Increasing survival rates for people with low survival rate cancers
5.1
This chapter discusses suggestions put to the committee intended to increase
survival rates for people with low survival rate (LSR) cancers. In particular,
this chapter considers:
-
the importance of early detection and diagnosis;
-
data and biobanking;
-
genomic medicine and biomarkers;
-
access to medicines;
-
care and support services for patients and their families; and
-
a national strategy on LSR cancers.
Early detection and diagnosis
5.2
The committee heard from a number of submitters and witnesses about the
correlation between early detection, screening and diagnosis, and increased
rates of survival for people with cancer.[1]
The committee also heard from people with LSR cancers, and their relatives,
about their desire for early detection of these cancers.[2]
5.3
Professor Guy Eslick spoke about positive developments for the majority
of cancers over the last 70 years due to early detection:
In the 1950s, the majority of cancers—that is about 75 per
cent of all cancers—had a five-year survival of about 50 per cent. Only half of
them were likely to live five years. Today most of these cancers have had
substantial improvements in their five-year survival. There are a number of
reasons for this improved survival, including increased research funding,
dedicated researchers, early detection and screening programs, education of the
public regarding risk factors that can be modified to reduce the risk and, of
course, newly developed treatments. However, there are a group of cancers where
the survival rates have not changed much at all in the last 70 years, and this
is unacceptable.[3]
5.4
Professor Eslick therefore advocated that the Australian government
should focus 'on identifying risk factors, prevention and screening programs
for low-survival cancers'.[4]
5.5
The positive effect of early detection was also discussed by
Dr Nicola Waddell, who informed the committee that early detection of
pancreatic cancer—a LSR cancer that is 'increasing among young females'[5]—would
'mean a larger proportion of patients can undergo surgery',[6]
which could lead to an increased chance of survival for these patients.
5.6
In relation to the improvements in breast cancer survival rates,
Mr Richard Vines of Rare Cancers Australia (RCA) observed that since
1990, the survival rate has increased from 60 per cent to 90 per cent due to
screening, and commented that '[e]arly diagnosis is everything'.[7]
Mr Vines also spoke about the importance of public awareness and its role in early
detection:
...how do you tell the public that if they have a pain that
does not go away that they should not just take two aspirin in perpetuity but
that they should do something about it? Virtually every patient who comes to us
has been three or four months in the diagnosis. That is critical because that
is the time when the cancer is likely to metastasise. For example, breast
cancer patients with metastatic cancers do not do well; you want to understand
it early.[8]
5.7
Mr Daniel Goulburn of the Pancreatic Cancer Alliance similarly spoke to
the high rates of survival for breast cancer, as well as prostate and colon
cancer, and how this correlates with early detection as well as public
awareness programs.[9]
Mr Goulburn noted that 'there is a general awareness amongst the general
public and good education of frontline medical practitioners' of such cancers
when compared with pancreatic cancer, which currently has a survival rate of
7.7 per cent: a marginal improvement over the last 30 years.[10]
5.8
Other witnesses also raised the lack of awareness of LSR cancers amongst
GPs, which hinders early detection and diagnosis. For example:
CHAIR: ...I want to ask you how you feel awareness is
amongst GPs and other medical practitioners. Do you feel there should be an
awareness campaign for them?
Mrs Shonk: It is really low. My brother was told up on
the Gold Coast that he had a tropical disease even after having [Magnetic
Resonance Imaging (MRI)]. When he brought the scan down to Sydney, I looked at
it and went, 'That's a brain tumour.' The knowledge with GPs is very limited.
My brother-in-law got sent off to the ear, nose and throat specialist. They
kind of think about a brain tumour as the absolute last resort, which is kind
of unfortunate because time is of the essence. I think it is incredibly poor.
Mr Shonk: They do not come across it enough to know
what to do.
Ms Ferguson: When Leanne first presented herself to
the doctor, they did not even take her blood pressure. They just gave her a
doctor's certificate—gave her two in case her headache had not cleared up by
the next day. In the scheme of things for GBM, a few days is not going to make
the difference, but for other cancers, where people are waiting for many months
to get a diagnosis, it is almost criminal.[11]
5.9
Professor Terrance Johns of the Brain Cancer Discovery Collaborative (BCDC)
remarked:
That is the problem with a rare disease. It is not only that
it is rare and so a lot of the GPs would not necessarily see it very often. The
other thing is that patients die so quickly and so they are not continually visiting
GPs. A GP might see one patient every five years but then that patient is dead,
and so there is no follow-up; there is no corporate memory there. I think that
is part of the problem.[12]
5.10
Professor Phyllis Butow, President of the Clinical Oncology Society of
Australia (COSA), similarly discussed the need for improved detection and
diagnosis of LSR cancers, stating:
This inquiry will hear a lot about laboratory research, as it
should, but we could also do a lot to improve cure rates by simply identifying
cancers earlier and treating them more efficiently. To do this we need to
understand the blockages in our health system that prevent those things
occurring. Rare cancers are particularly at risk of being discovered late
because their symptoms are often vague, patients do not know when or how to
report them, and GPs are often not very familiar with rare cancers or their
symptoms and send patients off in different directions to get different sorts
of investigations, because they are not expecting a rare cancer. Patients often
say to us that they have been reporting symptoms for some time before they are
diagnosed, and they find it difficult to know where to go for expertise and
they find it difficult to be reassured that they are on a tried and true
pathway for care.[13]
5.11
To address low awareness amongst GPs and improve detection and
diagnosis, COSA proposed a number of recommendations:
To improve this, we think there are a number of strategies
that might help, requiring health services research. For example, in England
and Denmark they have achieved a lot by getting health services to really focus
on where the blockages are by setting targets for time to diagnosis after presentation
of symptoms and time to treatment after diagnosis, and making the report of
achievements against those targets public. This has worked to reduce time
frames and get people to care more quickly, but we need to understand what
appropriate targets are in the Australian context and how we can accurately
measure those time frames. Another opportunity is to implement optimal care
pathways, which have been developed by Cancer Council Victoria and endorsed by
the National Cancer Expert Reference Group, NCERG. These describe key steps in
a cancer patient's journey and the optimal care the patient should receive at
each of those steps. We know there is variability in different jurisdictions in
the pathway that patients follow, and if we were able to really enforce or
encourage uptake of the OCPs we are likely to improve care significantly and
reduce some of the disparities that Karen has been discussing. We need to
develop implementation strategies to overcome the barriers to implementing
those care pathways in different jurisdictions.
We think that a demonstration project of rapid referral
clinics may be helpful in this space. For example, we might take a set of
symptoms such as abdominal symptoms, which are often the site where rare
cancers occur, and have a one-point referral system, where GPs can refer
patients with those sorts of symptoms to a clinic personed by GPs who have a
particular interest in cancer and who would make sure the possibilities of a
cancer are ruled out for those patients, with triaging out to specialists, if
that is required. Those GPs would have a very well developed network of
specialists to refer out to.[14]
5.12
Cancer Australia informed the committee about the work it does to increase
awareness amongst GPs by providing 'evidence-based information, resources and
data across the cancer care continuum—so, across a range of cancer types, which
obviously does include low survival and low incidence cancers'.[15]
Cancer Australia explained:
We use a range of channels and platforms to present this
information and to raise awareness. The Cancer Australia website would be the
main one, but also through media releases, media interviews, and through
various social media platforms.
If I could give you a couple of examples of our work in
raising awareness, with particular relevance to low survival cancers. In our
work in Ovarian Cancer Awareness Month in February this year, we developed a
range of resources for consumers and GPs, with a particular focus on symptom
awareness—I think, Senator, you alluded to the challenges that sometimes
symptoms can be quite nondescript and fairly common—so there's an important
piece of work around raising awareness in the community about what the symptoms
are. But also, particularly in the ovarian cancer space, raising awareness for
GPs on the importance of the assessment of family history, and also appropriate
referrals for ovarian cancer patients. This information was delivered through
our Cancer Australia website and through social media channels. The campaign
resulted in a 10-fold increase in traffic to the website. So the message is,
hopefully, getting out there.
Another example in another low survival cancer is in lung
cancer. We have done some work in this space. We developed a video animation,
What Your Cough Is Telling You, again working in that important space of
raising awareness of symptoms and encouraging members of the public to be aware
of what to look out for in lung cancer, and the importance of early
investigation of lung cancer symptoms. There are also links on the website to
risk factors, to understanding diagnosis and treatment and also for finding
support. Again, with this campaign in lung cancer we have seen significant
increases in traffic to the website to access this information.[16]
5.13
Cancer Australia also outlined work it undertakes more directly with
medical professionals. For example, Cancer Australia convenes 'an
intercollegiate advisory group' comprising representatives of the medical
colleges and consumers, and which meets twice each year. Through the advisory
group and:
also through a similar mechanism, which is a high-level
research and data advisory group, which also meets twice a year, we're able to
bring together people who are both working at the coalface and also are
policy-makers and health planners and also experts in cancer.
We also work directly with a number of agencies that have
mechanisms for accessing GP offices directly. For example, we place messages on
the television screens in the GP clinic, and there are a number of
point-of-care mechanisms also. Cancer Australia doesn't develop all of them by
any means, but there are point-of-care mechanisms whereby the general
practitioner in his clinic is able to access relevant information related to
patient care.
At Cancer Australia we seek to promote and widely disseminate
information that may be of relevance at the community level and at the health
professional level. We have the Supporting People With Cancer Grant Initiative,
where we work with local communities. We fund them to potentially raise
awareness or to provide supportive care to their communities.[17]
5.14
By way of international comparison, the committee heard from The Brain
Tumour Charity (TBTC) in the United Kingdom (UK) about its HeadSmart campaign:
HeadSmart is a campaign that we launched with the University
of Nottingham and the Royal College of Paediatrics and Child Health. It's an
information campaign...It's about giving parents, carers and also GPs more
information about the signs and symptoms of brain tumour in the paediatric
population. It's split into three different groups: under-five year-olds, five-
to 11-year-olds and 12- to 18-year-olds, as the symptoms can be different. But
because the symptoms are very common, it's actually a combination of the
symptoms that are the trigger for the referral pathway which was developed by
the University of Nottingham under our funding in 2011.[18]
5.15
The HeadSmart campaign has reduced the delay in diagnosis for children
with brain cancer from 14.4 to 6.5 weeks;[19]
which is still higher than the five week detection period in the US and Poland.[20]
Dr David Jenkinson, Chief Scientific Officer of TBTC explained why
the UK's detection rates have reduced so dramatically:
The information given to the carers and parents—often through
schools or through nurseries and places like that—is what is really driving the
diagnosis. What we are finding, though, is that the teenage group—the 12 to
18s—aren't really getting as good an outcome as the other groups. So the
current delay for the 12 to 18 group is 10.3 weeks, whereas with babies it's
4.1 weeks. Obviously, some work needs to be done in that space, which is why
the campaign was relaunched with different animations and different graphics as
well, hopefully to appeal more to that teenage audience.[21]
5.16
Dr Jenkinson elaborated on how the campaign engages with GPs, while
noting that attendance by GPs at 'healthcare professional sessions or days'
'would be less than one per cent':
A lot of the HeadSmart campaigning is done by a number of
volunteer advocates—often people who have been through the situation themselves
and have benefited from the HeadSmart campaign. They have found it on our
website and then actually gone to their GP with the information to hand. Or
there are those who would have benefited had they found it. They are often the
best advocates for us to go out there and work with the healthcare
professionals, the schools and places like that. We understand that GPs are
very busy and that, therefore, another leaflet may not be the best way to
educate them.[22]
Committee view
5.17
There is no doubt that early detection of cancer significantly improves
outcomes and survival rates for patients. Significant improvements have been
made to the survival rates for cancers such as breast, prostate and colon as a
result of widespread public education campaigns and the availability of tests
to aide early diagnosis. The public visibility of these cancers, together with
the number of Australians affected and survivors who become advocates, mean
that these cancers then tend to attract charitable and philanthropic support,
and the majority of funding for research. These cancers are also more likely to
be front of mind when a patient presents to their GP.
5.18
As evidence to this inquiry has demonstrated, the rarity of LSR cancers
means that GPs infrequently encounter them and this, coupled with often vague
symptoms, means that these cancers are not detected and diagnosed quickly. It
is obvious to the committee, therefore, that awareness amongst the public and
GPs must be improved so that patients seek medical attention and GPs
contemplate LSR cancers as a cause sooner than they do currently.
5.19
The committee is impressed by the HeadSmart campaign and the in-roads it
has made in reducing the time taken to detect and diagnose brain cancer in
babies and young children in the UK. In addition to the valuable work Cancer
Australia is already undertaking in this space, the committee is of the view
that the Australian government should do more to raise awareness about LSR
cancers among the public. The committee recommends that the Australian
government develops and implements an education and awareness campaign based on
the UK HeadSmart model to inform the public about LSR cancers and their
symptoms, with a view to reducing the time taken to detect and diagnose these
cancers.
Recommendation 9
5.20
The committee recommends that the Australian government undertakes
communication activities targeted at the public with the objective of reducing
the amount of time taken to detect and diagnose low survival rate cancers.
5.21
The committee also urges the federal, state and territory governments to
consider the proposals made by COSA, and the role that optimal care pathways
(OCPs) and rapid referral clinics could play in improving detection and
diagnosis of LSR cancers.
5.22
In order to maintain their registration, doctors in Australia are
required to undertake ongoing education and professional development,
recognition that '[t]he practice of medicine is a constantly evolving field'
and so that doctors 'maintain and further develop their knowledge and
expertise'.[23]
Certain elements of this ongoing training are compulsory (for example
cardio-pulmonary resuscitation (CPR)) while others allow 'general practitioners
(GPs) to self-identify priority areas of general practice learning needs in accordance
with their personal, patients and community needs'.[24]
Continuing professional development (CPD) offered by the Royal Australian
College of General Practitioners (RACGP), for example, includes courses in
vaccination, sexually transmitted infections (STIs), skin cancer, addiction,
clinical emergency management, and managing complex pain.
5.23
The committee considers that detection and diagnosis of LSR cancers
could form part of this CPD. The committee appreciates that the rarity of LSR
cancers means they infrequently present to GPs; however, GPs play a vital role
as often the first point of medical contact for a patient with an undiagnosed
LSR cancer and it is essential that GPs are sufficiently skilled to identify a
LSR cancer as a possible diagnosis early.
