Assistance and support for veterans
Introduction
4.1
An area of unanimous agreement in this inquiry is the utmost importance
of individuals who are unwell being able to access appropriate support and
assistance. The role of both the Department of Defence (Defence) and the
Department of Veterans' Affairs (DVA) in offering and providing support and
assistance was a key focus in much of the evidence received by the committee.
4.2
The committee spoke with some veterans who were clearly in need of
immediate assistance and many of these individuals had been trying to access
support for some time. As noted earlier in the report, the committee was pleased
that representatives from DVA were in attendance at hearings and available to
provide assistance and support to individuals and families in immediate need if
they wished to speak with them.
4.3
This chapter discusses the matters raised with the committee in relation
to the provision of assistance to veterans, with particular reference to
assistance with their health concerns. It covers the actions taken to date by
Defence and DVA; veterans' experiences with accessing assistance; barriers to
accessing assistance; the assistance and support being sought; and addressing
veterans' concerns moving forward.
Summary of Government actions to date
4.4
As noted in Chapter 1, this committee tabled the report, titled Mental
health of Australian Defence Force members and veterans, on 17 March 2016. The
report included two recommendations in relation to mefloquine.[1]
4.5
Responding to the committee's recommendations from the report, on 15 September
2016, the Minister for Veterans' Affairs, the Hon Dan Tehan MP announced that
the government would:
-
establish a formal community consultation mechanism to provide an
open dialogue on issues concerning mefloquine between the Defence Links
Committee and the serving and ex-serving ADF community;
-
develop a more comprehensive online resource that will provide
information on antimalarial medications;
-
establish a dedicated DVA mefloquine support team to assist our
serving and ex-serving ADF community with mefloquine-related claims, which will
provide a specialised point of contact with DVA; and
-
direct the inter-departmental DVA-Defence Links Committee to
examine the issues raised, consider existing relevant medical evidence and
provide advice to the Government by November 2016.[2]
4.6
With particular reference to these actions identified by the Minister
for Veterans' Affairs, the committee asked witnesses at its public hearings in
Brisbane and Townsville for their perspective on the progress of
recommendations. While noting that witnesses would likely be unaware of the
DVA-Defence Links Committee action, it was disappointing to note that several
witnesses indicated they were completely unaware of the other actions.[3]
4.7
Following the hearing, Senator Alex Gallacher wrote to the Minister for
Veterans' Affairs, the Hon Darren Chester MP, seeking advice on the progress of
the announcements from the Government.
4.8
On 18 September 2018, the Minister wrote to the committee and included
the following update:
With respect to the commitments made by the then Minister for
Veterans' Affairs, the Hon Dan Tehan MP, I can advise these have either been
met or are ongoing. I draw the Committee's attention to the submission to the
inquiry from DVA which provides more information about services and supports
available to veterans and their families; and the future action plan involving
further outreach, communications and research in this area.[4]
4.9
While it is disappointing that there was little awareness of the response
to the recommendations within the community the actions were designed to assist,
the committee is aware that Defence and DVA have both undertaken a series of key
actions in response to the issues and concerns raised about antimalarial use
which are outlined below and throughout the chapter.
Department of Defence response
Key message
4.10
Defence has indicated that its response to concerns about the use of
antimalarial drugs has 'been designed to provide current and former serving
members with information about the medications of concern, detail on the
studies, and to encourage them to seek help'.[5]
A key message from Defence has been to encourage individuals with concerns to
consult their treating medical practitioner and to consider putting in a claim
with DVA.[6]
4.11
On 30 November 2015, Defence issued a statement on the use of mefloquine
in the ADF and advised that 'if any ADF member, past or present is concerned
that they might be suffering side-effects from the use of mefloquine defence
encourages them to raise their concerns with a medical practitioner so they may
receive a proper diagnosis and treatment'.[7]
Comprehensive website
4.12
In February 2016, VADM Griggs told the Senate Foreign Affairs, Defence
and Trade Legislation Committee about the need for their actions to balance the
provision of information with the need to avoid causing undue concern for
people who are well:
I would like to make the point that we are now in about month
7 of a pretty sustained media campaign about mefloquine. What we have been
trying to do is to get out as much information as possible in as transparent a
manner as possible to allay the fears of serving and former serving members of
the ADF about the use of this drug, because the nature of the reporting and the
nature of this campaign has elevated concern levels amongst people who do not
need to be as concerned as they now are. We are actually quite concerned about
that. One of the things we have just completed is a series of web pages, which
is now available on the Defence internet site, which I think is a very
comprehensive and transparent articulation of all the issues around
antimalarials, not just mefloquine, in use in the ADF.[8]
4.13
In order to provide information to concerned veterans and their
families, Defence developed a comprehensive external website on malaria,
mefloquine and the ADF and established an email address where individuals can
request further information.[9]
Information for families
4.14
Defence advised that information for families concerned about
antimalarial use continues to be available by contacting the dedicated email
address as well as accessing information from their website.[10]
4.15
In its submission Defence also described other support services
available to families for a variety of reasons and not specifically related to
concerns about antimalarial use such as the ADF Family Health Program, the
All-hours Support Line, the Defence Family Helpline and the Veterans and
Veterans Families Counselling Service (VVCS).[11]
Research
4.16
To inform its ongoing response to these issues, Defence has undertaken
or commissioned research into a number of matters relating to its use of
antimalarials and in particular mefloquine, including:
-
a review of Medical Employment Classification outcomes of those
who participated in the Timor-Leste trials. This has shown no significant
differences in the incidence of becoming medically unfit for service, or
diagnosis of PTSD between those who were prescribed mefloquine and those
prescribed other anti-malarial medications;[12]
-
a comprehensive literature review on mefloquine commissioned from
Professor Sandy McFarlane AO, Director of the University of Adelaide Centre for Traumatic Stress Studies;[13]
and
-
commissioned (jointly with DVA) the University of Queensland to
undertake a research study involving the re-analysis of health study data on
anti-malarial use from the 2007-2008 Centre for Military and Veterans' Health
deployment health studies.[14]
Further information on this is outlined below.
