from 313 000 births.[15]
Figure 5.1: Stillbirth mortality
vs. breast cancer mortality per 100 000 persons[16]
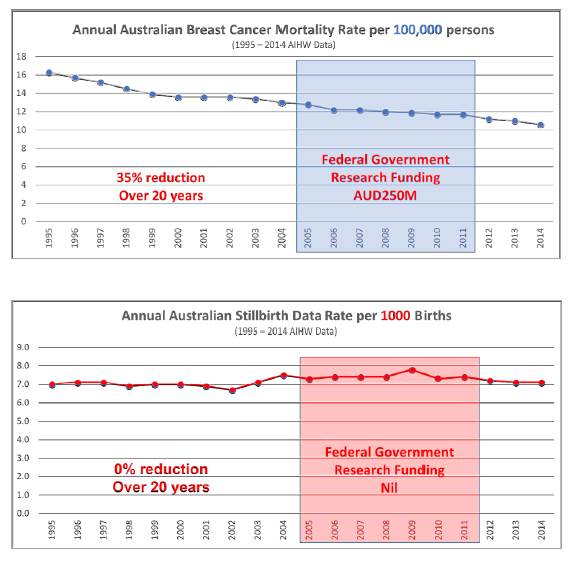
5.17
Red Nose noted that its investment of $17 million into Sudden Infant
Death Syndrome (SIDS) research had contributed to an 85 per cent reduction in
the incidence of SIDS. It then compared the levels of federal government
research funding in relation to the annual mortality rate for breast cancer
(per 100 000 persons) and stillbirth (per 1000 births), based on AIHW data for
1995 to 2014 (see Figure 5.2).
5.18
Red Nose noted that funding provided from the NHMRC for stillbirth
research has increased since 2012, totalling $5.4 million over the last six
years. It submitted, however, that a significant increase in funding is
required for stillbirth research and for developing new diagnostic tools to
prevent the 75 per cent of stillbirths that are most difficult to predict.[17]
Figure 5.2: Comparison
of government research funding in relation to annual mortality
rates for breast cancer and stillbirth[18]
5.19
The Global Stillbirth Advocacy Network observed that, in countries where
national governments have taken action, the rate of stillbirth has been
reduced. However, the limited amount of government funding available for
stillbirth research and education in Australia has resulted in fragmented,
short-term research efforts and a reliance on voluntary initiatives to provide
public education and support for bereaved families.[19]
5.20
Professor Craig Pennell, Senior Researcher, Hunter Medical Research
Institute, stated that one of the issues in research funding lies with the
three-year research grant cycle that inhibits the longer-term investment needed
to make inroads into stillbirth research and education.
If you look at the amount of money that's invested into
breast cancer research and then into stillbirth research, it's like a
hundredth. What is required is an investment into research, but that research
is discovery stuff and also implementation stuff. It needs to have a long-term
element, because to educate Australian doctors, midwives and patients about
something like this is going to take five years, realistically.[20]
5.21
A submission from the Department of Obstetrics and Gynaecology at the
University of Melbourne also noted the limitations of the cyclical nature of
current research funding arrangements which are also often project-based. The
intermittent and uncertain funding cycle reduces the capacity for large-scale
research programs, although the MRFF does offer the potential for longer-term, multi-disciplinary
and multi-faceted stillbirth research and education programs.[21]
5.22
Dr Adrienne Gordon, Neonatal and Perinatal Medicine Specialist,
Royal Australasian College of Physicians, highlighted the benefits of having a
greater diversity of expertise and interests amongst those allocated funding
for stillbirth research, noting that funding for cancer research is provided
through a range of organisations and that this approach has resulted in
significant breakthroughs in the prevention and treatment of cancer.[22]
5.23
Associate Professor Camille Raynes-Greenow of the School of Public
Health, University of Sydney, proposed that a roundtable approach to
coordinating research funding—involving
relevant stakeholders including government, philanthropic and corporate representatives
as well as researchers and care providers—would
be preferable to the current piecemeal approach.[23]
5.24
Ms Victoria Bowring, Chief Executive Officer, Stillbirth Foundation
Australia, noted that NHMRC has traditionally allocated funding for 'clinical-style
research' into stillbirth, but that there has been no significant reduction in
the rate of stillbirth. She stated that there is currently no dedicated
national stillbirth research fund administered by an independent organisation,
and proposed that the Stillbirth Foundation Australia could provide such a
service, in partnership with a government-led national organisation for
stillbirth research and education.