5.24
The committee therefore recommends that the Australian government works
in collaboration with the medical profession via the RACGP and Australian
Medical Association to improve awareness of LSR cancers amongst GPs, including through
CPD.
Recommendation 10
5.25
The committee recommends that the Australian government works in
collaboration with the Royal Australian College of General Practitioners and
the Australian Medical Association to improve awareness of low survival rate cancers
amongst general practitioners, including through continuing professional
development.
Data
5.26
Data collection and population level information about cancer in
Australia impacts on research undertaken into LSR cancers. The committee heard
that data collections on LSR cancers in Australia are not as good as they could
be, and received a number of suggestions about improvements that could be made in
this respect.
5.27
Cancer is a notifiable disease in Australia, such that all state and
territory registers are statutorily required to disclose information about
cancer to the Australian Institute of Health and Welfare (AIHW).[25]
This data is compiled in the Australian Cancer Database:
...which is a database of all new incident cases of malignant
cancers since 1982. It is all cancers not including non-melanoma skin cancer.
So we already have detailed data on all new cases of cancer. That covers the
number of people who have the cancers. We are also able to bring in information
on the deaths from those cancers and can do extensive analysis, including
survival analysis, for people with various types of cancer. So there is
detailed data there. If there is further information that is required, that
could always be looked at to see if that could be included in some form.[26]
5.28
However, the committee heard that the Australian Cancer Database only
contains data within 'a defined scope', and consequently, data required by a
researcher may not be available through this database.[27]
For example, the AIHW noted that it has data available 'on non-malignant
tumours of the brain (and other parts of the central nervous system) for those
diagnosed at any age' but only from Victoria, Queensland, Western Australia and
Tasmania, and the Australian Paediatric Cancer Registry—a national cancer
registry that specialises in data on cancer in children—contains 'diagnosis
data from all jurisdictions, but only for those ages under 15 at the time of diagnosis'.[28]
5.29
Mrs Tricia Berman of the Brain Tumour Alliance Australia (BTAA) opined
that Australia 'cannot afford' this approach anymore, noting that 'countries
such as the US, Canada and the UK register all [brain tumours], so that is
helping, in terms of analysing that data as a researcher, to see what options
are available for future treatments'.[29]
Further, Mr Philip Steel of BTAA stated that even though it is known that there
are 1600 malignant brain tumours recorded in Australia per year, 'we do not really
have any idea about how many benign brain tumours there would be, and there is
really no way to gather that information'.[30]
5.30
The CSIRO noted that much of the data collected by the AIHW had, until
now, been administrative in nature, which required 'researchers to infer
clinical utility from the data'.[31]
However, the CSIRO considered that the current capturing of clinical data in
the Electronic Medical Record and Electronic Health Record means 'that more
clinical data is being captured, which if made available, would greatly
increase the ability of Australia’s medical research community'.[32]
5.31
The CSIRO explained the significance of such data:
Registries are an important part of Australia’s health data
landscape. At a state level, health jurisdictions are required to maintain
various registries for public health, such as state based cancer registries. In
addition, various clinical groups have developed disease specific registries,
such as the trauma registry or prostate registry. In the case of mandated
registries these typically contain a minimum data set and it is a legal
requirement to submit this information. In the case of clinical registries,
these are typically more detailed but are not mandated and will not capture all
cases in Australia.
The linking of data from different data collections to these
registries can add significant value. In the case of the cancer registries, the
linking of treatment and outcome data provides a more useful set of data for
clinical research.[33]
5.32
Professor Eslick argued that people with LSR cancers need to be asked about
their lifestyle and that this information must be recorded, as the cause of
many cancers, such as pancreatic cancer, is not understood and evidence is
needed in order to prevent and treat them:
Until you identify what causes them, you cannot prevent them
and you certainly cannot treat them....You get information, but you need to be
conducting large, prospective studies on people and asking them nitty-gritty
questions about: 'What do you think caused your cancer? What has your work been
like? What do you eat on a daily basis?' I believe that the majority, probably
98 per cent of cancers, are due to environmental factors, and the remainder are
probably due to genetic factors. Some of those environmental factors may switch
genes on and off. I think, primarily, unless you can identify these factors, we
are sitting in a position where these gentlemen are correct: in 100 years,
survival rates for these low‑survival cancers have not changed. It is a
disgrace. As a researcher, you get a bit shirty when you see all this funding
going to breast cancer and colon cancer and other cancers that now have really
good survival rates. You think, 'What about the rest?' I think it is time for a
change.[34]
5.33
The Cancer Council Australia (CCA) and COSA raised concerns about the
accessibility of research data due to articles being 'hidden behind paywalls'
as well as 'delayed release [of research data] by long embargo periods'.[35]
5.34
However, the committee was also told that 'there can be a significant
administrative burden in the data sharing'.[36]
The Cancer Council Victoria (CCV) stated that:
...what researchers are wanting to do is prioritise those
high-value collaborations with institutions that have the capability and capacity
to do that. I think there is undoubtedly that appetite. We see in our
organisation, and I am sure in Karen's as well, the existence of collaborative
institutions coming together with combined research applications to our
organisation, and I am sure others, including [the National Health and Medical
Research Council (NHMRC)] as well. I think the appetite is certainly there.[37]
5.35
In light of the difficulties with sharing research data, the CCA and
COSA suggested that the Australian government could 'show leadership' by:
...ensuring that all federal government departments and
agencies, as well as cancer research centers [sic], and universities, that fund
cancer research are required to adopt and implement open access policies that
require knowledge to be openly licensed and freely-available without
restrictions or embargoes.[38]
A national biobank
5.36
A biobank is a facility that collects and stores 'various clinical
samples, such as blood and tissue from consenting patients for use in medical
research'.[39]
Biobanks are 'widely recognised as valuable resources for biomedical research'
and can improve 'the prevention, diagnosis, treatment and ongoing management of
diseases, including cancer'.[40]
A range of submitters and witnesses therefore advocated for a national biobank,
particularly for brain cancer.
5.37
The Queensland Brain Institute (QBI) explained the importance of
cancerous tissue in oncology research:
Senator BUSHBY: Coming back to the tumour tissue, you
talk about how valuable it is and about keeping it for research purposes. We
also heard earlier that there have fairly recently, I think, been full DNA
profiles on tumours.
Prof. Richards: Yes.
Senator BUSHBY: If you do a full DNA profile of a
tumour, is that all the information you need, or are there still advantages in
keeping the tissue for other purposes? Just take us through that.
Dr Bunt: You want as much tissue as possible which is
not necessary for the standard care. Whatever the pathologist does not need is
really a source of important information. There are different kinds of tissue preservation
methods. We have the pathological tissue, in paraffin, which you can use for
looking at the morphology of cells. Indeed, recently people have done a lot of
profiling of the DNA, which has changed our whole view about tumours that we
thought were just one tumour type; they are actually two or sometimes three
different tumour types, or just one but representing differently. We also—and
you see that in a lot of big laboratories around the world—want viable tissue,
tissue which is still alive.
Prof. Richards: Removed from the brain.
Dr Bunt: Yes, because we can use it for xenografting
models. That is when you take the tumour and transplant it to a mouse so you
can use it for either basic research on understanding how this tumour behaves
or drug testing—preferably, in the long term, maybe even models where you can
test drugs for a patient on a mouse model with the same tumour. If the patient
then has a recurrence, we know what drugs might help. So there are multiple
levels there.
But what you see is that the groups that really changed the
landscape in our understanding of brain tumours are big groups, and they are
collaborating. You need a lot of material from different tumours to really make
a difference. Because they are so different, you need at least hundreds of the
tumours to really find what they have in common and what makes them become the
tumour they are. So that is very important, and you see that countries that
have a longstanding culture of archiving and preserving this kind of material
now have an advantage, because they have this material ready to go and a lot of
information about the outcome for the patient.[41]
5.38
Professor Linda Richards of the QBI explained that brain cancer researchers
require both biological and non‑biological data:
We need research that is done by physicists and also
mathematicians who are applying algorithms to try to understand how tumours are
able to progress and invade the tissue around them'.[42]
5.39
The QBI therefore recommended 'the establishment of a central brain
tumour tissue bank' which would provide 'timely access to the tissue needed to
develop tumour models'.[43]
5.40
The Cure Brain Cancer Foundation (CBCF) also supported 'national
bio-banking and registry linkages', stating that '[s]tate governments are
creating impressive data linkages within their states that have the potential
to transform research and care' and that:
The Australian Government is well placed to facilitate the
integration of these resources through initiatives, such as the [Coalition of
Australian Governments (COAG)] National Cancer Work Plan, so that the national
capacity is greater than its parts and to create a truly international
competitive research environment with the highest levels of patient care.[44]
5.41
Dr Bryan Day, Team Head, Translational Brain Cancer Research Laboratory
at the QIMR Berghofer Medical Research Institute (QIMR Berghofer) and Professor
David Walker described current collection of brain tumour tissue as 'ad hoc'.[45]
This is because there are a number of complexities around the collection of
human tissue, including the way it is used and stored, issues of ethics and
consent, and other patient information gathered.
5.42
Dr Jens Bunt of the QBI explained, in relation to the
collection of tissue:
...there is a lot of tissue which is lost in certain steps,
because we have a lot of different hospitals, both private and public, a lot of
different pathologists and a lot of different neurosurgeons and because there
isn't the awareness that we can use this for basic research. Sometimes it is
lost because it is not stored in the right way or the pathologist releases the
additional material a little bit too late for us. In our case, because we
really want to xenograft it, there is a time limit. We would like it
straightaway from the surgeon—within 15 minutes into a mouse.[46]
5.43
Related to the collection of tissue, Professor Michael Buckland and Professor Manuel
Graeber discussed neuropathology, in the context of diagnosis of and research
into brain tumours. Professor Buckland remarked that:
Brain Cancer Biobanking Australia...is trying to coordinate
brain cancer tissue banks across the country to create a single large virtual biobank
to get the sorts of numbers we need for proper studies. I do note that the National
Research Infrastructure Roadmap which was recently produced by the federal
government did indicate that networked biobanking was a research priority for
the government.
I would also like to emphasise the role—the often forgotten
role—of pathology and pathological diagnosis in the treatment of these tumours...In
many cases, the role of the pathologist is often overlooked. I think, particularly
with the government funding models, the role of the pathologist is not
supported. I would point out that many of the tests we are now required to do
to comply with the latest WHO classification of brain tumours are not Medicare
rebatable, so either we have to absorb the costs, the referring doctors absorb
the costs or the patients have to pay out of their pockets. In Sydney, many of
the large departments will absorb those costs, so we will charge back to the
referring hospital. However, I am concerned that in rural and disadvantaged
areas there is not that sort of money, so patients are asked to pay and they
baulk, and so in fact their diagnosis may not be adequate.
I would put it to you that for any decent treatment you need
to know what you are dealing with, and that is the role of the pathologist.
Just the other week a large multi-institutional study from the United States
was published on the pathological diagnosis of brain tumours. They examined
1,500 brain tumours and identified a serious error or misdiagnosis rate of
close to five per cent when tumours were diagnosed at a local institution.[47]
5.44
Professor Graeber was similarly strident is his support for
neuropathology and emphasised its vitally important role in cancer research:
People have to have training in neurology and psychiatry—in
the brain sciences—in addition to what they do in pathology. You cannot become
a properly trained, if you apply international standards, neuropathologist
easily except when you make special efforts—like [Professor Michael Buckland].
He keeps travelling and attending international courses. I commend his effort
to raise that little flag of the neuropath department. I strongly support that.
It is the best thing you can do for brain tumour research and also neuroimaging
dementia research in this country. We need proper neuropathology. There are so
few hands that look at the brain's hardware...[48]
5.45
Professor Richards of the QBI discussed time delays arising from ethics
approval processes, highlighting that '[h]uman ethics is obviously crucially
important' but also that:
I think every tumour patient would want their tumour tissue
which is being removed to be used for research purposes. I think that it would
be more beneficial to have an opt-out process whereby the patient, if they
decided they did not want to have their tissue used for research, would opt out
rather than having to opt in, because that is just an extra step of consent
that has to go through.
In general, I would say the human ethics is a very, very long
process to get approved at the moment. We have the ability to perhaps share
with the groups in Europe or in the US, but we would have to de-identify that information.
But the ethics of trying to get the ability to even share the de-identified
data is very complex, especially at an international level, let alone at a
national level. I am not kidding. It can take a year, 18 months, to get one
ethics approval at the moment.
Senator BURSTON: Could it be part of the consent form
for an operation?
Prof. Richards: It should be. It really should be. But
here, again, we need the buy-in of the clinicians. We desperately need the full
buy-in of the clinicians. We have had some supportive clinicians in Brisbane,
who made it opt out rather than opt in, and that helped a lot.[49]
5.46
The committee heard that tissue collection cannot occur in isolation,
and that information about each patient from whom a tissue sample is collected is
essential. Dr Nicola Waddell, Group Leader, Medical Genomics Group at the
QIMR Berghofer emphasised that in order:
...for tissue banking to work, you need to enrich the samples
with clinical information. You need to be able to continually follow up the patients,
see how they have progressed, and find out what treatment they received and how
well they did, because that will inform the samples and the research that is
being done on the samples too.[50]
5.47
Wesley Medical Research told the committee that '[w]ithout data, the
samples are worth nothing' and that there must be relationships and networks
between clinicians, pathologists and researchers so that researchers are:
...able to go back to the clinician and know when they have had
extra testing done—or where the sample has come back and it is a different type
of tumour, or they have got a recurrence, the surgeons will ring me and say:
'This patient's coming back in next week. Can you collect?'[51]
5.48
Some submitters and witnesses also discussed logistical, regulatory and
cost implications. The CCA and COSA discussed the current fragmentation of
biobanks in Australia, describing the sector as:
...poorly regulated and lags well behind many other countries.
Specifically, a current lack of biobank oversight means that the numbers of
biobanks that currently exist in Australia, how most of these biobanks operate,
and whether they are effectively supporting Australian research by performing
at internationally-accepted standards, is not known.[52]
5.49
The QBI similarly described the fragmented nature of Australian biobanks
and their differing objectives:
Already there are multiple tissue banks currently in
Australia with different goals and different ways—what kind of material they
have and do—so the start is already there, but you have to have local nodes. It
would be good when there is just one consensus, both from the researchers and
the clinicians, about a concept, so everybody is aware that a clinician cannot
say, 'I didn't know that I could provide this tumour,' because it is a standard
concept within the clinical environment.[53]
5.50
The QBI and Wesley Medical Research commented on the costs of
establishing and maintaining a biobank. Professor Richards explained:
There is no doubt that a national tissue bank would really help
a lot. It will be expensive. Obviously, you need a person there at midnight or
whenever the surgical procedure is going on. You literally need somebody there
holding the tube while the neurosurgeon removes the tumour and then bringing it
back to the bank, processing it and making sure it gets to us as fast as
possible so we can then put it into culture or put it into a mouse or whatever.
