Chapter 5
Issues—governance
Instead of a “mental health system”...we have a collection
of often uncoordinated services that have accumulated spasmodically over time,
with no clarity of roles and responsibilities or strategic approach that is
reflected in practice.[1]
National Mental Health Commission
National Review of Mental Health Programmes and Services
Introduction
5.1
The committee has heard much evidence about mental health issues over
the course of its 38 hearings. As a result, the committee agreed to hold three
hearings on mental health issues, with a key focus on the findings of the
National Mental Health Commission and the government's consideration of its
response.
5.2
At the committee's public hearings on 26 and 28 August, and 18 September
in Canberra, Sydney, and Brisbane respectively, the committee heard from a
diverse range of mental health groups, carers, consumers, service providers and
others, including the National Mental Health Commission and the Mental Health
Commissioners of Queensland and New South Wales.
5.3
This chapter sets out the issues raised with the committee during its
hearings, and in the submissions received from groups and individuals, in
relation to governance and funding in mental health service and programme
delivery. These issues include:
-
Fifth National Mental Health Plan;
-
Mental Health Service Planning Framework;
-
Outcomes focussed funding with reporting; and
-
Policy and funding uncertainty.
5.4
The committee has examined each of these issues from three perspectives:
the evidence it received from witnesses; the findings of the Commission; and,
where it exists, Government reaction to the Commission's findings. The
committee summarises its findings and makes its recommendation towards the end
of this chapter. Issues relating to delivery of services and programmes, and
the committee's recommendations, are in Chapter 6.
Fifth National Mental Health Plan
5.5
In the 2015-16 Budget, the Government committed to work in collaboration
with States and Territories to develop the fifth national mental health plan.[2]
5.6
The Fourth National Mental Health Plan set:
...an agenda for collaborative government action in mental
health for five years from 2009, offers a framework to develop a system of care
that is able to intervene early and provide integrated services across health
and social domains, and provides guidance to governments in considering future
funding priorities for mental health.[3]
5.7
The Fourth National Mental Health Plan was developed to guide reform and
actions as part of the implementation of the National Mental Health Policy,
which was endorsed by Australian Health Ministers in 2008.[4]
The National Mental Health Policy sits within the National Mental Health
Strategy, endorsed in April 1992 by the then Australian Health Ministers'
Conference as a framework to guide mental health reform.[5]
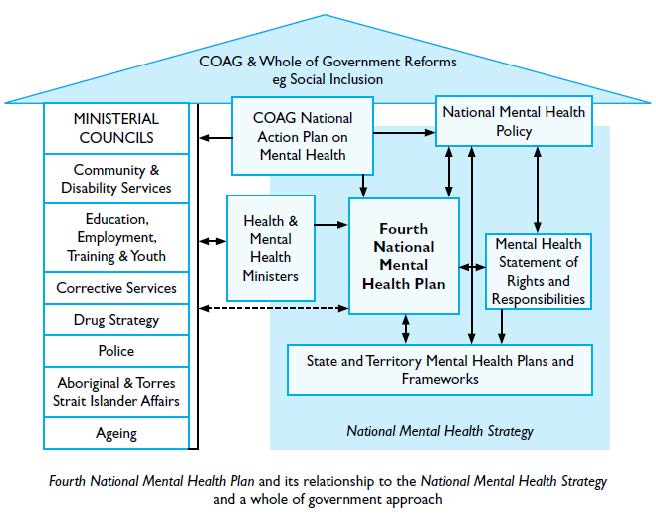
5.8
Figure 5 below shows the relationship of the Fourth National Mental
Health Plan to the National Mental Health Policy, the National Mental Health
Strategy, and the other elements of mental health within the COAG framework.