Department of Veterans' Affairs
response
Mefloquine support team
4.17
In accordance with the government commitment announced in September
2016, DVA established a dedicated mefloquine support team within their claims
area to respond to inquiries about mefloquine. DVA advised the committee that
the team 'did not receive many calls' and that team was subsequently put onto
other duties within the claims area. In September 2018, DVA added information
to their phone line, prompting callers to dial zero to speak to someone in
relation to mefloquine but again they did not receive many calls.[15]
Support for GPs
4.18
DVA has provided information to general practitioners (GPs) to assist them
to provide support to veterans who may have concerns about mefloquine:
-
DVA's Principal Medical Adviser wrote to all GPs on 30 September
2016 and to the Primary Health Network in October 2016 to bring information about
mefloquine to their attention;[16]
and
-
DVA organised and hosted a briefing with GPs in Townsville on 29
November 2016.[17]
Information event
4.19
In December 2016, DVA held an event, referred to as an 'outreach program',[18]
in Townsville which was attended by more than 90 members of the community
concerned about antimalarial medications such as mefloquine. Defence supported this
event.[19]
As noted earlier, the government committed to establishing a formal community
consultation mechanism on issues concerning mefloquine and the Townsville 'outreach
program' was the first step.[20]
Support for families
4.20
DVA provides support to veterans' partners and families through funding
a range of health services as well as the front line mental health services
provided through Open Arms—Veterans and Families Counselling (formerly VVCS).[21]
DVA's Future Action Plan
4.21
In its submission, DVA noted it has 'prepared an action plan to address [veteran]
community concerns about potential effects of mefloquine that includes outreach
activities, communications and research'.[22]
Following the outreach program conducted in Townsville in December 2016 (in
collaboration with the Repatriation Medical Authority (RMA), VVCS and with the
support of Defence), DVA is conducting consultation forums across other capital
cities. The submission noted that these will be publicised through
advertisements in newspapers and services newspapers, as well as direct
invitations to relevant organisations, and individuals where possible.[23]
4.22
Ms Liz Cosson AO CSC, Secretary, DVA, provided further detail about
these consultation sessions at the hearing in Canberra. A series of sessions
were planned in different locations throughout October and November. Further
sessions in different locations would be considered should there be sufficient
demand.[24]
These consultation forums are further discussed later in the chapter.
DVA funded health treatment and
compensation claims
4.23
The support provided to veterans who have been injured or suffered
illness as a result of their service (including illness or injuries related to antimalarial
medication) fall broadly into three categories—compensation, income support and
health treatment. To access compensation and income support, a veteran needs to
make a claim and show to the relevant standard of proof that they have suffered
an illness or injury, and demonstrate that this condition was related to their
service.[25]
4.24
In relation to health treatment, there are two pathways by which
veterans may access DVA-funded services:
-
Under the non-liability pathway, veterans can apply for
access to treatment for mental health conditions without the need to show that
the condition is related to service.
-
Under the liability pathway, veterans can make a claim
which DVA will then assess to establish whether the condition was related to
service. If the claim is accepted, the veteran's entitlement to compensation
and income support will then be assessed, and the veteran will be eligible for
DVA-funded health treatment for the condition.[26]
4.25
In addition, all former serving personnel can access a comprehensive
health assessment from their GP.[27]
Independent of the claims process, mental health services are also available
from Open Arms—Veterans and Families Counselling to all current and former
serving personnel.[28]
4.26
Serving and ex-serving ADF members can claim compensation at any time
for medical conditions they believe are related to their service. For DVA to
accept liability for compensation there has to be a causal link determined
between the person's service and their medical conditions. Under the Veterans'
Entitlements Act 1986 (VEA) and the Military Rehabilitation and
Compensation Act 2004 (MRCA) the potential link between a medical condition
and service is assessed using Statements of Principles (SOPs).[29]
SOPs are discussed later in this chapter.
Veterans' experiences with accessing assistance
4.27
The committee explored with individuals their experiences of accessing
assistance; whether they had tried to access assistance, and if so, the details
of that experience. The committee also spoke to veterans who had not accessed
assistance and explored the reasons why not, as well as the assistance they are
seeking.
Veterans who are accessing services
and receiving help
4.28
Some individuals appeared to be accessing assistance. While
acknowledging it had taken some time to access, Mr Mark Armstrong
described the services he is receiving:
I have access to a neurologist and a neuropsychologist, a
psychiatrist and a psychologist because of my PTSD tag, so I'm able to get
certain treatments through that. Other things like my brain injury—my eighth
cranial nerve is 31 per cent more damaged on my right-hand side than on my
left-hand side. As I was walking, I'd fall to my right, so I went and got that
tested. That was through the PTSD as well. I suppose I'm one of the lucky
ones—because I have a TPI [Totally and Permanently Incapacitated] gold card I
have access to a lot of different medical things that other people don't.[30]
4.29
Another submitter explained their experience as follows:
My health conditions are accepted by DVA and I consider I
have been well looked after with treatment, hospitalisation and incapacity
payments. My military super was converted to an invalidity pension at
discharge. None of my accepted conditions contain reference to Mefloquine
although my medical documents do so.[31]
Families/partners
4.30
A small number of partners and family members also advised that they
have accessed some support services through DVA, including counselling services
from Open Arms.[32]
While some indicated that support had been of some assistance, others reported
that the experience had not been helpful.[33]
4.31
However, Mrs Susan Armstrong spoke positively about her participation in
the Female Veterans and Families Forum. While she noted there is limited
opportunity to discuss personal circumstances in detail due to the number of
issues in these forums, it did provide an opportunity 'to get to [speak to] someone
in a meeting break'.[34]
Veterans who are getting assistance
but believe it is not working
4.32
Some veterans explained that while they are receiving help, their
current treatment and support has not been very successful in improving their
health.[35]
4.33
Mr Stuart McCarthy explained that although some of his claims to DVA for
issues such as depression and anxiety have been accepted, the available
treatment predominately consisted of medication which has not been of great benefit.[36]
4.34
Mr Aaron King advised that he was classified as Totally and Permanently
Incapacitated (TPI) some years ago and been diagnosed with PTSD but that the
treatment he has received to date has not been effective:
I'm TPI. I was made TPI years ago, not as a part of this [use
of antimalarials]. We only just found out about this a couple of years ago,
about the symptoms. It was put down to PTSD for me. I've got lots of side
effects and problems. It's always just been put down to PTSD. Treatment-wise,
there's Ward 17 at Heidelberg. Now they don't really want me to go, because
they've exhausted all avenues. There's no treatment. I've had [Electroconvulsive
Therapy and Transcranial Magnetic Stimulation] ECT, TMS [Transcranial Magnetic
Stimulation] and pretty much every medication. I've been in and out of psych
wards. I've been thrown in jail because they felt there was no other safe place
for me at times.[37]
4.35
Mrs Naomi Kruizinga explained that the medications given to her husband,
Mr Michael Kruizinga, have not helped:
Many times before, Michael has been given a bandaid, or a
temporary fix, to stop his suicidal ideation—more mood stabilisers under the
PTSD umbrella—with most of his network of psychologists and psychiatrists
linking it to just severe depression. Yet he suffers from the neurotoxic
properties of these drugs that were given. None of the medications have worked
since he commenced them over a year ago. If anything, they have made him worse.[38]
Veterans who are not receiving or
seeking assistance
4.36
Worryingly, some veterans told the committee that they are not accessing
help from DVA. In some cases, this was due to a lack of trust in the process.