It is not easy. It is complicated to set up a tissue bank.[54]
5.51
Ms Emma Raymond, Theme Leader, Cancer, Wesley Medical Research went on
to discuss the financial cost associated with implementing a standardised
procedure to collect tissue samples and data from all patients, stating that:
If the money was not an issue and we did it blanket across
every type of tumour, or all the rare types of tumours, and things like that, I
think that it would provide a resource for researchers that could be amazing
long-term. It is just that every time I have seen someone try to do that, they
will get funding for one year or two years or five years, and at the end of it,
they have not had enough time to then provide those samples to the researchers,
or they have to shut the doors and then what do they do with the samples?
There needs to be a look at, if we are going to do something
to the level, a commitment for 20, 30 years at least with the infrastructure
built in. You need to have buy-in from the public and private sectors, and that
is where it gets difficult. So in the private sector, I can physically go into
theatre and stand there and collect the sample, but in the public sector it
will not work that way.[55]
5.52
Ms Raymond also spoke to accessing the Brain Bank at the University of
Queensland (UQ) and the cost of storing brain tissue samples:
...the problem is the samples that they have stored [at UQ] are
half-brains from motor neuron disease, Parkinson's disease and things like
that. To store their samples would cost us approximately $50,000 a year just in
electricity. If there were a large resource, it would be great to bring in the
little ones like that and provide them to researchers. There is one case over
there where four members of the same family all have different types of
dementia. Those sorts of samples would be so useful to researchers, but like I
said, the actual money involved to bring all those samples across would be a
lot.[56]
5.53
Professor Richards suggested that tissue collection and participation in
research by clinicians and doctors could be improved by making 'a Medicare
rebate contingent upon them providing the tissue':[57]
...we need an increased awareness of the importance of research
in the clinical setting. Hospitals should be made aware of how important it is
to have research trained doctors leading their clinical groups. Obviously we
need doctors that also focus only on patient care, but the heads of
departments, for example, should be trained in research so that they can make
sure that that department also contributes to the research effort to cure that
disease, no matter what disease it is, not just treat the patient. That is of
the utmost importance—I do not want to undermine that at all—but we should be
in the process of preventing disease, preventing these tumours from ever
happening, and we need to understand why they occur in order for that to
happen. It is trying to involve our hospitals somehow. I was not kidding when I
said maybe you need to look at the Medicare rebate and whether or not you
actually tie that to the hospital, embedding research in that setting.[58]
Committee view
5.54
The committee notes that the Australian government is undertaking some
initiatives with respect to data collection. For example, through Cancer
Australia, the government:
...is undertaking an initiative which aims to strengthen
national data capacity through the collection, transfer, collation and the
reporting of standardised national data on stage, treatment and recurrence
(STaR) for all cancers.[59]
5.55
Importantly, the initiative 'is being undertaken in collaboration with
relevant Australian Government departments and agencies, and state and territory
governments and their population-based cancer registries'; and, according to
the government, 'will address the lack of national data on the severity of
cancer at diagnosis, which treatments are applied, and the recurrence of cancer
after treatment'.[60]
5.56
The committee welcomes this important initiative and urges the
Australian government to implement it as a priority, given how important
clinical and population level data are to medical research. The committee reiterates
the importance of Australian cancer data collections being complete and, aided
by technological improvements in both data collection, management and analysis,
the committee recommends that the Australian Cancer Database is expanded to
capture all cancers, including benign tumours of the brain and other parts of
the central nervous system.
5.57
In doing so, and acknowledging consultation already underway with
federal departments and agencies as well as state and territory governments,
the committee also recommends that the Australian government consults with
medical researchers to identify what data (for example, clinical and lifestyle)
data must be included so that the Australian Cancer Database is a valuable and
useful resource to them.
5.58
The committee also recognises that expanding the data set collected will
require the consent and cooperation of patients and clinicians. The Australian
government must collaborate with its state and territory counterparts to
address current barriers to data collection, and consider ways in which data
collection can be mandated, standardised and streamlined across Australia, in
both public and private health settings.
Recommendation 11
5.59
The committee recommends that the Australian government, in
collaboration with state and territory governments:
-
considers expanding the Australian Cancer Database to capture all
cancers, including benign tumours of the brain and other parts of the central
nervous system;
-
in so doing, consults with medical researchers to identify what
clinical and lifestyle data might be included in order to benefit oncology
research; and
-
addresses current barriers to data collection and considers ways
in which data collection can be improved across Australia, in both public and
private health settings.
5.60
The committee welcomes the acknowledgement of networked biobanks as a
priority area in the 2016 National Research Infrastructure Roadmap.[61]
The Roadmap states that:
Biobanks are enablers across a range of medical, agricultural
and biodiversity research. Integrating existing tissue and environmental
biobanks into collaborative networks linked to the research community, ensuring
the ability to collect, store and analyse high quality useful research data
will provide significant improvement in research effectiveness.
Linking established biobanks into a national network of
central tissue repositories will turn an under-utilised product into a more
valuable research resource. Under a national system for collecting and
biobanking human tissue samples, standards for data gathering and sample
curation would assist in the sharing of materials and would foster
collaborations. Inclusion of genomics, proteomics and metabolomics data with health,
lifestyle and clinical data, will magnify our ability to develop new
diagnostics and therapies.
While the necessary institutional processes are in place in
the network of natural history museums, herbaria and seedbanks, medical
biobanking is fragmented. Australia would also benefit from a population
biobank. A population biobank has unique value for population genomics and
research into the causes, prevention and treatment of disease. Other countries
have well established population biobanks that provide infrastructure for
public health research...We should explore building on existing capabilities to
move towards a national biobank network.[62]
5.61
The committee fully endorses this position and urges the Australian
government to give serious consideration to implementing a national networked
medical and population biobank that includes tumour samples and relevant
clinical and lifestyle data associated with each tumour sample.
Recommendation 12
5.62
The committee recommends that the Australian government gives
serious consideration to implementing a national network medical and population
biobank that includes tumour samples and relevant clinical and lifestyle data
associated with each tumour sample.
Genomic medicine and biomarkers
5.63
Advances in genomic medicine and molecular biology, particularly the
identification of biomarkers, are paving the way for 'personalised medicine'
and immunotherapy.
5.64
Genomics is the study of the genome; genomic medicine is the medical
discipline that uses and applies genomic information to a clinical setting,
such as managing a patient's condition or disease, and informing decisions
about their care. In cancer genomic medicine, genetic testing may be able to
identify the type of cancer, the heritable risk for a cancer, or a targeted
treatment of a cancer.[63]
5.65
A biomarker is a naturally occurring molecule found in blood, other body
fluid or body tissue that can be a sign of an abnormal process or of a
condition or disease. A biomarker may also be used to determine how well the
body responds to a particular treatment.[64]
5.66
The Garvan Institute of Medical Research/Kinghorn Cancer Centre/Garvan
Research Foundation (the Garvan Institute) explained the significance of
genomics to personalised medicine, and the positive impact this form of treatment
has on increasing survival rates for LSR cancers:
The genome is the complete set of genetic information we
inherit from our parents, and which determines every aspect of health and
susceptibility to disease. Genomic research has given us a new understanding of
the interplay within the genes, throughout our whole genetic landscape.
...
Precision or personalised medicine is the future for all
cancer treatment, but will have its greatest impact for ‘rare’, high-mortality
cancers. Genomics is essential to precision medicine. More funding is needed
for clinical research that brings the potential of genomic medicine to the
challenge of ‘rare’ and lethal cancers.[65]
5.67
The benefits of genomic research for advances in ovarian cancer was outlined
by Ovarian Cancer Australia:
...as we have progressed in genomics, we know that ovarian
cancer is not just one disease; it is a group of different types of cancer,
each with different cellular appearances and each with different molecular
characteristics and different trajectories. New evidence, for example, has
revealed that 50 per cent of ovarian cancer comes, in fact, from the fallopian
tube and then spreads to the ovaries.[66]
5.68
Professor David Thomas, Head of Cancer Research at the Garvan Institute,
discussed the work of he and his colleagues at the Kinghorn Cancer Centre who
have developed a Genomic Cancer Medicine Program (GCMP) that 'focuses on "rare"
cancers'[67]
with the goal of improving cancer outcomes for people with these diseases. The
program:
...brings together researchers and clinicians to translate
research findings into the clinic. The program utilises the sequencing capacity
of the Garvan Institute of Medical Research to identify more effective
treatments for cancer patients, as well as to understand and exploit heritable
cancer risk.[68]
5.69
The GCMP's Molecular Screening and Therapeutics (MoST) study 'offers,
within the research context, molecular profiling of tumours for patients with
"rare" cancers and links this to relevant experimental and standard
treatments':
MoST squarely addresses the challenges of engaging
individuals with less common cancers in clinical research, taking advantage of
the principles of precision medicine. Eligibility for participation in clinical
trials available as part of MoST is completely independent of the 150-year old
classifications that arbitrarily divide cancers according to where they arise
in the body. Once a cancer has spread, its site of origin is less important for
patients than understanding what makes the cancer ‘tick'. MoST trials
personalise experimental treatment based on an individual’s unique personal and
cancer genetic profile, and in so doing neutralise the disadvantage of
‘rarity’. MoST offers a new kind of clinical trial of treatments targeted to
the genomics of patients with high-mortality cancer and unmet clinical need.
...
Until recently, clinical trials were generally used to test a
new treatment, with some patients getting the new drug and the others getting
an existing drug or placebo. The MoST protocol tests multiple treatments at the
same time and all participating patients receive a treatment. The advent of
personalised medicine means that treatment is guided by the genetic make‑up
of the patient and their illness.
First, all patients, and their tumours where possible, are
genomically screened to see if they are suitable for a trial and if there are
biomarkers that can guide the treatments that can be trialled. These
‘signal-seeking’ trials are looking to see if a treatment will work, or work
more effectively than another treatment. The MoST protocol looks to understand
how targeted therapies work and find new biomarkers that can predict which
patients will benefit from these treatments.
After screening, patients will be offered one of three
options:
- MoST clinical trials, including immunotherapies
- Clinical trials outside MoST that use molecular
eligibility criteria
- Other biomarker-guided treatments outside MoST.
All participants, including those with no ‘actionable’
biomarkers, will be informed of the results of the screening of their tumour
tissue through their own doctors.[69]
5.70
The MoST protocol 'is also conducting clinical studies to test novel
immunotherapy drugs in patients with high-mortality cancers' through two
separate studies, although, it is noted that while 'immunotherapies are proving
to be effective in many cancer types, they do not work in all patients':
MoST researchers are looking to find biomarkers that can
predict which patients will benefit from specific treatments targeting the
immune system and to better understand how immunotherapies work to fight
cancer. With this knowledge, the team aims to develop a more precise approach
that tailors treatment with immunotherapy to individual patients based on the
characteristics of their immune system and its interactions with tumour cells.
The immunotherapy trials will allow us to understand how
these immune biomarkers influence the anti-tumour response and help develop a
precision immunotherapy approach where treatment can be personalised.[70]
5.71
The Garvan Institute established the GCMP in collaboration with the
NHMRC Clinical Trials Centre and with the support of the New South Wales
government.[71]
The NHMRC has also:
...committed $27.5 million from the [Medical Research Endowment
Account] to support the International Cancer Genome Consortium (ICGC) between
2009 and 2014.
The ICGC is a confederation of members (mostly key funding
agencies in major countries) that agreed to work in a coordinated and
collaborative manner to characterise a minimum of 500 unique cases for 50
different cancer types or subtypes that are of the highest clinical and
societal importance across the world. The aim was to obtain a comprehensive
description of the full range of genetic events associated with these tumour
types and make the data available to the entire research community as rapidly
as possible, and with minimal restrictions, to accelerate research into the
causes, diagnosis and control of cancer.
The $27.5 million grant was awarded to Professor Sean
Grimmond (Institute for Molecular Biosciences, University of Queensland). This
funding supported two large Australian-based projects to characterise ovarian
and pancreatic cancers. The ICGC has now evolved into ICGC medicine (ICGCmed)
that will link genomics data to clinical information, health and response to
therapies.
5.72
In speaking to this funding grant, Dr Elizabeth Johnson of the Victorian
Comprehensive Cancer Centre (VCCC) informed the committee that it 'allowed
Australia to go to the forefront of pancreatic cancer research in particular'.[72]
5.73
Indeed, Professor Johnson noted that the VCCC chair, Professor Sean Grimmond:
...is now leading genomic approaches particularly in pancreatic
cancers. Australia is now a world leader on that, with that allocation of
funding for a specific purpose for a limited amount of time having seeded
something very significant that has now put us at the forefront of research in
pancreatic cancer genomics. So there is precedent for it to happen that way.[73]
5.74
The NHMRC has also funded the Genomics Revolution in Health Care program,
in 2015 providing:
$25 million in funding for a Targeted Call for Research (TCR)
into Preparing Australia for the Genomics Revolution in Health Care (for
funding commencing in 2016). The aim of this targeted call was to support research
that will provide evidence and information that could be used to help prepare
Australian policy and practices for implementation of genomic information into
health care. NHMRC sought to fund a single, multidisciplinary, nationally
focussed grant through this TCR.
The funded application supports a national alliance of
clinicians, researchers, health economists and policymakers to evaluate the
case for clinical genomics across inherited disease and cancer, and to
determine how best to deliver this to the patient and to train a capable
workforce.[74]
5.75
Cancer Australia has also contributed to genomic research in Australia,
in 2013 establishing and funding:
...the Genomic Cancer Clinical Trial Initiative to
provide [National Cancer Cooperative Trials Groups] with expert advice and
technical services relating to the collaborative development of genomics-based
clinical trials protocols. From 2013 to the present, this initiative has led to
the development of 17 new concepts for genomics-based clinical trial protocols across
multiple cancer types, including a multicentre, randomised study specifically
focussed on new treatment approaches in rare cancers.[75]
5.76
Cancer Australia remarked that:
Recent advances in genomics have increased our understanding
of cancer at the molecular level, leading to new approaches to diagnosis and
treatment. Genetic sequencing technology has enabled cancers to be
re-classified based on a specific tumour mutation (or mutations) rather than
the site of origin of the cancer. This has led to the development of
genomics-based clinical trials that test a therapy or combination of therapies
targeted to the mutation across multiple cancer types, and can provide
important insight into the effectiveness of targeted treatment interventions.