We have a unique ability in being able to have insight into
the family's experience around stillbirth, but also the understanding of the
importance of particular types of research et cetera. We don't have a
particular allegiance to any single institute or organisation. In this
instance, because it is such a multifaceted issue, it needs to be dealt with in
such a way that all of the stakeholders that are a part of the problem are also
part of the solution, and not just one particular entity.[24]
Other research funding
5.25
There are isolated examples of stillbirth research being undertaken in
Australia without NHMRC funding.
5.26
The Australian Longitudinal Study on Women's Health (ALSWH), funded by
the Commonwealth Department of Health, currently includes about 250
collaborative projects on women's health issues, including four investigating where
stillbirth may be a factor.[25]
5.27
Some funding for stillbirth research is provided by charitable
organisations set up by and for families affected by stillbirth. Stillbirth
Foundation Australia is the first Australian charity dedicated to stillbirth
research, and has provided around $1 million to research projects since 2009
through various research institutes, hospitals and parent advocacy
organisations.[26]
5.28
The Hunter Medical Research Institute (HMRI) noted that it had been the
beneficiary of research funding from the philanthropic Haggarty Foundation. The
HMRI suggested that any national coordination of research funding should
recognise the potential for both community engagement and philanthropic
support, and its research program and priorities should be oversighted by a
high-calibre, multi-disciplinary scientific committee.[27]
5.29
Stillbirth CRE partnered with the Stillbirth Foundation Australia to
provide additional research funding which has largely been provided through
community and corporate engagement, and noted that there is a need for greater
government involvement in coordinating these activities.
As with other significant public health issues, a focussed
effort is needed and investments that could bring a wider group under one
umbrella would have significant benefits. The Stillbirth CRE has taken initial
steps to coordinate activity and effort but a clear direction from governments
to ensure that all research and public awareness campaigns are cost-effective
and achieve maximum impact would be highly beneficial.[28]
5.30
However, most research and investigation into stillbirth cause and
prevention is still researcher-led, with minimal funding provided by government.[29]
Stillbirth Foundation Australia argued that funding for researching what
constitutes a national health crisis should not be borne only by those who have
experienced stillbirth.[30]
Research priorities
5.31
Up to 60 per cent of stillbirths at term in Australia are unexplained,
highlighting the urgent need for further research into understanding why these
deaths have occurred.[31]
5.32
In addition, for every one stillbirth there are another 99 births that
narrowly avoid ending in stillbirth, making it imperative for research to
identify not only why unexplained stillbirths occur but also the determinants
of stillbirth in early fetal development.[32]
Stillbirth is a little bit like the iceberg that you can
see—underneath it you've got that 90 per cent of babies who were at risk but
fortunately didn't die. By studying that group, you can learn a lot about the
causes of stillbirth as well as optimising the outcome for a much larger number
of people, improving...the ability to be educated and participate fully in our
community and, almost certainly, having longer, healthier life expectancy.[33]
5.33
The NHMRC determines research priorities based on current and emerging
health issues in Australia and internationally, and identifies the National
Health Priority Areas which receive a substantial proportion of NHMRC funding.