In other cases, it was suggested that veterans do not have a diagnosis and/or
have not been able to access treatment and support because the effects of
antimalarial medications are not recognised under a single SOP. This is further
discussed later in the chapter.
4.37
Ms Anne-Maree Baker explained:
I have not used the phone lines and made claims for
compensation with DVA because I am undiagnosed. None of my illnesses are
attributed or connected to this trial because nothing has been reported
correctly.[39]
4.38
Mr Stuart McCarthy told the committee
that he has submitted claims for cognitive impairment which have not been
accepted. Further to this, Mr McCarthy stated:
...What's not happening—we are being
refused the support (a) that we need and (b) that we have actually asked for.
And that's exactly the situation that I'm in.[40]
4.39
Other veterans also discussed this issue. Mr Wayne Karakyriacos reported
that '[a] lot of veterans have gone bush and a lot of them are hiding'.[41]
Mr Desmond Rose told the committee that 'most of us don't contact DVA about
tafenoquine anyway...'.[42]
4.40
One veteran, Mr Brian Carlon, is receiving assistance but reported that
dealing with DVA is difficult:
Everything I've done with DVA is a fight, and that fight
takes its toll. I have nothing to do with DVA except: when they send me a
letter, I will send it back. I don't ring them. I don't contact them. It's too
hard on me, because it is a fight.[43]
Barriers to accessing assistance
4.41
As the committee was told that assistance is available and some
witnesses described their experiences of positive support, the committee
explored the reasons why some veterans are not accessing support. These
include: ADF cultural issues, lack of information and difficulties navigating
the claims process.
Cultural issues
4.42
As briefly noted in Chapter 3, some veterans suggested that the nature
of the ADF environment means it is difficult to report health concerns or to
question authority for fear of showing weakness and the potential impact on
career progression.
4.43
On a similar theme, some veterans reported that it is difficult to ask
for assistance. Colonel Ray Martin (Rtd) explained as follows:
Certainly in my experience, and you've heard it today, men
and women in the ADF are self-reliant and very well trained. They're kind of
tough on the outside. As soon as they admit there's a mental health issue, even
though the system says 'come seek help', the reality is you think that if you
put up your hand there's a career detriment to that.[44]
4.44
Mr Rose told the committee that he has only recently started to seek support
for PTSD due to the challenges of seeking help:
It's something you don't like to admit. It's a bit hard,
being a man and saying you've got mental problems. It's not the best.[45]
4.45
Mr Kruizinga acknowledged these cultural issues and suggested that there
needs to be more assistance when a soldier transitions to civilian life.[46]
Lack of information
4.46
Mr Colin Brock reported that information about the trials has not been
shared between Defence and DVA:
I guarantee DVA doesn't know that we were on mefloquine or tafenoquine.
How does DVA know? Defence hasn't told them. We haven't told them.[47]
Mefloquine support line
4.47
As outlined earlier in the chapter, DVA established a dedicated
mefloquine support line to assist veterans who were concerned about
antimalarials. Veterans and their families told the committee about their
difficulties getting advice from this dedicated team.[48]
4.48
Mr Mark Armstrong explained his experience seeking information via the
DVA dedicated mefloquine line:
They [DVA] told me that they didn't have a list of mefloquine
users and to contact the Department of Defence. They did give me a number for
that, and the Department of Defence told me to contact DVA. So I contacted DVA,
and we went back and forth a few times. There was supposed to be some special team
that looked after it. Then, after a while, a lady rang me back, and she was in
a special team—I think they call it a special team or something along those
lines—who don't just look after mefloquine; they look after anything special.[49]
4.49
In a supplementary submission from the Australian Quinoline Veterans and
Families Association (AQVFA), Mr McCarthy described his experience contacting
the dedicated mefloquine support team in DVA. Mr McCarthy details two phone
calls he made to the dedicated number in August and September 2018 seeking
information about the ADF use of tafenoquine. On both occasions, officers were
unable to provide responses to questions. He reported:
The 'dedicated mefloquine support team' was announced by DVA
in 2016. The DVA Secretary has stated that this dedicated team and toll free
number are part of her focus 'on the treatment for veterans who need
assistance', however the staff of the 'dedicated mefloquine support team' do
not hold contact information for healthcare providers and are unaware of the
most basic, factual information regarding the ADF's use of mefloquine and
tafenoquine.[50]
4.50
Following feedback from veterans, the committee was told that DVA made
additional changes to the support line in October this year. The mefloquine
support line is now answered by a team in Canberra that comprises:
...some higher-level staff that actually understand the
detailed nature of our SOPs and who can help any veteran that phones that
dedicated line to assist with their claims—particularly to assist them to
access treatment. [51]
DVA claims process
4.51
The committee heard about the difficulties experienced by some submitters
trying to navigate the DVA claims process, and that some veterans and their
families found it daunting or demoralising.[52]
Some witnesses explained that they were assisted to submit their claims by an
advocate but even with such assistance, veterans provided examples of the
claims process taking up to 10 years.[53]
4.52
The committee heard that support is available to assist to navigate the
claims process. For example, Ms Cosson, Secretary of DVA, told the committee:
We're happy to sit down with a veteran and help them put
forward what they are claiming. Certainly in the...consultation—that we had in
Adelaide and we propose having around the country, where a veteran does
present, which happened in Adelaide, we're able to sit down with them and help
them through the claiming process.[54]
4.53
Professor Nick Saunders AO, Chairperson of the Repatriation Medical
Authority (RMA), emphasised the importance of using an advocate to help
navigate the system:
...there are a lot of veterans who actually could establish a
causal link between their service and their health today if they actually went
through it in a systematic way with their advocate and looked at a range of
statements and principles and a range of conditions that they might have. For
example, we have a statement of principle for post-traumatic stress disorder.