Genomics-based clinical trials present opportunities for patients with low incidence
cancer types to join...larger clinical trials based on the genomic profile of
their cancer, rather than its site of origin.[76]
5.77
Despite government funding for genomics research via the NHMRC and
Cancer Australia, Professor Stephen Fox, Director of Pathology at the
Peter MacCallum Cancer Centre informed the committee that:
Most international countries of any ilk have large,
stratified medicines programs independently funded outside basic science
routes, which is the NHMRC or even the [Medical Research Future Fund (MRFF)].
They have large precision medicine programs in the US, as well as institutional
ones. In the UK you have got Genomics England, a genomics centre in Scotland
and there is even a genomics centre in Wales. In Australia I think we are a
little bit behind there. And there is a genomics centre in Kuwait as well, I
believe.[77]
5.78
Professor Fox also informed the committee that, from a testing point of
view, the regulatory process in Australia has not caught up with genetic
advances in understanding cancers, noting that Australia is 'way behind
international benchmarking'.[78]
Professor Fox elaborated:
The amount of genomic genetic testing available on the [Medicare
Benefits Schedule (MBS)] is absolutely minimal, and what there is, is usually
tied to a particular drug. So we have nothing in our armamentarium to provide
diagnostic tools. We get no reimbursement for that. Indeed, should we try to
make a proposal through the [Medical Services Advisory Committee (MSAC)]
process for some of the tools that we require, we can't fulfil the requirements
because the evidence base is so small. So for example, when you want to do a
generic platform and apply it to multiple tumour types—because you are looking
for a genetic change, as opposed to a particular tissue stream—you are not able
to do that whatsoever, which is very disappointing.[79]
5.79
Recognising that Australia lags behind in some aspects of genomics, the CCA
and COSA advocated for 'new, longer-term and more flexible funding grants...to
enable the development and maintenance of equipment, technologies and other
large-scale research infrastructure such as biobanks and genomics
services'.[80]
5.80
Roche explained that '[b]y looking beyond the "site" of a
cancer to its molecular biology and understanding the true complexity of the
disease, we can find solutions that work for both common and rarer cancers'.[81]
The CBCF observed that '[o]ver the past few years we have begun to see the
importance of biomarkers in cancer control', and advocated for using biomarkers
'whenever possible to provide another layer of important information for both
clinician and patient...[which] has the potential to result in better targeted
treatment and better health outcomes'.[82]
5.81
However, the committee heard that there are barriers to genetic testing
and identification of biomarkers in Australian LSR cancer patients. For
example, NSW Oncology Group (NSWOG) Neuro-oncology noted that there are issues
of equity that currently affect individuals with particular sorts of cancers:
At present detailed characterisation of individual patient
tumours is available only in a research setting. While common genetic
alterations such as mutations in the IDH gene are routinely tested as part of
pathology, further analysis is not made available for the vast majority of
patients – clearly limiting the ability of the treating team to potentially
tailor treatment to that is best for the patient. The correlation of this is
that this may alter survival rates adversely.[83]
5.82
Ms Linda Ferguson discussed how the lack of government rebates through
the MBS prevented her wife from undergoing tests that Ms Ferguson believes
would have assisted other patients who shared the same biomarker(s):
I do recall Leanne was offered a particular blood test when
we first moved to the Gosford healthcare system. I cannot recall exactly what
this test was for, whether it was looking for genetic markers or methylation
status of the tumour—I just cannot remember—but I recall we were told it would
not be refunded through Medicare and that we would be out of pocket about $350
for doing it. Leanne asked the doctor how would her treatment be done
differently depending on the results of the test, and we were told that there
would be no change to her treatment regardless of the results. This made us
think, well, why would we pay $350 for a test that is not going to help her—so
we did not do that one. In retrospect, with the benefit of hindsight and with a
better understanding of the circumstances in which these doctors are working, I
now believe this test was not offered to help Leanne but was offered instead to
help future patients. It was a way of giving the doctors additional
information—an extra variable to add to the mix to help them make decisions about
future patients who might share the same characteristics as Leanne.
So I guess we were being asked to pay for information that
was essentially adding to what is known about brain cancer. We were being asked
to pay for this ourselves because no-one else was paying for it. I do not
begrudge doctors learning from patients—indeed, with rare cancers I believe we
must learn something from each and every patient—but for that cost to be borne
by the patient or their family when brain cancer already places the heaviest
financial burden on households and has the highest per person lifetime economic
cost, it is simply wrong. If there is a blood test or a suite of blood tests
that that could provide some of the missing jigsaw puzzle pieces, then surely
we owe it to our loved ones, if they are willing, to do these tests and for
them not to have to pay for them. At the very least, why couldn't the cost of
these tests be covered by Medicare?[84]
5.83
The CBCF also advocated for the reimbursement of biomarker testing.[85]
5.84
Bristol-Myers Squibb (BMS) identified the increasing use of biomarkers
in oncology as a 'positive step in improving patient health outcomes', but
stated that 'the requirements to fulfil both the [Pharmaceutical Benefits
Advisory Committee (PBAC)] and MSAC processes add complexity and evaluation
time':[86]
Clinical trial design for cancer medicines is providing real
challenges to the reimbursement process, it is exceedingly difficult for the
newer cancer agents to prove cost effectiveness against the older cytotoxic agents.
This is primarily due to one of the key reimbursement criteria being the
requirement to demonstrate cost effectiveness against the comparator, defined
as the treatment that is most likely to be replaced in clinical practice.
However with the rapid emergence of new cancer medicines, the
treatment landscape is rapidly evolving and as such, the appropriate comparator
for the purposes of evaluating cost-effectiveness may not be known at the time
the trial is designed for the assessment of safety and efficacy. This poses a
problem because it is quite likely – and most often the case – that the
appropriate ‘main comparator’ nominated within a reimbursement submission is
not the comparator(s) of the Phase III clinical trials.
In this case, the therapeutic efficacy and safety of the new
medicine relative to the appropriate comparator has to be estimated indirectly
from clinical trials with a common third comparator. This is less
methodologically rigorous than the direct comparison method. In fact, the PBAC
has a low acceptance of using indirect comparisons to substantiate claims of
clinical superiority and cost effectiveness. [87]
5.85
Professor Andrew Wilson, the Chair of PBAC agreed that 'one of the
challenges' is 'what's the right comparison?':
It's challenging in that it's tempting for companies to say,
'This drug works better for this smaller group of patients,' and then they can
get a better price for the drug, so then they don't go and examine these other
patients whom it may benefit. It's challenging in that those same markers may
be just predictors of a tumour which is going to behave well or behave badly
anyway, so they may be a prognostic marker: if you've got that, your tumour's
going to do better or your tumour's going to do less well. And then we give you
this drug and, lo and behold, you seem to do better compared to the others, but
actually it's related to the biology of the tumour itself.[88]
5.86
In contrast to the optimism about genomics and biomarkers expressed by
other submitters and witnesses, Professor Wilson also stated:
If you believe the hype at the moment, you would think we
were there, that we could characterise tumours on the basis of some form of
genomic mapping or some sorts of markers, and we'd be able to choose just the
perfect drug for you. Unfortunately, while there are many promising aspects of
this, we are still quite a substantive way away from where this is likely to be
widespread.[89]
Immunotherapy and personalised
medicine
5.87
Immunotherapy refers to a treatment:
...that uses certain parts of a person's immune system...to fight
cancer. Immunotherapies are thought to work by slowing the growth and spread of
cancer cells, and by helping the immune system destroy existing cancer cells.[90]
5.88
According to the NHMRC, personalised medicine applies knowledge about
genetics to predict disease development, influence decisions about lifestyle
choices and/or tailor treatment to an individual. As a result, personalised
medicine is expected to:
...result in better disease prevention and more accurate
diagnosis of disease. Personalised medicine could also use knowledge of the way
specific genes work with medicines to tailor more effective treatment of disease
for each individual.[91]
5.89
During the course of the inquiry, both the immunotherapy and
personalised medicine were identified as important areas of development in the
treatment of LSR cancers, and a source of hope for LSR cancer patients and
their families.
5.90
Ms Susan Pitt, a consumer advocate, stated that '[w]e already have
surgery, chemotherapy and radiation, but the big brave new area is
immunotherapy...That is a big area of hope for patients'.[92]
Professor Buckland described 'the new wave of immunotherapy for melanoma' as a
'great example' and 'a very exciting new area of oncology'.[93]
The CBCF stated:
Immunotherapy in other diseases has become quite
revolutionary. Diseases like melanoma, which typically had a poor prognosis,
are actually seeing great improvements in survival. Melanoma is a solid tumour,
just as brain cancer is a solid tumour. We understand that there are significant
differences, but we are looking at a number of activities to look at
immunotherapy of all different types in brain cancer. Some of the results are
promising. It is not quite as exciting as melanoma yet—we have not really
cracked that—but there is definitely evidence to suggest that it is an area
worth considering.[94]
5.91
Merck Sharp & Dohme (Australia) (MSD) described immunotherapy as
'[o]ne of the most promising innovations in cancer treatment' and explained why
it is focussing its research on immunotherapies:
Initially, when the immunotherapy mechanism of action—this
concept that your immune system is used to fight against the tumour—came about,
I think what quickly became apparent was that you could use this treatment,
rather than its being a targeted treatment in a specific tumour, that all of a
sudden this mechanism of action had applicability across multiple tumours,
which offers a real opportunity and low survival rate in rare cancers, frankly.
So, we have embarked on what we call a tsunami of work, really, which is trying
to test or trial this drug in multiple tumours really at the same time...[95]
5.92
Like BMS (see paragraph 5.83), MSD raised the difficulties of getting an
immunotherapy listed on the Pharmaceutical Benefits Scheme (PBS). Both MSD and
the CBCF noted that the US Food and Drug Administration (FDA) has taken a
different approach to assessing immunotherapies[96]
and clinical trial protocols for LSR cancers:
We funded an international project with 160 researchers
coming together to talk about this based in Arizona State University. All the
researchers were from all over the world and from top institutions. The
protocol was written and submitted to the FDA, and we thought it was quite
ambitious. The FDA came back and said, 'Be more ambitious. This is the future
of drug development. We would like to see treatments developed around the
disease, not by the pharmaceutical company.' So this would act as a platform.
Rather than companies like Pfizer or Roche running their own trials, this would
be done by a number of pharmaceutical companies at the same time. Also, rather
than going from a phase 2 trial to a phase 3 trial, which could take six years,
this would compress the phase 2 and phase 3 trials, reducing it down to a
couple of years. So you can see it would reduce significant cost, reduce significant
time and, also, act as an incentive for biopharmaceutical companies to get
involved in the area.[97]
5.93
In an October 2017 report commissioned by MSD, Deloitte Access Economics
made the following recommendations with respect to improving awareness,
availability and affordability of immunotherapies:
-
to improve awareness:
-
change the language to one of
survivorship and immunotherapy as a potentially transformative alternative for
many patients, where appropriate;
-
ensure patients have access to
reputable and evidence-based information, setting out what immunotherapies are
available in Australia for whom, and how to access them as they are emerging
through the pipeline, including information on biomarker testing where appropriate;
-
remove sectoral silos and develop
partnerships between research, industry and academia, with patients in the
middle, to help ensure patients and clinicians can navigate information
channels effectively; and
-
provide further support to
survivors who face financial constraints, such as counselling services and
return to work programs.[98]
-
to improve availability:
-
systemic change similar to what
has recently been demonstrated by the [United
States' Food and Drug Administration],
adopting a tumour agnostic approach that recognises molecular level treatment;
-
increased investment and
coordination in availability of biomarker and screening tests, to better target
therapies towards biomarkers that are likely to respond;
-
faster implementation of the new
mechanisms available since the [Therapeutic Goods Administration (TGA)] Review;
and
-
greater awareness among
oncologists of the TGA’s provisions for special access.[99]
-
to improve affordability:
-
capacity constraints in PBAC
processes need to be overcome to ensure that listing of new medicines is not
delayed as increasingly more fill the pipeline, since the speed of listing is
critically important and cancer is already the slowest therapeutic area to be
reimbursed;
-
reimbursement decisions in PBAC
need to link with TGA tumour agnostic assessments across a range of therapeutic
outcomes, with serious consideration of new models for funding immunotherapies
into the future;
-
recognising the substantial cost
of innovative biological molecules, affordability considerations should include
life-saving and compassionate access to trials; and
-
the entirety of benefits from
newer medicines need to be valued including not just health system, longevity
and quality of life impacts, but also productivity and other impacts on
patients, carers and society. Data should be captured in trials.[100]
5.94
The committee also heard that the regulatory framework in Australia
differs to that in the European Union (EU) and United States (US), which
provide greater flexibility for basket studies that use biomarkers, and can
have positive results for people with LSR cancers:
Innovative trial designs are being explored to support access
to treatments for rare diseases, where it is not feasible to conduct randomised
trials. Studies known as “basket studies” look at a patient group with a mix of
tumour types that have common biomarkers, rather than conducting studies in
each tumour. However, such studies are not currently accepted as an evidence
base by the Therapeutic Goods Administration, the [PBAC] nor the [MSAC],
although they are more acceptable by EU and [US] regulators. There needs to be
further discussion on the role of these types of basket studies when making
decisions on access to treatments for rare diseases, especially as there is
some excellent research currently being conducted in Australia using these
types of trial designs.[101]
Committee view
5.95
Advances in genomics, molecular biology, personalised medicine and
immunotherapy offer hope and the possibility of innovative and effective treatments
for LSR cancer patients. Australia is well served by so many passionate and
committed medical researchers in these fields, who work tirelessly and without
widespread recognition, and who have to endure the vagaries of uncertain
funding streams. Supporting their efforts is vital if improvements are to be
made to the survival rates for LSR cancers.
5.96
The committee hopes that the recent changes to the NHRMC's funding model
will see genomics and other research into personalised medicine and
immunotherapies funded over periods that enable researchers to substantively
progress their work. The committee expects that its recommendations in relation
to data and a national biobank will also assist medical researchers and support
further advances.