Figure 5—Fourth
National Mental Health Plan in context[6]
5.9
Mr Cormack told the committee that work on Fifth National Mental Health
Plan is in its early stages:
...the Fifth National Mental Health Plan was a decision taken
by the COAG health council to progress that work. It is really just in its
early stages. It has been assigned to be led by Tasmania under the Mental
Health and Drug and Alcohol Principal Committee of AHMAC [the Australian Health
Ministers' Advisory Council] auspices, and a working group has been established
to progress that work. Through the course of the development of the Fifth
National Mental Health Plan there will be extensive consultation with a wide
range of stakeholders within the Commonwealth and also within state and
territory governments, the NGO sector and the private sector. At this stage...I
think there have been two meetings of the working group. It is hitting its
straps, but it is certainly not into the level where they would be ready for
wide-scale consultation with the sector. That has always been the process for
previous national mental health plans. There is extensive consultation, and
that will be the case with the Fifth National Mental Health Plan.[7]
5.10
Witnesses generally felt that the development of the Fifth National
Mental Health Plan should be considered in light of the findings of the
Commission's review. For example, Mr David Meldrum, the Executive Director of
the Mental Illness Fellowship of Australia argued that to be successful the
Fifth National Mental Health plan needed accountability and evaluation
mechanisms:
The First National Mental Health Plan...had a little bit of
bite because of its newness and, in fact, it came out of a fair bit of argument
between people on which direction we should be heading. In that sense, it was
quite influential.
With the last couple [of five year mental health plans], in
my view, you have been able to read them and say, 'That's about right,' but
that is about the end of the conversation. There has been nobody made
accountable to do something about those, particularly in the Commonwealth-state
divide. You have mental-health plans in every state and territory being
developed, as we speak. They either have just been released or are about to be
released or are starting to be formulated. That is the situation at any given
time. Most of them are the same. Most of them do not have any sort of a
timetable or accountability for implementation. This one needs state ministers
and the Commonwealth minister and key departmental heads not only to be saying,
'This looks like the way mental-health services ought to look' but also 'It
contains some specific accountabilities for outcomes that will lead to some
implementation.'[8]
5.11
Professor Malcolm Hopwood, President of the Royal Australian and New
Zealand College of Psychiatrists maintained that the Fifth National Mental
Health Plan was an opportunity to organise the government's response to the
Commission's findings, in a way which included both a national and regional
perspective:
I would support the idea that, both at a regional level and a
national-plan level, a national mental-health plan is an opportunity to say:
'What are the kinds of elements that we really need in a service response that
are going to give us the best chance of solving these kinds of difficult
problems?' Of course, there are going to be local variables within that. One of
our challenges...is that we need a diverse sector to meet the needs of the people
we work with. But that can end up being confusing, difficult to approach and,
at times, more competitive than is helpful. A national mental-health plan is a
great opportunity for us to say a little bit more clearly how we want these
elements to fit together, how we are going to govern that niche region and
really tell if it is having the impact...We really want to make the best of that
opportunity.[9]
Mental Health Service Planning Framework
5.12
The National Mental Health Service Planning Framework (the Framework)
was an initiative of the Fourth National Mental Health Plan for:
...the development of a national service planning framework
that establishes targets for the mix and level of the full range of mental
health services, backed by innovative funding models.[10]
5.13
The aim of the Framework was to:
...better estimate service demand across the service spectrum
and across different care environments and will allow jurisdictions to identify
service areas requiring investment. This project will reform mental health
planning in both Australia and internationally and will provide the mental
health planning community with a solid tool from which to establish creative
resource solutions.[11]
5.14
The Framework was to be guided by the following principles:
-
Nationally consistent – The NMHSPF will provide an 'Australian
average' estimate of need, demand and resources for the range of agreed mental
health services required across the lifespan and across the continuum of care
from prevention to tertiary treatment.
-
Flexible and portable – The NMHSPF will be flexible to
jurisdictional adaptation, and will be presented in a user friendly format.
However, some technical aspects cannot be altered or the validity of the
product will be compromised.
-
Not all, but many – To ensure national viability, the NMHSPF will
not account for every circumstance or service possibly required by an
individual or group, but will allow for more detailed understanding of need for
mental health service across a range of service environments.
-
Not who, but what – The NMHSPF will capture the types of care
required, but will not define who is best placed to deliver the care. Decisions
about service provision will remain the responsibility of each state/ territory
and the Australian Government.