Indeed, the people who are advocating for chronic brain injury being caused by
mefloquine say that there is significant overlap in the symptoms and there's
confusion in the system. Well, if one does have post-traumatic stress disorder,
it almost certainly will be able to be related to the service, and it will be
able then to related to access to appropriate treatment and
compensation—although...access to treatment is less of an issue now [that the
non-liability pathway has been established].[55]
Liability and non-liability pathways
4.54
As previously noted, veterans may access DVA-funded services through two
pathways. DVA stressed to the committee that there is help available to
veterans in need under the non-liability pathway which does not need to be
connected to service-related activities:
In relation to any treatment for anything that's part of the [Diagnostic
and Statistical Manual of Mental Disorders, Fifth Edition] DSM-5, which is
anything to do with a mental health condition, which includes brain injury, our
veterans are eligible for free treatment. There are two pathways to get
treatment with the Department of Veterans' Affairs. The first is through that
non-liability line, where you don't need to prove your condition is related to
service, and we will get you straight into treatment.[56]
4.55
Mr Kruizinga was positive about the establishment of the non-liability
pathway:
In recent times, DVA have added a new strain of help that
they call 'non-liability health care'. I believe this is a great step
forward—it means that any soldier can then go and find help for their mental
health—but I think that's a DVA umbrella trying to hide the issue that we are
talking about today.[57]
4.56
Mrs Kruizinga described how this change made a difference to the
circumstances of her husband and family:
When he was admitted into psychiatric in February for a
month, he was only on the white card at that stage. I had to fight tooth and
nail to keep him there, and they were wanting us to pay the cost, which was
quite exorbitant. I was going to have to pull him out, because there is no way
we could afford that. I think a week into his stay, this non-liability kicked
in, which was great...otherwise I would have had to pull him out.[58]
4.57
Alternatively, veterans can submit claims through the liability pathway.
DVA assesses these claims to establish whether the condition was related to the
claimant's service. Claims are also assessed against Statements of Principles
(SOPs). These inform decisions regarding claims for compensation or liability
for service injuries, diseases and death under the legislation relevant to DVA.[59]
SOPs are set out by the RMA, which noted that SOPs 'state the factors which 'must'
or 'must as a minimum exist if service is to be accepted as contributing to a
particular kind of disease, injury or death'.[60]
Professor Saunders emphasised that:
If an exposure can be causally related to a disease or injury
then it can become a factor within a statement of principles, but we do not
make statements of principles relating to exposures to drugs, toxins or those
sorts of things.[61]
4.58
DVA explained that when a veteran makes a liability claim in relation to
the use of antimalarials, it is necessary for DVA to establish that:
-
the claimant had a diagnosable condition answering the claim;
-
the claimant had taken a relevant antimalarial medication;
-
the relevant SOPs (if one has been determined by the RMA)
includes a causal factor relating to the use of that medication;
-
any other requirements set out in the SOP factor are met; and
-
the use of the antimalarial medication was related to the
person's service.[62]
Statements of Principles with
factors relating to mefloquine or tafenoquine
4.59
DVA advised that the RMA has included mefloquine and tafenoquine, either
by name or in more general terms, as a potential causal factor in the SOPs for
a total of sixteen conditions: 16 for mefloquine and six for tafenoquine.[63]
The RMA told the committee that they:
...are confident that we have included mefloquine or
tafenoquine in statements of principle for all diseases or injuries which could
be linked to taking these drugs based upon sound medical scientific evidence
that meets standard epidemiological criteria when examining things for
causation.[64]
4.60
The RMA noted that 'the wording of the mefloquine- or
tafenoquine-related factors in these SOPs requires a close temporal link
between the taking of the drug and the onset of the condition...reflecting the
well-accepted evidence that these agents can have acute neuropsychiatric
effects'.[65]
Ms Cosson suggested that if a trial participant reported an adverse event
during the trial, DVA may be able to use Defence's records to assist with
establishing this temporal link required by the SOPs.[66]
4.61
As noted in Chapter 2, Professor Saunders emphasised that the RMA takes
a very generous view of evidence when they write the SOPs.[67]
Therefore in his view the key for many veterans is getting assistance from an
advocate for example to establish a causal link between their service and their
current health conditions as:
...when the department has conducted reviews in the past about
claims that have been turned down or groups of claims being turned down for a
particular injury, when one looks through the list, there are many other
factors whereby those people could have legitimately claimed and got access to
compensation through the standard route. So there is access to the system. The
statements of principles cover 94 per cent of the claims that are made in the
department, and there is a higher rate of success for claims based on a
statement of principle than for those six or so per cent of claims that are
made, really, not based on statements of principle but relying upon medical
opinion, and the like. So the system is there for people to be able to gain
access to the outcomes of the system and assessment.[68]
4.62
Acknowledging the chronic and complex symptoms being presented to the
committee, Professor Saunders also raised the SOP concerning 'chronic
multisymptom illness' determined in 2014:
We have a statement of principle on an illness called chronic
multisymptom illness. This arose out of an inquiry that we conducted in
relation to Gulf War syndrome. Although this did not satisfy the Gulf War
advocate group that was presenting to us, it became quite clear to us that
there were a significant number of veterans who had quite debilitating symptoms
that fitted into particular patterns of illness, but this wasn't related just
to serving in the Gulf War. In fact, it was related more broadly to deployment
into hazardous environments. So we wrote a statement of principle called
'Chronic multisymptom illness'. That statement of principle is available today
for those people who were deployed to, say, East Timor, took antimalarial drugs
and now have debilitating symptoms that are broad-ranging.[69]
Antimalarial-related claims
4.63
DVA 'has maintained a record of specific claims relating to antimalarial
medications since September 2016'.[70]
As of 30 July 2018, 42 veterans had lodged 53 claims since reporting commenced.[71]
As at 15 October 2018, DVA had received claims from 44 veterans from a total of
71 conditions 'that have been contended as relating the use of antimalarial medications'.[72]
DVA detailed the outcome of the 71 conditions considered:
-
29 have been accepted either consistent with the original claim
or as relating to a different SOP;
-
24 have been rejected as either not meeting the requirement of
the SOP or there being no diagnosed condition as claimed;
-
six have been withdrawn by the veteran; and
-
12 are in progress.[73]
4.64
The veterans who made these claims were deployed to a range of locations
as follows: East Timor (30 veterans), South East Asia (four veterans),
Australia-Pacific region (five veterans), Middle East (two veterans), Africa
(one veteran) and two veterans from an unspecified location.[74]
The following table shows which antimalarial medications were being attributed
by the veteran as the cause of the condition being claimed, and the outcome of
the claim.[75]
Table 2: Outcome of claimed condition by antimalarial
medication
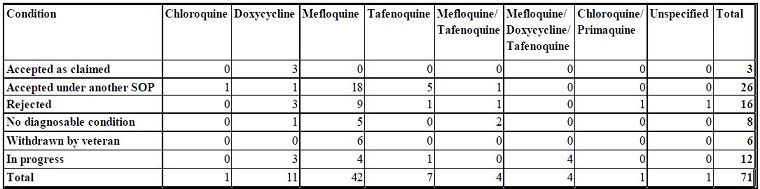
Source: DVA, Response to
questions on notice from 11 October 2018 public hearing (received 1 November
2018), [p. 6].