5.97
However, the committee shares the concerns of NSWOG Neuro-oncology, the
Peter MacCallum Cancer Centre and others that Australia is lagging behind
comparable countries in its support for genomics and provision of routine
genetic testing of LSR cancer patients. The Australian government should ensure
ongoing funding for genomic research, through organisations such as the
Kinghorn Cancer Centre. The government should also consider reimbursing LSR
cancer patients for genetic testing, via the MBS, both to contribute to
scientific understanding of these cancers and also to assist in the
identification of personalised treatment for LSR cancer patients in the future.
Recommendation 13
5.98
The committee recommends that the Australian government ensures
ongoing funding for genomic research into low survival rate cancers.
Recommendation 14
5.99
The committee recommends that the Australian government implements
any recommendation from the Medical Services Advisory Committee to list genetic
tests for low survival rate cancer patients on the Medicare Benefits Schedule
so that these tests are routinely available to these patients and reimbursed.
5.100
The committee acknowledges the government's implementation of some of
the recommendations arising from the medicines and medical devices review
(MMDR), in relation to the TGA's approval processes, and its commitment to
implement others (see chapter 2). The committee welcomes the reduction in
regulatory barriers for the supply of certain unapproved therapeutic goods and
expedited review of 'vital and life-saving prescription medicines'. The
committee urges the TGA to implement the other recommendations, particularly
the provisional approval pathway that will provide earlier access to new
medicines without a full dossier of clinical data but where there are
potentially substantial benefits to Australian patients.
5.101
Further and with respect to the use of clinical trials based on
biomarker rather than tumour location, and having an immunotherapy approved for
use and listed on the PBS, the committee believes it is essential that the TGA
and PBAC (re-)examine their assessment processes and the appropriateness of those
processes for innovative treatments for LSR cancers. The committee finds it
unacceptable for a "one size fits all" approach to be applied to the
assessment of innovative treatments, such as immunotherapies, for LSR cancers
when it is clear that the existing approaches are ill-suited to these
treatments and no improvements in survival rates for these cancers have been
made. Put simply, if it is acceptable for European and American regulators to
adopt more flexible and innovative approaches to assessing immunotherapies—including
approval or acceptance of novel clinical trial protocols—the committee sees no
reason why, pending a (re-)examination of TGA and PBAC assessment processes,
more flexible and innovative approaches should not be adopted in Australia.
Recommendation 15
5.102
The committee recommends that the Therapeutic Goods
Administration, if necessary following the medicines and medical devices
review, and the Pharmaceutical Benefits Advisory Committee:
-
(re-)examine their assessment processes and the appropriateness
of those processes for innovative treatments for low survival rate (LSR) cancers,
such as immunotherapies; and
-
pending that examination, consider adopting more flexible and
innovative approaches to approving innovative treatments for LSR cancers and assessing
them for listing on the Pharmaceutical Benefits Scheme.
Access to medicines
5.103
The committee heard that in some instances, there are medicines
available that may assist in treating LSR cancers, but that these drugs are
approved for use in Australia for a different indication or are not approved
and available for use in Australia at all. Equity of access and the
availability of medicines via the PBS was also discussed during the course of
the inquiry.
Repurposing drugs
5.104
The Thoracic Society of Australia and New Zealand argued that there are
many drugs already approved for use that may be effective in treating LSR
cancers, describing the use of these drugs as 'a low-risk avenue to increase
possible cancer therapies':
This approach takes drug molecules which have already been
designed, developed, characterised and tested for safety and efficacy in humans
and applies them to a new formulation, method, or target. It is estimated that
most safe-approved drugs will possess secondary indications for use in another
setting. This will be a time and cost saving endeavour. There are numerous
examples for drugs currently in use which were originally developed to treat a
different illness.[102]
5.105
A number of other submitters and witnesses also supported the repurposing
of drugs approved for other indications as potential treatments for LSR cancers.[103]
RCA remarked that '[t]here are many opportunities to repurpose existing drugs
from common to rare cancers, but we need evidence and flexibility'.[104]
5.106
Professor Johns explained how the physiology and biochemistry of the
brain make drug treatment difficult,[105]
and outlined how the BCDC engages with pharmaceutical companies to test drugs used
for more common forms of cancer as possible treatments for brain cancer:
The way that I mostly do it is that they will develop a drug,
say, for breast cancer or lung cancer, that we believe might have utility in
brain cancer, but they are not interested that because the finances do not make
sense as it is rare, so we will work with them to get some of the drug and
maybe a little bit of money, and develop the background and do the preliminary
experiments in the test tube and animal models to give them the confidence to
move forward with that drug in this space. So, it is through partnerships with
them. They can come to the groups like the [BCDC] and see that we have the
ability to take their drug through all of the tests and evaluations they need
to do to be confident to move it forward into brain cancer. That is certainly
one thing that we are very focused on and have done in the past, but we still
need the basic research to know the companies to approach that have the right
drugs that might be effective.[106]
5.107
RCA highlighted research being undertaken at the Garvan Institute:
...at Garvan, there is a trial being run by Professor David
Thomas which looks at analysing the genetic make-up of tumours and then trying
to define treatments from existing drugs. There is so much opportunity in this
process to repurpose. We have got a whole arsenal of drugs on the shelf here,
but we just need to go through—they may have been developed for breast cancer,
lung cancer or bowel cancer, but, if we are really clever about it, we can run
trials, test them and, we might find...that the drug that was developed for lung
cancer is ideally suited...We need to do work in that area, and David Thomas has
set up a trial that, like all research, is hard to fund, but it is an example
of what is possible.[107]
5.108
TBTC spoke to the approach in the UK, and noted the role that charity
organisations can play in helping pharmaceutical companies repurpose drugs:
I think that there are differences between a drug that's
still on patent, and therefore being driven by a company and their ability to
make profit, and one that's off patent. There was a bill that was put to
parliament to bring about an easier way of taking those off-patent drugs
forward, but that didn't make it through. There are currently discussions
around putting that bill forward again.
I think that when we're talking about a drug that's
effectively a cancer drug for a different cancer type and moving that into
brain or pancreatic, and when that's under patent by a company, then, as
charities, we have a role to play in helping the company facilitate that,
because the company still has the barrier of the investment versus the return,
and we don't have that barrier. So we would like to be able to work more
closely with companies and access their drugs to be able to do those trials.
There are continuing to be discussions around that. I personally feel that the
industry is becoming more open to those approaches. I think there's just some
work to do to maybe make them easier still.
The off-patent drugs are a challenge, because this will have
to be funded through charitable or not-for-profit organisations. Personally we
don't have any problem with a researcher bringing us those sorts of
applications. Whether or not they would ever become licensed is the problem,
because then the question would be: who would actually submit for the licence
application? I think that that's where we need to make some changes to allow
that to be an easier thing to do and also to give some indemnity for that
person. For example, as a charity, we wouldn't be able to bring a drug to
market, because of the potential risks to the charity were that drug to be
found at a later stage to be harmful.[108]
5.109
Indeed, internationally, there are other innovative approaches to
incentivise pharmaceutical companies to perform clinical trials to repurpose
drugs, as the QBI explained:
Big pharmaceutical companies will not start a clinical drug
trial for a rare disease where there are not many, but they will do anything to
be able to sell more. Actually in Europe there are a few initiatives where, for
instance, if they actively seek to repurpose drugs for rare diseases, they can
keep their patent for a couple of months longer or have an advantage over
competitors.[109]
Listing on the Pharmaceutical
Benefits Scheme
5.110
Equity of access to medicines for patients with LSR cancers as compared
with patients with more common forms of cancer was also the subject of
discussion during the inquiry. In particular, submitters and witnesses
highlighted that some drugs are available via the PBS for patients with certain
cancers, but not for LSR cancer patients, or have been approved and are
available for use overseas but not in Australia.
5.111
For example, Ms Ferguson explained that her partner, who suffered from
neutropaenia as a result of chemotherapy for brain cancer, was not entitled to
the same treatment as those patients with breast cancer and neutropaenia.[110]
5.112
RCA gave an example of a woman with anaplastic lymphoma kinase (ALK)
positive cancer for which:
There is no known diagnosed treatment for this on the PBS,
but there is a version of lung cancer that is also caused by that mutation.
Through a process of initially paying for the medicine through our crowdfunding
service and then, subsequently, through us and her clinician, lobbying the pharmaceutical
companies, she is now on a compassionate program for those drugs.[111]
5.113
Ms Marilyn Nelson told the committee:
What can happen, and has happened to someone I know...is that
her doctor did not actually tell her about this drug because he was weighing up
the cost of presenting her with something that she could not afford. He chose
not to tell her about this drug. The only way she could get it was to pay about
$8,000 a month. He did not tell her—she found out about it through other
sources. She said, 'I'm going to pay it—we'll mortgage the house, we'll find
money somehow.' It is ongoing at $8,000 a month. Eventually Rare Cancers
Australia helped her with some crowd funding and then eventually it got on the
PBS, but it was months and months of paying thousands of dollars to get access
to a drug that is already approved and in use in the [US] and [EU]. It has part
of the approval—maybe the TGA approval—in Australia, but it is going through
these painfully long processes for getting approval on the Pharmaceutical
Benefits Scheme. As patients, we know this drug is there. We know it is being
used everywhere, not here. Then we find we can actually get it as long as we
are prepared to take out a mortgage on our homes. It is something we face a
lot, and we find all this information ourselves...[112]
5.114
Mrs Evangeline Lim, a lung cancer patient, described her 'constant fear
that I will run out of treatment options, let alone be offered a cure'.[113]
Mrs Lim described herself as lucky that Xalkori, a targeted treatment, is
available to her, but also told the committee that 'America is more advanced as
far as pills and treatments go' and that three other treatments have recently
been approved in America, but are not available in Australia.[114]
5.115
With regard to the absence of PBS-listed treatments for LSR cancers, RCA
stated that:
It is no small coincidence that government research funding
into rare cancers remains disappointingly and disproportionately low, as does
the money we spend on treatments for these patients through the Pharmaceutical Benefits
Scheme. These two are closely related, as research generates evidence to justify
PBS funding, and it is a direct consequence that the drugs are not listed on
the PBS; it is a lack of research.[115]
5.116
Mr Vines of RCA continued:
The PBS requires evidence of
cost-effectiveness. I always describe it like this: imagine that the only way you
would decide what car you bought was on the basis of fuel economy. The
decisions the PBS makes are not entirely but largely driven by improvement in
survival for a cancer patient. If the current drug gives you three years and
the new drug gives you four years, you have an extra year, so the cost related
to that is balanced off. And that is regardless of what the side effects are.
There is no measure of the side effects; there is no measure of how many times
you are hospitalised or anything like that.
...
The second part of that is that you have to look at the
pharmaceutical industry, and, for a patient population of 30 or 40 in
Australia, there are two restrictions: one is, do they have any evidence at all
and have they run a trial on that? And secondly, putting in an application to
the PBS is a big job. As a charity, we applied to list two drugs last year so
we understood the process. Aside from the financial investment, they have a
team of people whose job it is to make applications to the PBS. If I were running
that team, sitting there, I would say: do I make an application for this drug
here, which might be melanoma or breast, which will give me thousands of
potential uses, or do I make it for Merkel cell carcinoma, which is going to
give me 300? I only have a certain number of hits.
So we need to think about how we make that a bit easier...one
of the things we have thought about is: can we make it so that they can apply
for several at the same time and bundle them up to make that process more
efficient?[116]
5.117
The committee also received evidence about the difficulties with respect
to the interaction between the PBAC and the MSAC processes.[117]
For example, MSD outlined how a co-dependent submission—'those submissions
where they rely on a drug and a test combination'—can delay access to drugs:
With the co-dependent submissions...the patient would first
need to be tested for a particular biomarker and then, provided that the
patient has a particular biomarker, then they would qualify for treatment with
the drug. That is called co-dependent submissions or co-dependent products in
Australia. The challenge we face with those types of products is that we have
the test which is funded through a separate committee—MSAC. And then we have
the drug that is funded through a separate committee, the PBAC, which we are
all familiar with. And the process of integration between the two is
problematic.
The process needs to start early, especially on the test
site, and that is where it takes almost twice as long as for the drug, because
we need to start the process very early on, sometimes when we do not even have
some data in order to be able to go through the process. It is the interaction
between those two committees. They do not meet at the same time. There are
complexities associated with putting forward the health economic arguments.
There is an expectation around certain types of evidence which does not happen
overseas. That type of information might not necessarily always be available in
the clinical studies.[118]
5.118
Professor Fox of the Peter MacCallum Cancer Centre stated that the
applications to PBAC and MSAC—which are submitted simultaneously—are 'out of
sync', and recommended that the delays in the process could be assisted by
aligning the committees, such that they communicate with each other more.[119]
Professor Fox also suggested that the PBAC and MSAC be merged into a single
committee.[120]
5.119
This recommendation for a single committee was also made by MSD,[121]
which noted that 'reimbursement submissions are often co‑dependent technology applications,
requiring submissions to both the PBAC and MSAC, which can significantly
lengthen approval timelines'.[122]
In addition to its recommendation for a single committee, MSD also recommended that
the Australian government:
-
conducts a review of evidentiary
expectations for co‐dependent applications and benchmarks these to
comparable reimbursement authorities overseas
-
implements a framework for a
managed entry scheme for diagnostics used in co‐dependent technologies, similar to what has been in
place for pharmaceuticals since 2011, to enable access to patients whilst more
conclusive evidence is being generated.[123]
5.120
Similarly, Medicines Australia advocated for streamlining 'the
evaluation and decision making process for co-dependent medicines', on the
basis that 'medicines for rare or low survival cancers often rely on the use of
a diagnostic to identify the appropriate patient population'.[124]
5.121
Professor Wilson, Chair of the PBAC, emphasised the importance of
'[f]it-for-purpose clinical trials that inform [PBAC's] decision-making', and noted
that where an international trial takes place, 'we don't understand how they
work within the services which are available within Australia', and 'the
treatment plans and treatment approaches for some of these tumours may vary
within the Australian context'.[125]
5.122
Professor Wilson also stated that, in order to list a drug on the PBS,
'[w]e would certainly want to see the evidence from a trial', noting that '[i]f
a drug's going to be used and promoted broadly in the community then there
needs to be substantive evidence that it works and not just, "You might
want to try that"'.[126]
5.123
In response to the discrepancy in neutropaenia treatment for brain and
breast cancer, Professor Wilson told the committee:
The decision about the listing of Filgrastim and the other
variations on the same drug were based on the cost-effectiveness. So patients
develop [neutropaenia] at different rates, depending on what chemotherapy
regimes they happen to be on. There are chemotherapy regimes which have high
and low rates of [neutropaenia]; there are ones which have very low rates of
[neutropaenia]. The original approval for the drug would have been based on the
regimes which caused the higher rates of [neutropaenia] in relation to that.