Stillbirth is not identified as a National Health Priority Area.[34]
5.34
The NPESU noted that research priority-setting had been undertaken by
the Perinatal Society of Australia and New Zealand and members of the Stillbirth
CRE, in consultation with all stakeholder groups including consumers, and recommended
that these research priorities should inform future funding initiatives that
encourage collaborative research between academia, governments, consumers and
stillbirth organisations.[35]
5.35
Ms Pip Brennan, Executive Director of the Health Consumers' Council (Western
Australia) stated that the NHMRC had emphasised the need for research
priorities to be driven by bereaved parents and families. She noted that the
submissions to this inquiry from those who had experienced stillbirth suggested
a range of excellent research questions, and argued that consumer generated
research questions will help to ensure best practice in stillbirth research. Ms
Brennan highlighted the need to:
- take verbal autopsies from parents and other key care providers
who are not currently consulted in a stillbirth review;
-
establish benchmarks for monitoring the rates of stillbirth
across Australia;
-
make research and data more accessible nationally; and
-
translate stillbirth research into practice, for example by
requiring customised fetal-growth charts to enable intrauterine growth
retardation to be identified sooner.[36]
5.36
Stillbirth CRE endorsed this approach.
Parents must remain at the centre of all future research as
they inform research priorities and can provide invaluable advice on how to
most effectively involve parents and families in appropriate ways.[37]
5.37
Stillbirth CRE outlined its national research program, developed in
consultation with parents, parent-based support and advocacy organisations,
foremost international expert researchers and clinicians, and the Australian
community. The program addresses four major priority areas:
- improving care and outcomes for women with risk factors for
stillbirth;
-
developing new approaches for identifying women at increased risk
of stillbirth;
-
implementing best practice in care after stillbirth and in
subsequent pregnancies; and
-
improving knowledge of causes and contributors to stillbirth.[38]
5.38
Achieving meaningful and ongoing change requires additional government
funding and policy support for a unified national priority driven approach building
on the Stillbirth CRE model so that government, philanthropic and corporate
funding bodies can work together to produce the best outcomes. According to
Stillbirth CRE, the most important research priority is addressing the gap
between 'what is known and what is done in every day clinical
care of women having a baby in Australia'.
Major gains can be made by simply doing better what is
already known to be best practice, and although implementation projects may not
be as attractive to funding bodies, it is vitally important that there is a
rigorous approach to translating new ideas into practice.[39]
5.39
The National Rural Health Alliance advised that research and education
priorities to improve health outcomes and increase the quality of care to women
in rural and remote Australia must include obesity prevention and management,
and cultural safety and cultural competence.[40]
5.40
Other suggestions included:
- introducing research performance as a key performance indicator
for chief executives of tertiary hospitals across Australia;
-
making a long-term investment in stillbirth research in order to allow
time to properly implement research findings;
-
implementing a centrally coordinated national process to enable
pathologists to conduct collaborative investigations into stillbirth cases,
similar to the research being conducted in relation to babies that have died
from SIDS;[41]
-
elucidating the causal pathways to stillbirth and neonatal death;
-
examining stillbirth by location, cultural/ethnic background, and
socioeconomic circumstances; and
-
assessing the effectiveness of public health campaigns.[42]
Identifying mothers at risk
5.41
As in other high-income countries, the risk of stillbirth for Aboriginal
and Torres Strait Islander women and women who live with social disadvantage is
far higher than other Australian women.[43]
...statistics show that the rate of stillbirth increases the
further away women are from an Australian major city. Stillbirth can have long
term and economic consequences and adds to the inequitable health and social
burden that people in rural and remote Australia already experience.[44]
5.42
Contributing factors include perinatal infection, fetal growth restriction
(FGR), unexplained antepartum fetal death, and maternal conditions (mainly
diabetes). However, there has been little reduction in the gap between
Indigenous and non-Indigenous women in relation to stillbirth rates, indicating
that this area is a priority for future research.[45]
5.43
The Multicultural Centre for Women's Health drew attention to
differences in the risk of stillbirth in relation to country of birth, and emphasised
the need for more research to shed light on the causes and contributing factors
to higher stillbirth rates amongst women from CALD backgrounds, including late
presentation to antenatal care and disparity between rural and regional and
metropolitan rates of stillbirth.[46]
5.44
Submitters and witnesses also raised other risk factors that require
further research, including FGR, ageing of placenta, and hypertensive
disorders.