Further investigation of claims by
DVA
4.65
At the hearing on 11 October 2018, Ms Cosson noted that DVA are 'looking
at each individual client claim to understand what the claim was that they were
seeking and to try and understand a little bit further about why they were not
accepted'.[76]
Claims team
4.66
On notice, DVA provided information about the composition of the claims
team:
The dedicated Complex Case Team in the Melbourne office
consists of seven delegates (three APS6 and four APS5) supported by an EL1
Assistant Director, a contracted medical advisor and two social workers. The
team previously consisted of four delegates and was increased to seven
delegates when combined with the Mefloquine Claims Team. The delegates in the
team are experienced and have expertise across the Veterans' Entitlements
Act 1986, the Safety, Rehabilitation and Compensation (Defence-related
Claims) Act 1988 and the Military Rehabilitation and Compensation Act
2004. Mefloquine or other anti-malarial drugs claims receive a higher level
of priority and all calls relating to these claims are handled by the Complex
Case Team.[77]
4.67
DVA further advised that of the seven delegates processing claims, five
have been in the team for greater than 12 months. The team also processes
claims relating to physical and sexual abuse in the ADF and 'given the nature
of these claims delegates are rotated after about 12 months'.[78]
What assistance and support are veterans seeking?
4.68
Given the range of challenges highlighted by veterans and their
families, the committee explored what other assistance and support is being
sought in relation to their health. A range of suggestions were put forward
throughout the inquiry including: acceptance that use of mefloquine and
tafenoquine are the primary cause of the veterans' health issues, improved response
times by Defence and DVA, information and support for families, a proactive
outreach program and tailored treatment programs.
Acceptance of antimalarials as the
cause of health issues
4.69
A number of witnesses called for the use of mefloquine and tafenoquine
to be recognised as the sole or primary cause of the veterans' ill health. Mr Kruizinga
distinguished this from the current situation:
...although DVA have added mefloquine and tafenoquine as the
basis for several SOPs, as a contributing factor, I do not believe yet that DVA
have acknowledged that mefloquine can be a sole factor.[79]
4.70
The AQFVA submission similarly advocated:
That an SOP be established for chemically acquired brain [injury],
quinolone poisoning or similar, to facilitate claims and compensation for
veterans and their families exposed to these drugs during ADF clinical trials
or general military service.[80]
4.71
Lieutenant General John Caligari AO DSC (Rtd), a commanding officer
during the tafenoquine prevention trial, also stated:
In my view, there is sufficient evidence to acknowledge that
mefloquine and tafenoquine are the cause of significant suffering among them. I
believe much more can be done, and needs to be done, to help them...I would like
to see four outcomes from this inquiry: acknowledgement that it is possible
that mefloquine and tafenoquine have an adverse effect on the mental health of
some service personnel and that the treatment may be different to the common
treatments for PTSD; commencement of suitable research to understand how best
to treat those who have experienced adverse effects from the use of mefloquine
and tafenoquine; initiation of a program to identify every service person who
has been prescribed mefloquine and/or tafenoquine and has been adversely
affected by those drugs; and alerting the treating GPs and mental health
practitioners of these individuals that these people need to be dealt with
under a common protocol as directed by DVA and not automatically treated with
PTSD.[81]
4.72
Dr Remington Nevin told the committee:
[A] veteran can derive a significant amount of relief simply from
learning that it's not all in their head; that they're actually sick from a
disease with a name that doctors recognise. I don't think the amount of relief
that comes from simply having their lifelong concerns finally validated can be
understated. Many veterans have suffered with this problem for 25 years. To be
finally told that what they suspected all along is true, that their government
unintentionally or unwittingly poisoned them, can itself be deeply therapeutic.[82]
4.73
Associate Professor Jane Quinn provided her view
...until that acknowledgement is there, it doesn't really
matter what we put in place—that system is still going to ignore that it
exists, and that's always going to be a problem.[83]
4.74
Some of the family members of veterans participating in the inquiry also
highlighted their desire to see the antimalarials publicly recognised as the
primary or sole cause of the ill health experienced by veterans. Mrs Susan
Armstrong, the wife of veteran Mr Mark Armstrong, explained to the committee
that while they were not interested in assigning blame or looking for financial
compensation, they hoped the inquiry could provide:
...acknowledgement and acceptance of the existence of the
permanent adverse health effects of mefloquine; education of medical doctors
and specialists so they understand the permanent adverse health effects that
can arise; funding for long-term studies and research into methods or tests for
detection of toxicity and how to treat to mitigate the adverse health effects;
real and practical support for the veterans and their families; and legislation
prohibiting the testing of drugs on ADF personnel.[84]
4.75
At the public hearing in Melbourne, Mrs Raelene King cautioned:
I find that if this isn't acknowledged—that tafenoquine and
mefloquine have caused this problem—this is not going to move forward. It needs
to be acknowledged that this is the cause of our problem. Without
acknowledgement, it's not going to move forward.[85]
Improving response times
4.76
The committee also heard the view that Defence and DVA should respond
more quickly when contacted by concerned veterans. Mr Benjamin Whiley explained
that he waited two months to receive information from ADFMIDI about the
medication he had taken and then several months to get an appointment with a
doctor and then another four months for the recommended brain injury
rehabilitation program to be approved and commence. Mr Whiley was concerned
about the impact this sort of timeframe can have on veterans' health.[86]
4.77
The need for a timely response to assist veterans was noted by Mr Kel
Ryan, National President, Defence Force Welfare Association:
I have quite a deal to do with DVA in another capacity, and I
would agree that DVA is becoming a lot more responsive than it was 10 or 15
years ago. But the fact that we're only now addressing this very issue, 15 or
30 years after the event, means, to me, we have to become a lot more agile with
the way we deal with these issues. I know enough about soldiers and soldiering
to say that people present with issues, often, many years after they've left
the service, and they present because of triggers that might not have occurred
20 or 30 years ago that have suddenly occurred. So somehow or other we need to
get a more agile process to deal with these issues.[87]
4.78
As noted above, some claims, even with the assistance of an advocate,
have taken up to 10 years to be finalised. Some individuals the committee spoke
to were clearly in need of more immediate assistance.