Having said that, we are currently in the process of negotiation around an
extension of that, so I can't say any more about it. But we have been
approached to look at that more broadly and are currently working on that.[127]
Committee view
5.124
The committee applauds the research of institutions such as the BCDC and
the Garvan Institute investigating whether certain drugs already used in the treatment
of more common cancers, and even other diseases, might be repurposed for use in
the treatment of LSR cancers.
5.125
The committee believes that institutions such as the BCDC and the Garvan
Institute should be supported to conduct further research into repurposing
existing drugs. Consistent with its other recommendations, the committee
recommends that the Australian government ensures that funding is available to
researchers investigating whether existing drugs may be suitable for treating
LSR cancers.
Recommendation 16
5.126
The committee recommends that the Australian government ensures
funding is available to researchers investigating whether existing drugs may be
suitable for treating low survival rate cancers.
5.127
The committee also notes the approach in Europe where pharmaceutical
companies that actively seek to repurpose their drugs for rare conditions are
able to extend their patent or have an advantage over competitors. The
committee therefore recommends that the Australian government works with
industry to consider a mechanism to repurpose drugs appropriate for the
Australian context.
Recommendation 17
5.128
The committee recommends that the Australian government works
with industry to consider a mechanism to repurpose drugs.
5.129
There may be circumstances in which an existing drug is found to be an
effective treatment for LSR cancers, but because it is off-patent or the
patient population is so small, it is not financially attractive or clinical
evidence is insufficient for a pharmaceutical company to seek TGA approval. The
committee is aware that there can be serious implications for clinicians and
patients, with respect to adverse reactions, indemnity and insurance, of using
drugs 'off-label' and that off-label use must be approached with caution.
However, the committee heard from some medical researchers and clinicians, and
many patients (or their families) that LSR patients with no other treatment
options should be afforded the opportunity to access off-label drugs. Indeed,
as Mrs Sandra Woods told the committee: '[i]f you are diagnosed with a fatal
illness, you have got nothing to lose. You will die anyway, no matter what you
try. Trying is doing something; it is fighting back'.[128]
5.130
The committee cautiously agrees, and recommends that consideration is
given to permitting off-label access to drugs for LSR cancer patients without
further treatment options, on compassionate grounds.
Recommendation 18
5.131
The committee recommends that the Australian government considers
a mechanism to permit access to and properly supervise use of off-label drugs
for low survival rate cancer patients without further treatment options, on
compassionate grounds.
5.132
The committee is concerned by the apparent inequity of access to some
treatments for LSR cancer patients via the PBS. The committee understands that
pharmaceutical companies may make financial decisions not to seek PBS listing
for medicines to treat rare and LSR diseases, and that the PBAC's evidentiary
and cost-effectiveness requirements mean that many drugs for rare and LSR
diseases will not obtain PBS listing if sought. However, it is unacceptable
that LSR cancer patients should be left without access to treatments which are
available to other Australian cancer patients or people in foreign
jurisdictions. The committee has already recommended that the TGA, if
necessary, and the PBAC (re-)examine their approval and assessment processes
for innovative treatments for LSR cancers; the committee makes the same
recommendation with respect to the repurposed drugs.
Recommendation 19
5.133
The committee recommends that the Therapeutic Goods
Administration and Pharmaceutical Benefits Advisory Committee examine the
appropriateness of their approval and assessment processes for existing drugs
repurposed for use in low survival rate cancers.
5.134
With respect to co-dependent submissions requiring MSAC approval of a
diagnostic test or tool and PBAC assessment of a drug, the committee agrees
with the proposals that these processes should be better aligned and
streamlined.
5.135
The committee has already recommended that the Australian government
considers listing genetic tests for LSR cancer patients on the MBS; where a treatment
for LSR cancer is dependent on a genetic or other diagnostic test, the
committee recommends that the Australian government considers whether the MSAC
and PBAC processes can be streamlined so that assessment and approval is not
unduly delayed.
Recommendation 20
5.136
The committee recommends that the Australian government considers
whether the Medical Services Advisory Committee and Pharmaceutical Benefits
Advisory Committee processes can be streamlined where a diagnostic test and
treatment for a low survival rate cancer are co-dependent.
Care and support services for patients and families
5.137
A number of submitters and witnesses expressed their frustration and
disappointment about difficulties accessing care and support services, such as care
co-ordinators or nurses and welfare payments.
Care and support services
5.138
The committee heard from a number of submitters and witnesses that being
diagnosed with a LSR cancer can cause patients to feel isolated and
unsupported.[129]
QIMR Berghofer suggested that this is a consequence of the rarity of the
cancers, such that '[t]hey are not common enough to justify specific support
services at all centres', despite the fact that such care is important,
regardless of where patients live.[130]
5.139
For example, Mr Tim Eliot recounted the problems that he experienced
with respect to receiving information about research and treatment options,
including that '[t]echnical documents supplied post-surgery, such as pathology
reports, often have little explanatory or interpretive information beyond what
is provided verbally', and that there are '[i]nformation gaps in how to access
and best use available care and support services, including Cancer Council;
Allied Health; Public/Private cancer care choices'.[131]
5.140
These issues appear to be exacerbated for people living in regional and
remote areas. For example, Mrs Suzanne Turpie informed the committee about the
lack of support available for her son, a brain cancer patient, once he leaves
the metropolitan area in which he receives his treatment:
We have pretty much no help. As soon as we leave Sydney we
are on our own. We see our local GP, who I cannot fault, though she is not a
specialist in the field at all. It is only when we go to Sydney every three
months that Caleb gets the support and help that he needs. We are desperately
crying out for Caleb to be able to see a psychologist right now. After
everything that has happened to him, he has terrible nightmares, terrible
dreams, and it is impacting his life quite a lot. We cannot get in to see a
psychologist in Port Macquarie at all. We are screaming out. We just cannot get
into one. So he only gets mental help when we go to Sydney, and that is not
good enough. He needs help and he cannot get it.[132]
5.141
Ms Dianne Dunn, who lives 45km from a major regional town and was
diagnosed in November 2016 with an inoperable brain tumour, shared a similar
experience.[133]
Ms Dunn outlined a number of difficulties that she faced with respect to her
diagnosis, such as her inability to easily seek a second opinion about her
initial cancer diagnosis, and suggested that such difficulties could be
addressed by '[p]roviding greater access to those in regional areas to support
services – transport to treatment, accessing second opinions'.[134]
5.142
Another issue raised was the difference in support available for patients
depending on their cancer. For example, Ms Ruth Churchill stated:
There is very little support in the community beyond tea and
sympathy for those with Atrial Sarcoma. Compared to breast cancer sufferers, we
are stumbling about in the dark attempting to find information and support
services. My family and I have dedicated many hours over the past four years to
researching different scientific based treatment approaches and whom to
approach for up to date information. – something that we finally feel we are
making some headway with.[135]
5.143
This was also discussed by Ovarian Cancer Australia, which provided
comments from women with ovarian cancer in response to a recent survey:
The first lady writes: 'So much pink support makes you feel
like you have the wrong cancer. Breast cancer patients even get free parking at
the hospital I went to for chemo. Ovarian patients do not.' The second lady
writes: 'At the hospital when I get infusions there are dedicated breast cancer
support nurses for those getting chemo for breast cancer. Not for me. I have
the wrong cancer.' The third lady writes: 'It feels like ovarian cancer is
where breast cancer was 30 years ago. It comes down to funding and research.'[136]
5.144
Indeed, a number of submitters and witnesses raised the issue of care co‑ordinators/
nurses, as outlined in the following section.
Care co-ordinators and nurses
5.145
Many people with a LSR cancer or their family members expressed their
disappointment about the lack of specialist care co‑ordinators or nurses,
calling for more of these positions,[137]
a sentiment supported by organisations and medical professionals.[138]
5.146
For example, in response to a question about the support services he is
receiving, Mr Shonk—who was diagnosed with a grade 3 brain tumour in
2004—stated:
Virtually zero. There aren't any. The one care nurse that
they have in the North Shore hospital is half-funded by Ramsay Health Care; the
other half is funded by SNOG—the Sydney Neuro-Oncology Group. For breast
cancer—I think I am right—they have about 90 care nurses, and some of those
patients have a lumpectomy as opposed to a mastectomy. Brain cancer is so much
more insidious; it goes on so much longer and it is so much more debilitating.
The inequities are just mind-boggling.[139]
5.147
The potential benefit of specialist care co-ordinators and nurses for LSR
cancer patients was outlined by a Lung Cancer Nurse Co-ordinator:
Our hospital offers a dedicated lung cancer
[Multi-Disciplinary Teams (MDTs)] which aims to improve patient care and
outcomes through the development of an agreed treatment plan. As a specialised
Lung Cancer Nurse Coordinator I am involved in the nursing care of our patients
with lung cancer in all treatment areas and am an integral part of the MDT. I
am an expert point of contact for our patients, providing both psychosocial and
clinical support. My experience after 14 years in this field is that supporting
patients with lung cancer to receive coordinated care is not only the best way
to care for them but is also greatly appreciated by our patients, their
families and carers.[140]
5.148
Mr Khang Chiem expressed his appreciation for the care his partner
received from a dedicated neuro‑oncology nurse care co-ordinator at St
Vincent’s Hospital, stating that:
Without her our journey through the public hospital system
would have been chaotic, confusing and demoralising. With her gentle and caring
approach, she has guided us from the first operation all the way through to the
multiple neurosurgeon appointments, and bridged the gaps between the various
departments of the public hospital on our behalf. Any questions we had, she,
time and time again, found the answers. Due in large part to the nurse care
coordinator, my partner has received the best care we could ask for as a
patient in the public health system.[141]
5.149
However, the committee heard that there are only a small number of these
nurses available relative to the number of people who suffer from LSR cancers.
For example, in 2016, when 12 000 people were diagnosed with lung cancer,[142]
the Lung Foundation Australia reported that there were 29 dedicated cancer care
co‑ordinators/lung cancer nurses in 60 MDTs in Australia.[143]
Mrs Sandra Woods noted that '[t]here is one online dedicated NETs nurse for all
of Australia where there are over 10,000 known NETs patients'.[144]
5.150
Indeed, the committee heard that it often falls to charities or
community organisations to raise funds for specialist care co-ordinators and nurses.
For example, the Centre for Community-Driven Research (CCDR), a non-profit
organisation with the goal of supporting 'a more patient-driven health sector',
established the 'Patient Engagement in Research and Services – with One Nurse'
program, which:
...gives a patient access to a registered nurse (via telephone
or video) who can help them access all available local services, understand
clinical trials that are available to them, and be a [single], central point of
support for as long as the patient needs them.[145]
5.151
The CCDR informed the committee that it had piloted the program in
pancreatic cancer over the past 12 months, and is currently testing its
transferability in brain and ovarian cancer.[146]
5.152
Ms Michelle Bradley noted that:
...the McGrath Foundation has worked hard to raise funds to
support Breast Care Nurses who offer a range of support for breast cancer
patients. This type of support would greatly assist brain cancer patients to
negotiate a complicated and daunting treatment pathway which includes surgery,
radiation therapy, chemotherapy, medications (such as dexamethasone) and to
explore potential side effects.[147]
5.153
The BTAA noted its financial support for brain cancer nurses/care co-ordinators
and other brain tumour allied health professionals, and also supported the
calls of patients 'for better access to brain cancer care coordinators', on the
basis that 'they play a critical role linking patients with treatments and with
clinical trials, as well as assisting them to navigate the medical system
following diagnosis'.[148]
5.154
The BTAA suggested that while general cancer care co-ordinators are
available across most Australian states and territories these 'are not aware of
the specific needs of brain tumour patients' and that:
Specialised cancer care coordinator nurses create
efficiencies in the system by freeing up other specialists and can assist with
recruitment to clinical trials. As suggested previously, while there have
private and private/public models to provide specialist nurses for cancers such
as breast, prostate and some others, we are calling for equitable access for
all Australian cancer patients with a poor prognosis.[149]
5.155
Dr Jonathon Parkinson, Chair of the NSWOG Neuro-oncology similarly
remarked:
This is the area in which I think we have the opportunity to
make the single, most immediate, impact on survival of brain cancer patients:
through care coordinators. Over the last few years most of the dedicated brain
cancer care coordinators have given way to more general care coordinators
covering a number of cancers, who then become preoccupied, sheerly because of
the numbers of other types of cancer sufferers. In fact, I think there are only
two dedicated care coordinators in New South Wales. We can look at the model of
breast cancer as a cancer where care coordinators have made a great impact on
survival. I think the care coordinators are even more important to brain cancer
sufferers, because of this impact on the family and the resources consumed.[150]
5.156
The Department of Health (DoH) acknowledged the benefits of specialist
cancer care co-ordinators and nurses, but stated that '[i]t's not always viable
to have specific tumour nurses for all types of cancer', further stating that:
There is evidence that cancer care coordinators improve
patient experiences. It's a difficult, challenging time, and there are lots of
care pathways to navigate. Coordinators can help in that information transfer
and stitching things together for people. You'd probably be aware that there
are cancer care coordinator positions in jurisdictions across Australia which
recognise that need to streamline patient care and help support patients across
the journey. For the majority of cases, those coordinators are employed, and
sometimes receive specialist training roles, through state and territory
governments. They're usually nurses who are experienced in cancer care. Some
are tumour specific and many are not. The role of those cancer care
coordinators varies according to the area in which they're employed, the tumour
types and the complexity of patient care needs. Metropolitan cancer care coordinators
are generally based at a single institution, often a cancer hospital big enough
to have coordinators for the care of patients with just one tumour type, though
that's not always the case. Cancer care coordinators in rural areas tend to
have to cover a number of tumour types and are often more community based. The
overall shortage of nurses is an issue that the Australian health system is
facing. In a workforce shortage situation, you need to balance the need for
more general nursing positions against increased numbers of nurses for specific
roles like cancer care coordinators.[151]
5.157
The DoH informed the committee that the Australian government 'makes a
small contribution' to cancer care nurses 'by funding a certain number of the
McGrath Foundation's breast care nurses and a certain number of the Prostate
Cancer Foundation of Australia's prostate cancer nurses', which the department
acknowledged are, incidentally, cancers with the highest rate of survival.[152]
5.158
The DoH further remarked that while 'those coordinators do help in the
survival journey':
...in the context of the total number of cancer care
coordinator positions in Australia, it's a fairly small contribution, and that
states and territories, because of their responsibility for public hospitals
and cancer centres, are generally the employers of [the nurses].[153]
5.159
In contrast to the situation in Australia, the committee heard that in
the UK '[t]here are clinical nurse specialists for high-grade [brain] tumours...that
coordinate the care of the individual'.[154]
These nurses 'will make sure they are getting access to physio and allied
health professional services'.[155]
5.160
In respect of pancreatic cancer in the UK, the approach is that 'each
person should be assigned a clinical nurse specialist once they've received
their diagnosis to help them navigate the system' through the National Health
Service, although some patients are not assigned a nurse as 'it is a role that
is in fairly short supply'.[156]
Financial assistance
5.161
In addition to the absence of support co-ordinating their care, the
committee heard about the out-of-pocket expenses facing people with LSR
cancers, and the challenges facing patients and their carers trying to access
financial support.