Fetal growth restriction
5.45
The Royal Australian and New Zealand College of Obstetricians and
Gynaecologists (RANZCOG) noted that FGR and intrapartum hypoxic death together
contribute to about eight per cent of all stillbirths. As a strong risk factor,
FGR screening, diagnosis and management are important to protect against
stillbirth.[47]
5.46
Professor Susan Walker, Head, Department of Obstetrics and Gynaecology
and Chair, Women's and Newborn Heath Network at the Melbourne Academic Centre
for Health agreed.
Fetal growth restriction is associated with a fourfold
increase in the risk of stillbirth, is a common antecedent to stillbirth in
labour and seems the likely mechanism linking factors such as obesity, medical
conditions and increasing maternal age with stillbirth. Disappointingly,
current care detects only 20 per cent of babies destined to be born small. Yet
if we can discover better ways to identify small babies, we know we can halve
their stillbirth risk. In conclusion, we suggest that by daring to connect,
daring to inspire and daring to discover, we bring the day when families may be
spared the tragedy of preventable stillbirth one day closer.[48]
5.47
HMRI also pointed to the importance of conducting research into poor
fetal development more generally, especially in vulnerable communities, noting
that for every one stillbirth there are another 99 that narrowly avoid
stillbirth.[49]
5.48
RANZCOG cited international studies showing that elective induction of
labour at 39 weeks could reduce the risk of stillbirth and other adverse
perinatal outcomes.[50]
However, Professor Steve Robson stressed that RANZCOG was not advocating early
induction for all pregnancies.
We're not saying for one second that everybody should be
induced at 38 or 39 weeks or whatever. We're saying that the evidence around
the world is coming down saying, 'If you're worried—if you have concerns about
the condition of a baby, about how it's tolerating things—then a policy of
having that low threshold, offering it to women and allowing them to make a
choice, seems to be a safe thing. It doesn't seem to be associated with the
other things that we worry about, like a rising caesarean section rate.[51]
Placental insufficiency
5.49
Laureate Professor Roger Smith, Director, Mothers & Babies Research
Centre, HMRI, drew attention to the recent discovery that stillbirths can be
triggered by ageing of the placenta, and noted that the placenta is part of the
baby not the mother.
So if the placenta ages prematurely, it may well have nothing
to do with the mother, and I think that's important to think about. But it's
also important for us to focus our research efforts on understanding this
extraordinary organ on which the baby is dependent.[52]
5.50
One submitter, who experienced a stillbirth despite having no known risk
factors, considered that there needed to be better detection of placental
insufficiency—an
issue which is responsible for 24 per cent of stillbirths—as well as research into
the effects of sleep apnea and sleep disordered-breathing on fetal health.[53]
Hypertensive disorders
5.51
The Department of Obstetrics and Gynaecology at the University of
Melbourne noted that preeclampsia is the most common and serious medical
condition complicating pregnancy, responsible for 70 000 maternal deaths
globally and over 500 000 perinatal deaths every year. It considered
improved detection and management of hypertensive disorders of pregnancy to be
a leading priority to reducing stillbirth risk.[54]
Innovative technology and coordinated research efforts
5.52
There is an extensive international research community working together
to address stillbirth. The NHMRC, recognising that no single country has the
resources, skills and capacity to address all health and medical research
challenges, supports funding schemes that have provision for international
collaborations.[55]
5.53
Ms Stephanie Vowles cited recent financial modelling on the economic
benefits of investing in medical research, noting that 'for every $1 spent on
research, at least $2 was generated in additional economic output'.[56]
5.54
Several submitters claimed that their stillbirth may have been prevented
if their clinician had access to consistent and timely information,
highlighting the potential role innovative new technology such as mobile phone
apps offered in education, screening and delivering better health outcomes,
especially for high risk births.[57]
5.55
Ms Ellana Iverach submitted that most of the current research effort
into stillbirth is focused on post-death and support requirements, and argued
that more research needs to be done into stillbirth prevention. She pointed to