Information and support for
families
4.79
As has been raised in other inquiries undertaken by this committee,
support from the partners and family members of veterans is very important.
Several veterans who provided evidence to this inquiry did so alongside
partners, parents and other support people. Similar to the experiences of the
veterans themselves, family members reported difficulties accessing information
about the ADF trials, veterans' health records and any support that may be
available.
4.80
Mrs Naomi Kruizinga, wife of a veteran, outlined some challenges her family
experienced when in crisis.
I was completely overwhelmed. I had three children trying to
make sense of what had happened and unable to give their dad a hug at night. I
had to keep going, and I was the only bread winner. There was no assistance
from DVA. They couldn't do anything. Except offer a one-time payment of 900
[dollars] to tide us through. We have had to get food vouchers from RSL and
bravery trust to get us [by]. Hock personal belongings to help us through. Why
is there no help from your government for this? I am not the only family who is
going through this right now.[88]
4.81
In addition to providing counselling services, Mrs Kruizinga asked that
more coordinated support be available for families:
Especially for the children as well—they do give us
counselling, but there needs to be sort of a team involved that will come out
and help assess each family individually and try and find out what supports
they need, whether it's financial assistance, other things as well. There's
no-one out there like that. We have to make the calls. When you're so busy
dealing with him in hospital—I don't have the time and I have three children
whose needs I have to look after as well. Having that team come in and help me
would be highly beneficial, just to take that load off.[89]
4.82
The role of ex-service organisations was also discussed. Mr and Mrs
Kruizinga explained that their children had attended 'highly beneficial'
support programs with Legacy and also accessed some services from the RSL. Mrs
Kruzininga explained that because there is no coordination between ex-service
organisations, as well as with DVA, family members must approach each service
individually to find out what assistance is available.[90]
4.83
When describing her experience, Mrs Raelene King also advocated for more
support for children to be available:
I would also perhaps like to see a quinoline support group for
all children of affected trial participants to establish what the impact these
psychological effects have had on them. My children are adolescents and adults
now. Personally, seeing my husband go through this has affected me deeply in so
many ways. So try to imagine seeing this through the eyes of my children.[91]
Proactive outreach program
4.84
Several submissions and witnesses advocated for a proactive outreach program
to be initiated whereby all trial participants are contacted individually to
inquire about their health and to check whether support or assistance is
required.[92]
For example, Mr Benjamin Fleming, a veteran who participated in the
mefloquine prevention trial, was supportive of a broad outreach program
because:
...there are a lot of people out there who don't know they have
got the issue....Defence and DVA, et cetera, have in their means the ability to
contact every individual who has consumed these drugs. The first step is very
much to reach out to them and help educate.[93]
4.85
He called for a program 'funded to speak with every Defence Force member
who consumed these drugs—not just one that focuses on sufferers in Townsville'.[94]
Also appearing at the public hearing in Brisbane, Mr Whiley agreed that an
'outreach program is vital' and that such a program 'needs to occur at a faster
priority'.[95]
4.86
The AQFVA called for the establishment of a working group:
...encompassing veterans advocates experienced in the effects
of quinoline toxicity with appropriate, independent advisers sourced from the
military mental health community, family services, occupational health
practitioners, brain injury rehabilitation specialists, neurologists,
psychologists, cognitive and behavioural experts and psychiatrists, to
establish a recommended assessment and treatment program for those affected by
mefloquine and tafenoquine during their military service.[96]
4.87
It further suggested that such a group 'be appropriately resourced to
deliver a national outreach and rehabilitation program for quinoline veterans
and families in Australia'.[97]
The AQVFA submitted a proposal to then Minister for Veterans' Affairs, the Hon
Dan Tehan and DVA in December 2016 to direct a pilot outreach, rehabilitation
and research program for quinolone veterans and families.[98]
The AQVFA's outreach program proposal was supported by other participants in
the inquiry.[99]
Mrs Kruizinga emphasised that a broad ranging outreach program would also be
able to provide assistance for families and advise about other support
services:
This is where having this outreach program that can do the
advocacy and the support and all that for the families is really beneficial,
because it's just too overwhelming. I'm just so focused on the children and my
husband that I just don't get the time to do that.[100]
4.88
Associate Professor Quinn told the committee that when responding to the
proposal from the AQVFA, Minister Tehan did not support the proposal and noted
that there are existing services available through DVA, or through Defence for
serving members.[101]
4.89
Dr Remington Nevin noted that the American Quinism Foundation has recommended
that all recent American veterans be screened for a history of symptomatic
mefloquine exposure.[102]
Tailored treatment programs
4.90
The committee heard views from veterans that current treatment options
are not sufficient to meet their health needs. Veterans reported that the difficulty
in obtaining a definitive diagnosis covering the complexity of their health
issues also makes it more difficult to access treatment.