5.162
Some submitters discussed the financial impact of an LSR cancer
diagnosis and the financial burden of repeated diagnostic tests and treatments.
For example, Dr Parkinson remarked that 'the financial impact goes with
that...when you think of people being cut down in the prime of their earning
lives'.[157]
Mrs Margaret Shonk commented:
Yes, definitely support, and also subsidies of the
medication, the MRIs and those sorts of expenses. Usually it is the major wage
earner that is hit. You are hit with all these extra expenses. Obviously
research is key, but those other things would also help with the suffering that
many people face when they have someone in the family with a brain tumour.[158]
5.163
Mrs Turpie stated:
I am still unable to return to work. I was the main income
earner in our family, and there is no possible way that I can return to work.
We still have to come to Sydney every three months for the next four years, and
that is a massive financial impact on us, with travel costs and accommodation.[159]
5.164
Mrs Turpie has been unable to work since her son's diagnosis with brain
cancer, and described the difficulties she encountered accessing a carer's
pension:
When I was filling it out it was very much directed at what I
thought was an autistic child, high functioning, along those lines. There was
nowhere in the form where I could tick that Caleb had cancer and had
neurological problems as a result of the surgery, he was in a wheelchair, he
was going to get sicker than what he already was and he was going to require
this and that. The questions were was he suicidal, did he get up and walk away
from his bed at night, did he need to be restrained, was he at risk of leaving
the house? He was not at risk of any of that because he could not walk—he could
barely even talk at this stage. I could not tick 'yes' to the boxes that they
wanted ticked.
A friend of mine heard my plight and she got onto our local
MP, after he had been knocked back twice, and at the same time I was trying to
get onto a social worker from Centrelink to ask what it was that I needed to
do, saying that we needed help here. She said we needed to be ticking the boxes
that yes Caleb is suicidal—you need to be making a worst case scenario,
otherwise it will not get approved. So I ticked the boxes and at the same time
the local MP got involved, he rang the office and lo and behold it was approved
that afternoon.
...
It was ridiculous. I had all the letters from the specialist
stating what the diagnosis was, what the outcome was, and what we were looking
at happening, but I could not hand any of it over. I had to tick the boxes, but
it is hard to tick the boxes when the boxes are not aimed at cancers.[160]
5.165
The difficulty with navigating the Centrelink system was also reflected
in evidence from Mrs Tracey Taylor, whose son also has brain cancer:
Because everything happened so fast, you have to get
applications in by due dates and times and the amount of information that they
are asking for—yes, some of it is relevant; some of it could be different—and
then you are left to phone up to ask these questions. You are on the phone for
hours, literally hours, and then you are on hold for hours. Then it goes to a
dead end and you have wasted three hours of your day. It is time that you do
not have. It is like you need—not a fast track, but some kind of extra
assistance to say, 'Okay, this person doesn't have time to be sitting on the
phone for hours.'[161]
5.166
Mr Phil Reynolds, whose wife died from brain cancer, described his
frustration with navigating government agencies and the time it took to access
services:
In my time caring for my wife the most frustrating task was
trying to deal with Centrelink, Medicare, ATO, banks and numerous other
institutions. Whilst trying to do the best for Caroline I was having to spend
up to two days every week on the phone or waiting for my name to be called at
these places and often sent away because another piece of paperwork or
information was required.[162]
5.167
The Sydney Neuro-Oncology Group commented that '[n]avigating Centrelink
and the [National Disability Insurance Scheme] is impossible', elaborating
that:
Most cannot return to work, and even those on higher incomes
often have mortgage and family commitments. The need for constant supervision
also impacts on the spouse, children and often elderly parents. Studies have
documented the stress in caregivers for this cancer is often higher than the
patients themselves, but treatment programs and research rarely extends to the
unpaid volunteers and the long-term impact on children is unknown. Family and
carers face the emotional turmoil of being told their loved one is unlikely to
survive and have to confront the daily fear of seizures and the challenges of
both cognitive deficits and personality change, all compounded by financial
stress.[163]
5.168
Dr Rachel Harris, the daughter of a man with brain cancer, argued that
the Disability Support Pension (DSP) and the carer's pension 'need to be
streamlined'.[164]
5.169
Indeed, there appears to be limited access to the DSP for people with
LSR cancers. Following a simplification of DSP assessments from
1 July 2010, a person who has a terminal illness or profound
disability is eligible for fast-tracking to prevent these claimants being 'unnecessarily
referred for a Job Capacity Assessment and provide them with financial
assistance more quickly'.[165]
5.170
A 'manifest grant of DSP' can be made when a claimant is diagnosed with one
or more of the conditions listed in Table 7. There are other conditions, listed
on the Department of Social Services website, where a manifest grant of DSP can
be made when a claimant is diagnosed with one or more of the conditions;
undertakes additional action (such as confirming the stage of disease or
establishing the prognosis and/or level of care required); and provides
evidence that the claimant 'is clearly qualified for DSP'.[166]
Table 7: Fast-tracked DSP List 1[167]
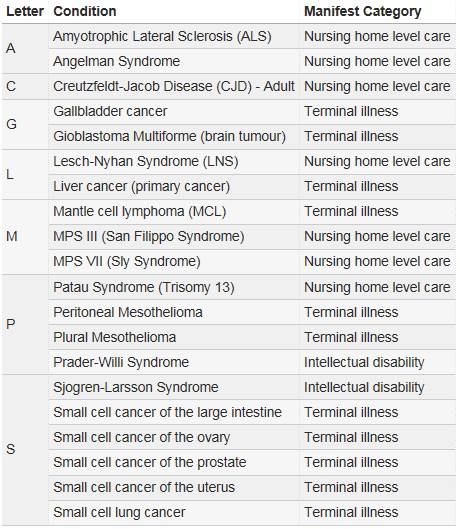
Committee view
5.171
Evidence before the committee demonstrates the benefits to patients of
cancer care co-ordinators or nurses and the support they provide. The
availability of such support has resulted in improvements to survival rates for
those with some cancers, such as breast or prostate cancer.
5.172
Submitters and witnesses to this inquiry have argued that the benefits
to patients with LSR cancers may be even greater, given the complexity of their
care and the current lack of co-ordinated care and support.
5.173
The committee does not wish to suggest that the level of care and
support provided to those with cancers with higher survival rates, such as
breast or prostate, should be diminished, and the committee in no way
criticises charities that have raised awareness about and provided support for
patients with these cancers. Indeed, the committee applauds the work of
organisations such as the McGrath Foundation for the incredible work they do
and the support they provide. However, it is disappointing that LSR cancer
patients do not have access to the same care and support. The absence of
specific care and support through specialist cancer care co-ordinators or
nurses further exacerbates existing inequalities for LSR cancer patients and
hinders improvement in survival rates for these people.
5.174
The committee is particularly concerned that the Australian government,
via the DoH, appears to only provide financial support for cancer care
co-ordinators for patients with breast and prostate cancer. It should not be
left solely to charitable organisations to fund and establish specialist cancer
care co-ordinators and nurses for LSR cancers: raising awareness and funding
can be difficult for these charities because the cancer they represent is so
rare and, tragically, very few patients survive long enough to become
advocates. It is also unacceptable that LSR cancer patients should have to rely
on charities to receive adequate care and support, given the potentially
inconsistent and uncertain flows of charitable and philanthropic funding.
5.175
The Australian government should examine how it allocates funding for
cancer care co-ordinators and ensure that LSR cancer patients have access to
specialist cancer care co-ordinators and nurses. In doing so, the Australian
government should work with its state and territory counterparts to improve
access to specialist cancer care co‑ordinators or nurses in every state
and territory. The committee expects that the provision of this care and
support will make tangible improvements in the survival rates for LSR cancer
patients.
Recommendation 21
5.176
The committee recommends that the Australian government, in
conjunction with its state and territory counterparts, works to improve access
to specialist cancer care co-ordinators or nurses for low survival rate cancer
patients in every state and territory.
5.177
The financial costs to LSR cancer patients can be large and this can
place an immense burden on them and their families. It is concerning that people
who are already vulnerable and fighting for their lives are further burdened
with loss of income and the financial stress of large medical bills.
5.178
In the first instance, the committee is of the view that the Australian
government should ask the MSAC to review the criteria for reimbursement of
ongoing diagnostic tests such as MRIs. Given this testing is not discretionary
but used to determine disease progression and treatment options, the committee
believes it is appropriate for such ongoing diagnostics to be reimbursed.
Recommendation 22
5.179
The committee recommends that the Australian government asks the
Medical Services Advisory Committee to review the criteria for reimbursement of
ongoing diagnostic testing for low survival rate cancer patients.
5.180
The government should also address the barriers and time delays
encountered by LSR cancer patients and their families when seeking financial
support such as the DSP or the carer allowance or payment. As the committee has
already highlighted, burdening LSR cancer patients and their families with
unnecessarily complex administrative processes and time delays—especially where
a person has a terminal diagnosis and time is precious—is inappropriate. The
committee therefore recommends that the Australian government further
simplifies and streamlines the application processes for LSR cancer patients
and their carers when seeking to access the DSP or carer allowance or payment.
Recommendation 23
5.181
The committee recommends that the Australian government further
simplifies and streamlines the application process for low survival rate cancer
patients and their carers when seeking to access the Disability Support
Pension, or carer allowance or payment.
A national strategy for people with low survival rate cancers
5.182
The following sections of this report examine:
-
the work of the Australian government to date developing and
implementing a national approach to cancer;
-
recent announcement for a plan to increase the rate of survival
for people with brain cancer; and
-
some key international developments.
5.183
The final section considers a proposal for a national strategy to
increase survival rates for all LSR cancers in Australia.
The National Cancer Work Plan
5.184
In April 2010, the Council of Australian Governments (COAG) agreed that:
Victoria and the Commonwealth would lead work under the
auspices of Health Ministers, to report back to COAG in 2011, on the most
effective cancer diagnosis, treatment and referral protocols, to be developed
with expert clinical input[168]
5.185
Subsequently, the National Cancer Expert Reference Group (NCERG),
jointly chaired by the Australian and Victorian governments, was formed, comprising
'senior representatives of all jurisdictions and peak stakeholder bodies ([COSA];
[CCA]; Cancer Australia; and consumer representation)'.[169]
5.186
In July 2012, the NCERG released a National Cancer Work Plan (the Plan),
described as:
...a suite of initiatives, focused on providing appropriate,
efficient and well coordinated care for people affected by cancer and their
families, from diagnosis through treatment and support to the management of
follow-up care and survivorship.[170]
5.187
The three key initiatives of the Plan are:
- Initiative 1 – Pathways of cancer care which will:
a) establish best-practice
pathways of cancer care with agreed referral protocols (including
post-treatment and survivorship) between GPs, cancer specialists and other
allied health professionals; and
b) improve the practical support available to patients, their
carers and families so that they can better navigate the complex cancer
journey.[171]
- Initiative 2 – Efficient and effective cancer services, to
'be achieved by working with consumers, jurisdictions and peak health
professional bodies to establish':
a) the piloting of innovative use of the cancer workforce
including service efficiencies, scope of practice, and new models of shared
care for cancer treatment; and
b) agreed capability frameworks for cancer services with
defined linkages to primary care, regional cancer services and specialist
tertiary teaching hospitals, and the promotion of safe, high quality cancer
care by agreed role delineation for cancer services, specific tumours and
sub-specialties to optimise outcomes.[172]
- Initiative 3 – Evidence-based cancer treatment, which will
promote:
a) better use of multidisciplinary initial assessment and
treatment planning cancer teams across both the public and private sector. The
new National Broadband Network and tele-health technology will be used to
support multi-disciplinary care in regional areas where feasible; and
b) the implementation of new research findings,
evidence-based treatment and care, commencing with the national adoption of the
NSW Cancer Institute’s eviQ database as an easily accessible, consistent,
on-line, point‑of-care treatment resource for cancer health
professionals.[173]
5.188
The Plan also contains the following agreed principles:
- Focus on actions that require national coordination rather
than those that can be achieved by one level of government alone; build upon
existing jurisdictional cancer plans and enhance the current investments made
by all governments within reasonable timeframes.
- Be underpinned by best-practice cancer research and
optimal, evidence‑based cancer treatment and supportive care.
- Recognise the fiscal outlook facing all governments and
the difficulty of funding significant new activity, and focus on high-impact
and achievable actions.[174]
5.189
Cancer Australia, on behalf of the Australian government, implements the
following components of the Plan:
-
a dedicated cancer research budget
-
support for cancer clinical trials
-
the 'Supporting people with
cancer' program
-
the Improved lung cancer data and
treatment guidelines measure.[175]
5.190
Cancer Australia spoke to a few of these components, but did not refer
to the Plan itself. For example, in respect of the 'supporting people with
cancer' component, Cancer Australia informed the committee that it works with
local communities, funding them 'to potentially raise awareness or to provide
supportive care to their communities'.[176]
5.191
Notably, the NCERG's 'future directions' for the 2016–2017 financial
year did not specifically address LSR cancers:
In 2016-17, NCERG will consolidate work undertaken to date in
implementing the National Cancer Work Plan and continue to provide a crucial
forum for coordination of cancer policy and control at a national level. The
focus in 2016-17 will be on implementation of the [Optimal Cancer Care
Pathways] and working with jurisdictions to encourage their uptake. This work
will contribute to consistent cancer care across the country that maximises
efficiencies and builds on the considerable recent investment in cancer
infrastructure by all governments.[177]
5.192
The committee received no detailed information from the DoH or the NHMRC
about how the Plan responds to LSR cancers.