recent technological advancements in fields such as neuroscience, which have
allowed researchers to study the brain in new ways and gather data to build
prevention and treatment strategies, and suggested that similar advancements
may help to prevent stillbirth.[58]
5.56
Stillbirth CRE reported that bereaved parents had identified the need
for a 'cure' as their highest priority during consultative meetings, and
expressed interest in partnering with the corporate sector and exploring
opportunities for potential use of new technologies including:
- improving detection of the unborn baby who is at-risk;
-
detailed evaluation of potential harms, including anxiety, of
unnecessary intervention (such as preterm delivery); and
-
prevention of spontaneous preterm birth (which contributes to
around 15−20 per
cent of stillbirths).[59]
Mobile phone apps
5.57
New and relatively cheap technologies such as mobile phones can already
deliver health messages, help lines and real-time monitoring and reporting of
births and deaths. They also have the potential to increase communication and
data-sharing amongst health providers and communities more generally.[60]
5.58
Different countries have developed successful ways of educating women
about the risks of stillbirth. A phone app developed in Finland, for example,
provides a simple and effective tool for educating people about the risks of
stillbirth, although it should also be coupled with a message that helps to alleviate
any fear or guilt.[61]
5.59
Stillbirth CRE reported on the current Australian trial of a mobile
phone app called 'My Baby’s Movements' (MBM), developed by the Mater Research
Institute, University of Queensland and funded by NHMRC. It aims to reduce late
gestation stillbirth through earlier reporting and improved clinical care. The
app is not yet available in multiple languages due to a lack of funding.[62]
5.60
The trial forms part of a large research project being conducted in
maternity hospitals across Australia and New Zealand, and led by experts from
Australia, New Zealand, the Netherlands, the United Kingdom (UK)
and Norway. Stillbirth CRE is collaborating with researchers in the UK to
combine data from similar trials to explore the differential effects in higher
risk groups.[63]
5.61
An educational program has also been developed for clinicians on the MBM
app's use and management of women reporting decreased fetal movement to reduce
stillbirth in late gestation stillbirth.[64]
Wearable technology for monitoring
pregnancy
5.62
Opinions were divided over the merit of relying on wearable technology
to monitor pregnancies.
5.63
Mrs Doshni Stewart recommended wider application of wearable technology
for monitoring fetal movement. Mrs Stewart claimed that such technology offers
a solution to the lack of resources in public hospitals, is not subject to
human error, and has the potential to reduce the risk of stillbirth, especially
for high-risk pregnancies.
With increasing high-risk pregnancies, the automation of
certain processes within the health system is necessary not only to provide
adequate health care to our growing population but also to drive efficiencies
in our public hospitals. I recommend that more widespread use of fetal
monitoring and other relevant technology be implemented. I believe there were
elements of my antenatal care which could have been different and which could
have changed what happened to Coralie. Our hope is that this inquiry will
result in changes to the care of pregnant women that may reduce the incidence
of stillbirth in this country, as has been achieved in other countries around
the world.[65]
5.64
One submitter argued that such technology may be particularly helpful
for Aboriginal and Torres Strait Islander women in remote locations, where the
rate of stillbirth is higher.[66]
5.65
Dr Jane Warland warned against funding wearable devices at the expense
of innovative technology to better support maternity care providers to detect
and manage the fetus at risk.[67]
Stillbirth CRE expressed similar reservations, noting that there are other
methods of predicting at-risk pregnancies, although these require further
research.
The current focus of innovation is on devices to detect
changes in fetal movement, although it is unclear if this has real potential to
change outcomes. There are other examples of new technology in which biomarkers
might either predict the pregnancies ‘at risk’ or detect the vulnerable fetus
late in gestation, but both of these require much more research.[68]
5.66
Associate Professor Raynes-Greenow pointed out that some groups in
Australia will be disadvantaged because of the cost of such technology.