4.91
Mr Kruizinga explained that the DVA process is one of exclusion or
elimination to reach a diagnosis, which in his case, after numerous tests, has
not been reached.[103]
4.92
The Defence Force Welfare Association also expressed concern about the
effect of an incorrect diagnosis:
The absence of effective diagnostic routines, referral
protocols and dedicated rehabilitation programs is leading to very poor health
care. Affected individuals are commonly wrongly diagnosed with posttraumatic
stress disorder (PTSD) or other mental health disorders and subsequently
subjected to treatments which fail to improve their condition and may
inadvertently make it worse. The patient's neurological and psychological
difficulties arise not from a functional brain problem as current treatment
follows but from a structural change problem, drug mediated, that will require
a different treatment approach. Here in lies the reason for these individual
patient's failure to thrive. And for their on-going treatment.[104]
4.93
Associate Professor Quinn noted she has received reports from veterans
that address a 'common theme':
That certainly seems to be the common theme that runs through
the experience of the people that I talk to. They have ease of access to
psychiatry and they have ease of access to counselling, but if they ask for
something that sits outside any of those particular domains then all of a
sudden [their] SOP and their claim doesn't fit, and accessing that treatment
becomes almost impossible.[105]
Treatment for neurocognitive issues
4.94
As outlined in Chapter 2, the AQVFA has argued that mefloquine has
caused 'lasting or permanent brain damage, with chronic symptoms typically
misdiagnosed as PTSD or other psychiatric disorders'.[106]
4.95
Dr Nevin indicated that in his view that treatment 'is a little
premature to discuss'.[107]
However, veterans who provided evidence to the inquiry supported the view that
additional treatments needed to be available that address potential brain injury
and other neurocognitive issues.[108]
4.96
Associate Professor Quinn explained that treatments for brain injuries acquired
from taking antimalarials are not currently available:
I think the treatments that are lacking at the moment are
those that are applied to an actual brain injury as opposed to those that are
applied to a psychiatric condition. In the vast majority of cases of people who
have suffered long-term side effects from these drugs, what we see is the
profile of, essentially, a brain injury.[109]
4.97
Furthermore, Associate Professor Quinn explained that in her view, should
someone be incorrectly diagnosed with PTSD, they will be unresponsive to that
treatment:
What we see is that people who are treated for post-traumatic
stress disorder without having that as an absolute formal diagnosis that is 100
per cent correct—when that post-traumatic stress disorder is present as an
accumulation of symptoms caused by that underlying brain disorder, they're
actually non-responsive to the treatments for PTSD, and that's extremely common
in this group.[110]
How can the concerns raised by veterans be addressed?
4.98
While acknowledging the actions already undertaken by Defence and DVA to
date, the challenges and barriers reported by veterans demonstrate that these
actions are not meeting the needs of all veterans. The committee heard a number
of suggestions from veterans about the assistance and support they would like. Noting
the challenges of coming to an agreed position on the cause/s of their symptoms
between the veterans and their advocates and the medical community, the
committee discussed how best to address their health concerns.
Improving connections with the veteran
community
4.99
The committee heard various suggestions for how to improve the
connections between veterans and service providers, to ensure that veterans are
accessing the support to which they are entitled. It appeared that while
submitters agreed on this general point, views varied on how this could be
achieved. While many in the veteran community were calling for a proactive
outreach program, other evidence to the inquiry highlighted concerns with that
approach.
Ethical and practical concerns regarding proactive outreach
4.100
The committee was told that this kind of 'active outreach program' could
cause additional and unnecessary suffering to veterans and 'could also
undermine measures being applied more broadly to address the mental health of
veterans'.[111]
Associate Professor Harin Karunajeewa cautioned that it is:
...hard to see how such a program could be implemented without
implicitly suggesting to recipients of the outreach that their symptoms are
indeed related to previous drug exposure. This approach is therefore highly
susceptible to an important and very well characterised phenomenon known as
'recall bias'. It effectively becomes a 'self-fulfilling prophecy' and one
which I believe would contribute significantly to anxiety and other
psychological morbidity in these veterans.[112]
4.101
Defence has on a number of occasions indicated it does not support
undertaking a proactive outreach program as it is concerned that this approach
could potentially cause veterans undue harm. VADM David Johnston AO, Vice Chief
of the Defence Force explained:
Defence has considered whether individual follow-up of all
those who were involved in the antimalarial studies in the late nineties and
early 2000s is warranted. The vast majority of individuals who have taken these
medications are unlikely to have ongoing health problems. Our view has been
that contacting this majority might cause more harm than good. It may cause
unnecessary worry to individuals who have no reason to be concerned. The
significant profile of this issue now and the confusion that may now exist
amongst study participants mean that we need to keep this approach under
review.[113]
4.102
Defence suggested that there may be benefit in future outreach
activities being:
...focused more broadly on encouraging all veterans with any
health concerns to seek help, rather than specifically focussing on this group.
It remains pivotal that veterans and their families understand the services
available to them regardless of their diagnosis, many of which can be accessed
through DVA or through their GP, who are best placed to investigate, manage and
if necessary refer patients for specialist advice.[114]
New consultation program
4.103
An important issue is enhancing trust with this group of veterans as the
committee heard some have lost trust in the system, such as Ms Anne-Maree
Baker, who told the committee 'I have a real distrust in the government, the
military and any institutions because of my experiences since 2001 when my
health started to decline'.[115]
Mr Stuart McCarthy similarly said 'I have zero trust and zero faith in any
democratic institution in this country, because the culture of those
institutions is denial, at best'.[116]
4.104
As outlined above, DVA will be holding a series of consultation forums.
The consultation forum mechanisms may present an opportunity to enhance trust by
facilitating greater collaboration and fostering connections between veterans,
families, advocates and service providers, particularly DVA.