5.193
While the Australasian Gastro-Intestinal Trials Group (AGITG) noted the
work that Cancer Australia is doing to implement the Plan, it nevertheless
recommended a national cancer research plan to specifically address LSR
cancers:
We are aware of several of our States which have produced
comprehensive Cancer Care Plans with stakeholder/consumer input. We are also
aware that Cancer Australia has a National Cancer Care Plan and has allocated
several initiatives to its [NCERG] one of these initiatives is “Evidence-based
care for lung cancer - better lung cancer care - led by Cancer Australia.”
Whilst this initiative is comforting it is not what the AGITG [Consumer
Advisory Panel] considers a comprehensive National Cancer Research Plan which
should, inter alia, include specific research requirements for “low survival
cancers”.[178]
5.194
Indeed, as discussed further in a later section, a number of other
submitters and witnesses called for a plan or strategy to specifically address
the low rates of survival for LSR cancers.
A new strategy for combatting brain
cancer
5.195
On 29 August 2017, the Hon. Greg Hunt MP announced the establishment of
the Australian Brain Cancer Mission (the Mission), a $100 million fund to
combat brain cancer, which:
...aims to double survival rates of people living with brain cancer
over the next 10 years, which hasn’t changed significantly in the past 30
years.
In the long-term our goal is to defeat brain cancer through
world-wide collaboration.[179]
5.196
The Mission:
...is underpinned by a research roadmap developed by Australian
and international experts in brain cancer treatment and research, and those
affected by brain cancer, their advocates and philanthropic interests.[180]
5.197
The Mission will be administered by Cancer Australia, which will be
supported in this work by a Strategic Advisory Group.[181]
5.198
The minister noted that one of the key objectives of the Mission 'is to
ensure every patient, adult and child in Australia has the opportunity to
participate in clinical trials'.[182]
To achieve this, the government will provide $50 million to the MRFF, which
will be supplemented by $20 million from the CBCF and $10 million from the
Minderoo Foundation's Eliminate Cancer Initiative.[183]
The government will also dollar match 'every donation up to $50 million' to
support the mission.[184]
The government expects to 'announce the remaining $20 million in the coming
months'.[185]
5.199
The '[p]rioritised first investments include the establishment of an
Australian arm of the GBM AGILE, an international adaptive trial platform for
adults with glioblastoma' and 'new funding for [ANZCHOG] clinical trial centres
and support [for] the consolidation of the national ZERO Children’s Cancer
initiative'.[186]
International approaches to LSR
cancers
5.200
During the course of the inquiry, the committee received evidence that
specifically identified the US Recalcitrant Cancer Research Act of 2012
(the Act) as an example of how governments can work to increase survival rates
for LSR cancers.[187]
5.201
The Act '[a]mends the Public Health Service Act to require the Director
of the National Cancer Institute (NCI) to develop a scientific framework for
research on recalcitrant cancers (cancer with a 5-year relative survival rate
below 50%)'.[188]
5.202
The framework for research includes:
- a review of the status of research, such as a summary of
findings, identification of promising scientific advances, a description of the
availability of qualified scientific researchers, and the identification of
resources available to facilitate research;
- identification of research questions that have not been
adequately addressed; and
- recommendations for actions to advance research and for
appropriate benchmarks to measure progress on achieving such actions. Requires
the Director to develop the framework within 18 months and review and update it
every 5 years.
5.203
The framework for research also requires the following actions of the
Director of the NCI:
...to identify within 6 months 2 or more recalcitrant cancers
that have a 5-year relative survival rate of less than 20%, and are estimated
to cause the death of at least 30,000 individuals in the [US] per year.
Authorizes the Director to identify additional such cancers and to consider
additional metrics of progress (such as incidence and mortality rates) against
such cancer.
...to convene a working group for each identified cancer to
provide expertise on, and assist in developing, a scientific framework under
this Act.
...to consider each relevant scientific framework developed
under this Act when making recommendations for exception funding for grant
applications.[189]
5.204
Although certain groups in the US, such as the Lung Cancer Alliance and
the Pancreatic Cancer Action Network cautiously welcomed the Act as a result of
their lobbying,[190]
'[a]dvocates for other kinds of cancer research view [the Act] warily':
A man named Jonathan Agin, who lost a small daughter to a
kind of brain cancer with no treatment at all, has been a vocal critic both of
the Act and of the NCI. When he met with representatives of NCI to argue for
more funding of children’s cancers, he was told that funding allocation does
not matter, because discoveries in the lab often apply to many cancers.
...
It’s also the case that the head of the NCI, Dr. Harold
Varmus, is unhappy with the law because he believes it ties the hands of
scientists to determine how money is spent. But others are unhappy with NCI and
think there should be less emphasis on the search for cures and more emphasis
on prevention. NCI’s annual budget requests include billions for research and
treatment, but usually less than $300,000 for prevention and control. It is
argued we are likely to have better results putting money into preventing
cancers to begin with rather than continuing to sink nearly all of our
anti-cancer money into looking for cures.[191]
5.205
CanTeen Australia supported the implementation of similar legislation in
Australia, stating that the Act is:
...an example of how legislative change can support meaningful
coordinated effort to improve outcomes for cancer with low survival rates. It
guides not only the establishment of priority frameworks, but the
accountability mechanisms required to ensure progress, public availability
requirements and how frameworks should be utilised to inform funding decisions.[192]
5.206
The Pancare Foundation also advocated for a national government
commitment mirroring the approach taken in the US, and commended the approach
to improving survival rates for pancreatic cancer currently under development
in the UK.[193]
Mr Barry Westhorpe, Chief Executive Officer of the Pancare Foundation, informed
the committee that the UK All-Parliamentary Group on Pancreatic Cancer is
looking at 'terms of reference based on a framework similar to the US model,
not regulatory as such'.[194]
5.207
With regard to developments in brain cancer in the UK, TBTC informed the
committee that, following a parliamentary inquiry into the funding for brain
tumours:
...the Department of Health was instructed to set up a task and
finish working group to look at this issue. That working group has been taking
evidence for probably about six months now, and the report is due out...there
have been inputs to that across the board from drug discovery symptoms and
various other things.[195]
5.208
TBTC suggested that the work of this committee 'will be a similar sort
of piece' to what is currently happening in the UK in respect of brain cancer.[196]
The UK report is yet to be published.
A national strategy for all LSR
cancers?
5.209
As discussed earlier, the National Cancer Work Plan has no specific
reference to LSR cancers. Further, LSR cancers were not identified as a
specific priority of the NCERG for the 2016–2017 financial year. As the Low
Survival Cancers Alliance has observed, Cancer Australia's Strategic Plan
contains no focus on LSR cancers, supporting the Alliance's statement that 'there
has been no ownership for responsibility for low survival cancers research at a
Federal or state level'.[197]
5.210
Indeed, while COAG did consider a National Rare Diseases Plan in 2013, a
recommendation for such a plan was ultimately not supported.[198]
5.211
A number of submitters and witnesses called for a plan or strategy to be
established specifically to improve survival rates for LSR cancers. Some of
these proposals are discussed in the following section.
A new research plan
5.212
As the Pancare Foundation highlighted, 'there isn't a national strategic
plan to increase survival, nor a definition on what constitutes cancers with
low survival rates'.[199]
It was submitted that, in terms of research, '[t]his translates into
uncoordinated plans instead of a long term, national coordinated approach
across the government, medical, health and research communities'.[200]
5.213
Other submitters and witnesses called for a national strategy to address
funding of research into LSR cancers. For example, Mr Chiem advocated for a
'[n]ational strategy to coordinate planning and funding of cancer research and
reduce the associated administrative overheads', reasoning that:
This will minimise duplication of efforts and reduce the
highly bureaucratic and administrative overhead of research/grant application
and reporting. Funding agencies should also partner to fund like-areas and
capitalise on the economies of scale afforded by the joint funding. A
particular study found that the time spent to prepare for NHMRC proposal
translated into annual salary costs of $66 million. Furthermore, as success
rates of NHMRC grant proposal outcomes are historically 20-25%, there are large
opportunity costs in lost research output.[201]
5.214
Speaking particularly to brain cancer, Mr Barrie Littlefield of CBCF
informed the committee that the mission of the CBCF is to 'increase brain
cancer survival from the current 20 per cent to 50 per cent by 2023', and
stated that:
We need a firm, coordinated plan around this mission. Whilst
more money for research is important, it is also important that the delivery
and allocation of this money when it comes is coordinated, working to a clear,
agreed plan based on our mission, hopefully, both here and internationally.
Australia needs to work to its strengths, do what it does well and not repeat
what is being done elsewhere. It is unlikely that Australia alone will cure
brain cancer, but it can and should play its part.[202]
5.215
Cancer Voices Australia (CVA) opined that 'without a plan we have no
idea where things are headed' and suggested that a national strategic plan for
cancer research would provide greater transparency to consumers and specialists
about the allocation of funding for research.[203]
CVA detailed its proposal:
Such a document, co-designed by key cancer survivors,
researchers and health care providers, would provide greater transparency of
the focus and priorities for research funding. In the absence of a national
plan, the current model of funding is not equitable in allocating funding to
cancers with low survival rates and has resulted in a limited evidence base for
these cancers. A National Cancer Research Plan should embed funding into
cancers with low survival rates and require the establishment of a register for
each cancer. This should include funding for the multiple and cumulative
reasons for low survivor rates, for example, late or incorrect diagnosis, lack
of access to appropriate therapies and clinical expertise, the very limited
number of clinical studies due to the small number of patients and the apparent
lack of interest in developing new therapies due to market limitations.
A national plan should include targets for research into
cancers which currently have low survival rates, while at the same time
providing a national focus for research into all cancers. A national plan
should also support collaborative, baseline work, so necessary in identifying
and prioritising gaps in research with consumers, researchers and health care
providers to set research actions plans for cancers with low survival rates.
Annual reporting to Parliament on progress towards targets in the plan should
be mandatory. In addition it is recommended that the Australian Institute of
Health and Welfare establish routine reporting of the category 'cancers with
low survival rates' to collectively report on the incidence and overall
proportion of mortality contributed by this group, and to track positive or
adverse changes within this group. It is also suggested that as part of this reporting
rare cancers and higher incidence, but low survival cancers, are separately
reported.
A National Cancer Research Plan and associated registry could
provide information to the public about sites where research into cancers with
low survival rates is occurring so that cancer survivors, their carers and the
public can access information about treatment options, and cancer researchers
can see opportunities for collaboration and/or innovation. Cancer Voices
believes a new funding model [should] address identified unmet needs and move
away from clinical trials that propose marginal improvement in care,
particularly as more subsets of cancers are identified.[204]
5.216
CanTeen Australia suggested that the NHMRC could be charged with
developing:
...a scientific framework or multiple frameworks to guide the
conduct and funding of research for the cancers with both low survival rates
and low representation in funding distributions to date. As an organisation,
the NHMRC may be best placed to develop such a framework given its prominent
role in shaping the Australian medical research landscape and working
collaboratively to establish nationally applicable frameworks such as the 2007
National Statement on Ethical Conduct in Human Research.[205]
5.217
CanTeen Australia considered that a collaborative, representative body
could achieve a national strategy for improving outcomes for LSR cancers, and
outlined that such a strategy would assist the NHMRC and MRFF in setting their
funding priorities.[206]
5.218
Similar to CVA, CanTeen Australia advocated for a new framework that
'could include clear accountability mechanisms for monitoring progress on the
strategy and similar requirements for public availability of these strategies'.[207]
Committee view
5.219
The committee welcomes the government's recent funding announcements,
and is particularly encouraged by the investment of $100 million for a 10 year
plan to increase the survival rates for brain cancer. This illustrates the
government's understanding that funding for research is inextricably linked to increasing
survival rates for cancers.
5.220
The committee is concerned, however, by the continued absence of
explicit recognition of LSR cancers, in terms of funding and in government
plans to address cancer in Australia.
5.221
As a result, the committee considers it necessary for a comprehensive
Australia-wide strategy to be developed and implemented to address LSR cancers,
with the explicit goal of increasing the 5-year survival rates for LSR cancers
to above 50 per cent by 2027. The development of such a strategy will require
the participation and commitment of the federal, state and territory
governments, and could be developed via the NCERG and COAG.
5.222
The development of an Australian strategy to improve survival rates for
LSR cancers should take into account the recommendations in this report; must
consult with medical researchers, clinicians, patients and patient groups; and
consider the roles of research, early diagnosis and access to medicines.
International approaches, such as the Recalcitrant Cancer Research Act of
2012 (US), should also be considered and an assessment made as to whether
similar legislation is appropriate in the Australian context.
Recommendation 24
5.223
The committee recommends that the federal, state and territory
governments develop and implement a comprehensive Australia-wide strategy to increase
5-year survival rates for low survival rate cancers to above 50 per cent by
2027:
-
taking into account the recommendations in this report;
-
consulting with researchers, clinicians, patients and patient
groups;
-
considering the roles of research, early diagnosis and access to
medicines; and
-
assessing the applicability of international approaches, such as
the Recalcitrant Cancer Research Act of 2012 (US), to the Australian
context.
5.224
The committee further recommends that annual progress reports on the development
and implementation of an Australian strategy to improve survival rates for LSR
cancers are provided to COAG's Health Council and made publicly available.
Recommendation 25
5.225
The committee recommends that annual progress reports on the
development and implementation of an Australian strategy to improve survival
rates for low survival rate cancers are provided to the Council of Australian
Governments Health Council and made publicly available.
Senator
Catryna Bilyk Senator David Bushby
Chair Deputy
Chair
Senator
Brian Burston Senator Stirling Griff
Pauline
Hanson's One Nation, NSW Nick Xenophon Team, SA
Senator Jane
Hume Senator Chris Ketter
Liberal
Party of Australia, VIC Australian Labor Party, QLD
Senator
Malarndirri McCarthy Senator Dean Smith
Australian
Labor Party, NT Liberal Party of Australia, WA
Navigation: Previous Page | Contents | Next Page