-
Evidence and expertise – The NMHSPF will identify what services
'should be' provided in a general mental health service system. Contemporary
mental health practice, epidemiological data and working with key stakeholders
with diverse expertise will underpin the technical, clinical and social support
mechanisms that will form the content of the framework.[12]
5.15
Consultation with a range of mental health sector stakeholders was built
into the Framework structure. The project was to be supported by an executive
group comprising of mental health representatives from all Australian
jurisdictions, and a modelling group with three expert groups:
-
Primary Care / Community / Non Hospital Expert Working Group
-
Psychiatric Disability Support, Rehabilitation and Recovery
Expert Working Group; and
-
Inpatient / Hospital Based Service Expert Working Group.[13]
5.16
The modelling group also included a consumer and carers reference group
and consumers and carers could participate through the three expert groups.[14]
5.17
Funding for the Framework was provided by the Commonwealth, through the
Department of Health and Ageing (now the Department of Health) and the project
was led by the NSW Ministry of Health in partnership with Queensland Health and
other jurisdictions. The timeframe for the project was two years, with the
project to be completed by 2013.[15]
5.18
Mr David Butt, CEO of the National Mental Health Commission told the committee
that when the Commission began its review, it requested a copy of the Framework
from the Department of Health, but it was not provided:
No, we were not [provided with a copy of the NMHSPF]. I think
we have commented previously that it would have been useful to have it, because
what it does is model the staffing and the services to respond to particular
assessed needs. So that would have been a very useful tool, and it probably is
a very useful tool. My understanding—and you really would need to check this
with the department again—is that it has been distributed across all the states
and territories and they are all looking at the implications and whether it is
in fact a good model...[16]
5.19
Mr Butt's understanding was that the Framework was still under consideration
by the federal and state governments:
I think some concern has been raised by some states—not all
states—that the potential implications of implementing that model would be
quite expensive, but the resourcing issue is a separate issue from the planning
tool, from our perspective. Governments have to make decisions about how much
investment they will put into particular services and obviously there are
finite resources available. So we would certainly be eager to see that services
planning framework finalised and released.[17]
5.20
Other witnesses told the committee that the Framework was eagerly
awaited by the mental health sector. Mr Quinlan, CEO of Mental Health Australia
advised that:
It is fair to say that those across the sector who invested a
lot of time—and it is true to say that there were some hundreds of people
across the sector—in developing that model [the NMHSPF] have been somewhat
frustrated by the fact that it has not yet managed to come out the other end of
the process. This is because it is likely to give us some of the answers to the
questions that David Meldrum [Executive Director, Mental Illness Fellowship of
Australia] alluded to—what are the numbers [of mental health consumers and
mental health services]?—and gives us a platform where we can have a sensible
debate about who is in what group and where the sorts of services for them
should rest.[18]
5.21
According to representatives of the Department of Health, the Framework
is still under development. Mr Cormack described the current situation relating
to the Framework as 'a collaborative piece of work that is being progressed
through the Australian Health Ministers' Advisory Council. It is well advanced.'[19]
5.22
Ms Janet Anderson, First Assistant Secretary of the Health Services
Division of the Department of Health expanded on Mr Cormack's answer:
...the framework exists now, but it is what is known as a beta
version. It has had some testing in several jurisdictions, including New South
Wales, WA and Queensland. The Mental Health and Drug and Alcohol Principal
Committee of AHMAC [the Australian Health Ministers' Advisory Council] has
agreed to establish a steering committee to take forward the framework into its
further and final stages of development. They are aware of a number of areas
where further work is required. It does need some further effort. Apparently
there are some technological bugs, which I do not presume to know much about,
but they also want to look more closely at some elements of the design model
such as the way the care packages are put together. There are further
considerations to be given to rural and remote residents in terms of mental
health and also to Indigenous communities, and at the far end of all of that
there is the need to seek state and territory sign-off to the framework in
order for it to be a genuinely national product.[20]
5.23
Ms Anderson explained that the 'beta version' was 'a testing model':
It is something which is recognised as not yet fully
developed but has enough of the moving parts to see how it might apply in real
life but in a piloted way. It is not currently being used as a planning model,
but it is being tested as if it could be used and to identify things that might
need further development. Indeed, that list which I partially rendered is still
being developed. There is still the need for further identification of the