We don't consider that technology will solve stillbirth, and
it most likely would have unintended consequences, such as unnecessary
interventions or causing anxiety, and it is most likely only ever going to be
available at a personal level for people who can afford it.[69]
5.67
The Centre for Midwifery, Child and Family Health cautioned that:
...technology is appropriately and carefully used and listening
to women should be the first technology used. The risk is that clinicians tend
to concentrate on the technology (the machines that say everyone is alright or
that things are going wrong) and often forget to prioritise what the woman
feels or is experiencing. Very often, women say that ‘they knew something was wrong’
but that all the tests they had showed no problems and she was sent home.
Listening to women should be the first technology applied in this area.[70]
5.68
Professor Caroline Homer, Distinguished Professor of Midwifery,
representing the Centre for Midwifery, Child and Family Health, considered that
women are generally best at monitoring their own baby's movements, 'but if they
don't know that they should be monitoring something they're going to miss out'.[71]
Genetic testing
5.69
The AIHW noted that, in 2013−14,
27 per cent of stillbirths were caused by a congenital anomaly, making it the
leading cause of stillbirth death in Australia. It noted that work is
commencing shortly to re-establish an Australian Congenital Anomaly Collection
linked to the National Perinatal Mortality Data Collection.[72]
5.70
Professor Hamish Scott, Head of Genetics and Molecular Pathology
Laboratory, SA Pathology, and Associate Professor Christopher Barnett, Head,
Paediatric and Reproductive Genetics Unit, The Women's and Children's Hospital,
Adelaide, noted the limitations of standard autopsy in relation to stillbirth
and reported on the success of their NHMRC-funded genomic autopsy study in
identifying genetic causes of unexplained perinatal death, including
stillbirth. The service is now available to all major perinatal centres in
Australia.[73]
5.71
Professors Scott and Barnett advised that they had also established a
national and international network of collaborators across 10 countries.
Working closely with the Broad Institute of MIT and Harvard,
world leaders in genomic technologies, we are delivering a world-class research
service model to Australians to provide them with a genetic diagnosis of
problems in pregnancy. Our model has been adopted nationally as part of this
NHMRC-funded study and will involve all major women’s and children’s hospitals
in Australia, including 37 clinicians and 20 researchers. We are also guiding
two international groups in Boston, USA and Toronto, Canada to establish their
own studies based on our model. We are also working with industry to develop
the tools needed to help patients access IVF and genetic diagnosis of embryos
if they are at risk of having a genetic condition in their next pregnancy.[74]
Corporate sector partnerships
5.72
Stillbirth CRE noted that, with some notable exceptions such as the
Stillbirth Foundation Australia and PriceWaterhouseCoopers (PwC) partnership,
there has been little collaboration between stillbirth researchers and the
corporate sector.[75]
5.73
However, there is clearly a role for greater involvement of the private
sector in developing innovative new technology and commercial products as well
as non-commercial interventions that may help in stillbirth prevention,
research and education.[76]
5.74
The NHMRC highlighted the importance of private-public partnerships for
delivering better health outcomes. Recent partnerships funded by the NHMRC have
included:
- a universal blood test for all pregnant women to measure
circulating proteins that are likely to be of placental origin and identify FGR,
a major cause of stillbirth; and
-
the biochemical processes within the placenta that lead to FGR
and placental ageing.[77]
5.75
The NHMRC also noted that Stillbirth CRE, in partnership with the
Australian and New Zealand Placental Research Association, is establishing a
national biobank to support ongoing placental research into the causes and
predictors of stillbirth.[78]
5.76
Several submitters highlighted the importance of a national biobank to improve
research and clinical practice.[79]
However Stillbirth CRE noted that, in the absence of any clinically useful
tests for early predictors of stillbirth, longer-term research funding and
changes to ethics approval processes are urgently needed to facilitate its
development.
MRFF funding is one alternative to supporting long term
initiatives that will have significant long-term benefits. While there has been
support by individual families for research to be carried out where an adverse
pregnancy outcome has arisen, Human Research Ethics Committee (HREC)
requirements are restrictive particularly around sharing of data across
centres. Such data are urgently needed if large scale collection of samples,
amenable for later research, is to be permitted by HREC under a possible waiver
of consent, or similar approach.[80]
Committee view
5.77
There has been no reduction in the rate of stillbirth in Australia over
the past two decades, despite modern advances in medical practice and health
care, and stillbirth remains the greatest cause of infant mortality.
Nevertheless, as international studies have shown, when a national government
takes action, the rate of stillbirth declines.
5.78
The committee acknowledges that the Australian government, through the
NHMRC, has recently invested funds in a research project to investigate why the
stillbirth rate is so high in Australia, particularly in rural and remote
areas, and to seek strategies for prevention. The committee heard evidence,
however, that funding for stillbirth research lags behind other areas of health
research.
5.79
The committee recognises that Australian stillbirth researchers,
clinicians, health professionals, advocacy groups and individuals have been
working tirelessly to understand the causes of stillbirth and identify the
strategies that will reduce the incidence of stillbirth. Such research is
absolutely crucial, but much of this research and investigation into stillbirth
cause and prevention is being undertaken with minimal funding provided by government.
5.80
The committee is concerned that stillbirth will continue to be a 'hidden
tragedy' if it continues to be neglected as a national public health issue and is
not prioritised in public health research funding.
Recommendation 5
5.81
The committee recommends that, through the Australian Health Ministers'
Advisory Council, the Australian government leads a process to establish a set
of national stillbirth research funding priorities for the next 10 years, drawing
on those developed by the Perinatal Society of Australia and New Zealand and Centre
of Research Excellence in Stillbirth. This set of priorities should:
- draw on the experiences and knowledge of parents, parent-based
support and advocacy organisations, international expert researchers,
clinicians and other health professionals; and
-
enable government, philanthropic and corporate funding bodies to identify,
prioritise and coordinate efforts to produce the best and most cost-effective
outcomes through collaborative research programs, including 'discovery projects'
which explore new technologies that may prevent stillbirth.
5.82
Government research funding is currently restricted to three-year cycles.
Stillbirth researchers are concerned that such arrangements limit stillbirth
research which, because of the nature and complexity of the issue, requires
longer-term funding in order to allow for large-scale, multi-disciplinary
research to be undertaken and the results used to make improvements in clinical
practice and stillbirth prevention strategies.
Recommendation 6
5.83
The committee recommends that the Australian government reviews current
research funding arrangements administered by the National Health and Medical
Research Council, in consultation with a roundtable of relevant stakeholders,
to examine options for longer-term funding cycles for targeted, large-scale,
collaborative research partnerships, potentially through the Medical Research
Future Fund.
5.84
One area of particular interest to the committee is the potential for
new technologies to identify women at increased risk of stillbirth and other
adverse pregnancy outcomes. The committee acknowledges that new wearable
technologies may offer women a convenient tool for monitoring a pregnancy, but
cautions that the use of such technologies should be balanced against the risk
of downplaying the importance of a woman trusting her own instincts and
experiences during pregnancy.
5.85
The committee supports the development of a national biobank to enable
researchers to have access to a large-scale collection of samples in order to
determine causes and early predictors of stillbirth. It considers that the Australian
government should give urgent consideration to:
- provision of long-term dedicated funding and support through the
MRFF; and
-
a review of Human Research Ethics Committee requirements for
access to the biobank and sharing of other large repositories of research data
relevant to stillbirth research.
Recommendation 7
5.86
The committee recommends that the Australian government gives urgent
consideration to the allocation, through the Medical Research Future Fund, of
long-term dedicated funding and support for the development of a national
biobank for stillbirth placenta research.
Navigation: Previous Page | Contents | Next Page