issues to be worked on to move it from its current testing phase into a
framework which nine jurisdictions can agree to.[21]
5.24
Ms Anderson's understanding of the timeframe for progressing the
Framework to completion was that approximately another year would be required:
My understanding is that the expectation of the time frame is
that it will take at least 11 or 12 months—probably to the middle of the next
calendar year—before this work is completed. A steering committee is being
established that is chaired by the Commonwealth and has representation from a
number of jurisdictions. It has not yet met, and I think its first meeting will
be in September. There is work now underway to establish its specific terms of
reference and a work plan which will guide its efforts over the coming 12
months.[22]
5.25
The fact that the Framework was in 'beta version' was the Department's
reason for the framework not being provided to the Commission during its
review. Mr Cormack argued that:
[The Framework] is a Commonwealth/state piece of work. It
obviously has very significant implications for the way services are planned,
designed, delivered and resourced. Any endeavour that requires collaboration
across the Commonwealth, state and territory governments on matters that would
potentially require changes or increases in their levels of resourcing do
require a significant degree of scrutiny within the budget processes of nine
jurisdictions. Accordingly, there are appropriate safeguards on the release of
unfinished, unapproved work. So it is not unusual for something that is in its
development stage within this governance context not to be made more broadly
available, particularly as it is subject to change. Whatever version they might
have been access at that point in time may not even have been the beta version;
it may have been an earlier version. Clearly, things have moved on.[23]
5.26
Although the Framework is being progressed towards completion, the
committee notes that there is limited publicly available information about this
fact. The committee gained information about the progress of the Framework
through its public hearing on 26 August 2015. The Department of Health's
website, which provides information about the Fourth National Mental Health
Plan, does not mention the Framework, its history or its current progress.
Information about Framework, which does not include its current status, is only
available through the National Library of Australia, Australian Government Web
Archive.
Outcomes focussed funding with reporting
5.27
It was the Commission's view that 'much of the funding from the
Commonwealth is neither particularly effective nor efficient.'[24]
Professor Fels told the committee:
Eighty-seven and a half per cent of the spending is downstream
on income support and crisis response, basically—the Disability Support
Pension, carer's payments, payments to states for hospitals, Medicare and
pharmaceutical benefits. So, much of the Commonwealth spending is for failure
to treat the problems early and cost effectively. It is payment for failure. We
have made recommendations about how that heavy expenditure could be reduced
with a much greater emphasis on and investment in prevention, early detection,
recovery for mental ill health and the prevention of suicide.[25]
5.28
Ms Jacqueline Crowe, a National Mental Health Commissioner observed that
without the proper identification of outcomes, and monitoring of those
outcomes, mental health funding could not properly benefit those with mental
ill-health:
...the key to all change initiatives is to ensure that change
means we do better—and we must do better for the people who are caring and our
families. To do this, Australia must consistently and rigorously be monitoring
and reporting publicly on outcomes. We do not currently do that well—and not
just outputs but outcomes for people, which includes human rights issues, the
effectiveness and quality of services, service system impacts, immigration,
performance and coordination, the reform process and, importantly, what people,
families and communities think of those systems.[26]
5.29
Ms Jaelea Skehan, the Director of the Hunter Institute of Mental Health
told the committee that a further impediment on the effectiveness of funding
for mental health was the current government funding being provided on a
year-by-year basis. Ms Skehan pointed out that this situation meant that early
intervention, prevention and health promotion was effectively de-prioritised:
...around funding, apart from the fact that prevention and
promotion is deprioritised compared to the more costly treatment ends of the
funding cycle,...I would really like to see some transparency about how funding
decisions are made, particularly in certain areas. We have seen a reduction in
funding in some areas and an increase in funding in others, and I am not sure
that there is a vision statement or a clear plan that makes it really clear to
the sector why certain priorities were made.[27]
5.30
Professor Hopwood, the President of the Royal Australian and New Zealand
College of Psychiatrists outlined a further funding and outcomes issue. He
argued that no future work could be planned without first setting in place
mechanisms for targeted research:
...a really important element of any development in the mental
health sphere is research to improve what we do. The risk that we continue to
do what we do because we do it will be obviated if we measure the outcome
better, but common sense says we would still like to improve on what we can do.
So the very best we can do at the minute still could do with a lot of
improvement. A significant commitment for research is an important factor—and
that includes funding we currently receive from organisations like the NHMRC
while a specific allocation from potential new funds like the medical research
fund would be something we would like to support.[28]
Policy and funding uncertainty
5.31
As mentioned briefly in Chapter 4, mental health policy and funding has
been 'on hold'[29]
since February 2014 when the Government tasked the Commission to review of
mental health services and programme delivery.
5.32
While the Government has deferred major policy decisions until after the
review was completed, and subsequently on completion of the outcome of the ERG
and COAG processes (paragraph 4.22 Chapter 4), recent Budgets have made cuts to
mental health service funding.
5.33
The 2014-15 Budget included a $53.8 million cut to the Partners in
Recovery programme. The Budget also introduced the $7 GP co-payment,
much-criticised for creating a barrier to those seeking to access primary
health care, including mental health care.[30]
5.34
The 2015-16 Budget included 'savings' of $962.8 million to be achieved
over five years by 'rationalising and streamlining' funding across the Flexible
Funds, which include funding for mental health, drug and alcohol dependency and
preventative health services and programmes.[31]
5.35
Minister Ley's April 2015 announcement of additional funding of
$300 million to mental health services has gone some way to temporarily
ameliorating the problem. However, as the funding extension is for a 12 month
period, it is at best a stop‑gap measure.[32]
5.36
The mental health sector is waiting for the Government response to the
Commission's recommendations for sector-wide reform. In the meantime, the
uncertainty about future direction and funding means that the sector is facing
a crisis.
5.37
In addition to the funding crisis, the mental health sector is waiting
to see how the government's response to the Commission's recommendations will
link with the transition of mental health programmes to the NDIS. The NDIS
transition will be examined in Chapter 7, while this section focuses on the
uncertainty caused by the delay in Government decision making.
5.38
Witnesses told the committee of the difficulties of operating services
and programmes in the current uncertain environment. Mr Ivan Frkovic, the Deputy
Chief Executive Officer, National Operations of Aftercare told the committee
that mental health service clients were greatly concerned about the
continuation of existing services:
People are really concerned that existing services, such as
Personal Helpers and Mentors and Partners in Recovery, which are helping them
to maintain lives in the community to some level and degree, will disappear... This
is creating uncertainty at the moment and increasing anxiety and levels of
relapse amongst people, because they do not know, as I think has been said. A
lot of these programs are due to finish in June next year: 'What happens beyond
June? Where do I go?' So, it is creating problems for the participants
themselves—the individual consumers—families and carers. They are saying, 'What
do we do in this situation?'[33]
5.39
Ms Ka Ki Ng,
Senior Policy Officer, Mental Health and Wellbeing Consumer Advisory Group
BEING, explained that from the point of view of consumers and carers, the uncertainty
around policy and funding may have resulted in service disruptions:
We want to particularly highlight some of the recent
proposals and changes that have happened that may have caused some disruptions
to mental health service provisions which have had a flow-on impact on mental
health consumers as well as family and carers. For example, we are aware that
at the moment there are a lot of uncertainties within the community or
non-government mental health services sector. We know that things like the national
review into mental health programs and services have caused a lot of anxiety in
the sector with rumours of our services potentially being defunded or having
their budget reduced or possibly being severely restructured.
We have heard that the transition from Medicare Locals to
Primary Health Networks has not been a particularly smooth transition in some
areas and has led to loss of services or at least disruptions. There are
funding uncertainties with regard to ATAPS, Partners in Recovery and also the NDIS
rollout—what services may be available to mental health consumers who are not
going to be eligible for the scheme. All of these are snowballing into a big
mass of uncertainty that is impacting on the wellbeing of the people working in
the sector as well the people that are actually trying to access support and
services.[34]
5.40
In particular Ms Ng observed that the change from the Medicare Locals to
the PHNs had resulted in loss of staff and relationships between consumers and
health care professionals:
For example, people not being referred on by GPs because GPs
are not sure where to go to, not knowing whether that particular Medicare Local
in their region is going to survive. There is also loss of staff. Often what we
have found in the mental health sector, and I would imagine it is the same in
many other human services sectors, is that relationships are built between
individuals. I may have a really good relationship with a particular staff
member in the Medicare Local and I may not know many other people beyond that
relationship, or I may not have a lot of trust—it is a particularly profound
relationship for consumers and carers. If there is such an uncertain
environment at a service, what has been pointed out is that if there is staff
turnover, then people will naturally try to find alternatives and those
relationships are lost. For a GP it might be a case of, 'Okay, let's find
another relationship', but for consumers and carers, it might actually mean
that they have to consider whether they want to make the effort to build a
relationship again, especially if there have been previous relationships where
it was negative. It can be really traumatic. I think people mentioned some of
those issues this morning. [35]
5.41
As discussed above, the government's response to the concerns of
the mental health sector about the uncertainty around mental health policy is a
12 month funding extension. The government is considering advice from the ERG,
and other processes, before it will make its response to the Commission's
recommendations.[36]
Committee view
5.42
As noted in Chapter 4, the government received the Commission's
completed review in early December 2014. The government then delayed releasing
the review until mid-April 2015, when forced to do so when parts of the
Commission's report were leaked. In October 2015, ten months after the
completion of the Commission's review, the government has still not responded
to the Commission's recommendations. As a result, the mental health sector struggles
with ongoing funding uncertainty and indecision about the future direction of mental
health policy in Australia.
5.43
The committee heard the concerns of mental health groups, advocates,
service providers, and consumers and carers in relation to the uncertain future
direction of mental health funding and policy. These groups all gave the
committee similar evidence: the government needs to respond positively to the
Commission's recommendations and it needs to do so before the end of 2015.
5.44
The Commission's review has been delivered at a strategic time for the
implementation of change in funding and governance of mental health policy. A
number of complementary processes are currently in play:
-
the Fourth National Mental Health Plan expired in 2014 and work
is beginning on the Fifth National Mental Health Plan;
-
according to the Department of Health, the National Mental Health
Service Planning Framework has approximately one year of development remaining
before it is ready for release; and
-
with the PHNs newly established in July 2015, witnesses argued that
a further 12 months is needed for PHNs to become fully operational and
connected in their regions.
5.45
The committee believes that by making a response to the Commission's
review now, the government will set the mental health policy agenda for the
foreseeable future and provide much needed certainty for mental health groups,
service providers, carers, and consumers.
5.46
The Minister for Health has stated that the $300 million extension of
funding for mental health services and programmes provided in April 2015 will
provide 12 months for the government to develop its response to the
Commission's findings.
5.47
To provide much needed clarity to the mental health sector, the
committee urges the government to conclude its deliberations by the end of
2015. Mental health service and programme providers, carers, and consumers, are
keenly awaiting the government's future policy direction. State and territory
governments also await the government's response for their planning of the
Fifth National Mental Health Plan. And all stakeholders, including the
Commission, are awaiting the release of the National Mental Health Services Planning
Framework.
Recommendation 1
5.48
The committee recommends that the government:
-
immediately publish the Expert Reference Group report;
-
urgently respond to the National Mental Health Commission's
review; and
-
guarantee funding for mental health groups and service providers
for the 12 months after the announcement of the government response to the National
Mental Health Commission's review.
Navigation: Previous Page | Contents | Next Page