Improving cooperation
4.105
Ms Cosson, Secretary of DVA, acknowledged that there has been differing
views on what should be regarded as 'outreach' and, as a result, DVA is
undertaking what they are referring to as 'consultation'.[117]
Ms Cosson observed that, among the attendees at the recent Adelaide consultation
forum, there was not a strong level of awareness about what services are
available generally to veterans:
Recently we had a consultation session in Adelaide and we
talked with our veteran community. Forty of our veterans and families
participated in that consultation. What seemed to be a gap in understanding is
that when we introduced non-liability health care in the budget last year we
extended that free treatment for any condition that's listed in the DSM-5.[118]
4.106
Following the 11 October 2018 public hearing, DVA provided more detail
about the Adelaide forum including a summary of areas discussed which included:
health experiences related to ADF service (including experience with
antimalarial medicines), a lack of awareness of what supports are available
through DVA or Defence and concerns about how to access the mental health
workforce eg. psychiatrists and psychologists in Adelaide and South Australia.[119]
4.107
A number of suggestions came out of the public forum held in Adelaide. DVA
advised that attendees were invited to provide feedback via a short survey and
that overall, attendees reported that the 'forum provided helpful information
and a good opportunity to openly discuss their concerns'. However:
...some felt that the discussion became too emotional and that
a smaller group might help facilitate a more focused and comfortable discussion
for attendees. Attendees also identified that additional information on
available supports and services, including non-liability health care
arrangements, would be helpful.[120]
4.108
Regarding the forum in Adelaide, Associate Professor Quinn noted the
need to build on the information provided:
The other thing that did seem to be a deficit in the way the
first one [session in Adelaide] was carried out was that there really wasn't
any provision of information about what the next step for those people needed
to be other than 'put in your claims'. So we always give effect to this
circular—whatever you want to do, put in your claims.[121]
4.109
Associate Professor Quinn also suggested that DVA could proactively
contact groups such as the AQVFA to inform them of upcoming consultation or
information-sharing activities. She noted that in relation to the DVA sessions
held in Adelaide:
...what was interesting was that we [the AQVFA] weren't
informed of any of them directly. We found about the dates of all of them
through ex-service organisation members who have been on the mailing lists for
them, which is odd because I have Liz Cossin's personal email address and Tracy
Smart's mobile number and either of them could have given me a call and told me
when they were.[122]
Ensuring GPs have access to
relevant information
4.110
One of the key messages from Defence has been for those concerned to
seek assistance from medical practitioners. GPs are therefore central to
ensuring veterans have access to a range of health services and ongoing
support. Dr Penny Burns, representing the Royal Australian College of General
Practitioners (RACGP) explained the organisation's role:
The role of the RACGP in this discussion is around ensuring
general practitioners are available to provide ongoing support to veterans
affected by mental health symptoms and/or physical symptoms, whatever the
cause. Their aim is to continue to update GPs so they can provide the best
evidence based treatment on an ongoing basis. The aim is to decrease the level
of dysfunction experienced with symptoms and get people back to more normal
lives. In practice, when people present with symptoms—mental health issues, for
example—it's sometimes not possible to definitely define a cause, but, in most
cases, we're still able to look at managing symptoms to improve the conditions.[123]
4.111
Furthermore, Dr Burns emphasised:
In summary: the RACGP is keen to ensure easy access by
veterans to GPs for any support needed—be it for mental health symptoms and/or
physical symptoms, or just general distress; whatever the cause—and to ensure
that GPs are educated to provide the best possible evidence based support,
diagnosis and treatment for veterans.[124]
4.112
Evidence to the inquiry has reported varying levels of awareness among
GPs of the mefloquine and tafenoquine antimalarial drugs and it was suggested
that more needs to be done to better educate GPs about the issues being
reported by veterans.[125]
4.113
Officials from DVA recognised the important role of GPs to provide
assistance to veterans as well as the role that DVA has to support and educate
GPs:
...What we are very aware of, as I've looked into this and I've
worked with my colleagues and I've worked across the last year, is that we need
to find ways to educate our GPs better so that, when veterans present with this
type of disorder, there is a very clear, signposted way for people to get to
these specialists—because it is a specialist area.[126]
4.114
Dr Burns said most GPs would have a reasonable understanding of
mefloquine due to the fact that mefloquine 'has been used for quite some time'.
She spoke about the resources that have been made available to increase awareness
about mefloquine:
My understanding of most of the GPs who I know is that they
would have a reasonable understanding of that. There have also been clinical
guidelines brought out by the Joint Health Command. Recently, I think that the
Gallipoli Medical Research Foundation and the Returned Services League of
Australia put out a comprehensive brief on some PTSD stuff. And there has also
been some stuff coming out recently about mefloquine as well. So there's a lot
of education that comes out continually to GPs around that.[127]
4.115
Dr Burns noted that as tafenoquine is new, GPs would not typically have
received information about that yet:
Tafenoquine, no. I hadn't actually heard of it before or seen
it before the invitation to this inquiry. So, if I'm an example of the average
GP, I would presume that they don't have much information around that.[128]
4.116
Mr Karl Herz, Biocelect, informed the committee about the information
they will be providing to GPs leading up to the official release of
tafenoquine. As well as the information that is already provided on the TGA
website, Biolcelect is finalising a 'Dear Doctor' letter which will provide
information about the medication with a focus on explaining the
contraindications.[129]
Ensuring information sharing
between health professionals and DVA
4.117
As noted earlier in the chapter, DVA has undertaken activities to
increase GPs' awareness of the use of antimalarials in the context of the
veterans' community. Dr Burns noted that the clinical guidelines for GPs
produced by DVA and Defence 'are fantastic' and the importance of ongoing
information sharing and promotion across GP groups:
I think that one of the things that need to happen is that it
needs to be promoted through all the GP groups continually, and workshops and
webinars are the ways that GPs are now accessing information. I think having
the GP groups involved—so the AMA [Australian Medical Association], the
college, ACRRM [Australia College of Rural and Remote Medicine], the various
groups, promoting it. I think webinars, workshops, guidelines particularly—GPs
love guidelines and workshops. At the moment, there's a big conference, the
annual GP conference, GP18. That's another way of getting information out to
GPs.[130]
4.118
Dr Burns suggested that the provision and promotion of this sort of
information was particularly relevant around major bases as well as in other
locations where there is high volume of 'travel back and forth between malarial
areas'.[131]
4.119
On notice, the RACGP explained that a RACGP representative attends the
DVA Health Providers Partnership Forum[132]
meetings three or four times a year to provide advice to DVA about developing
information resources for veterans. Attendance at these meetings also
facilitates information sharing back to the RACGP about DVA programs.
Furthermore, the RACGP 'helps to distribute DVA information and resources
through RACGP publications' and has endorsed a number of resources that provide
information and support for veterans.[133]
Additional research underway
4.120
Professor Sandy McFarlane AO, Director of the Centre for Traumatic
Stress Studies, stressed the need for research which is independent in order to
provide reassurance to veterans about the findings.[134]
The committee is aware that Defence and DVA have jointly commissioned the
University of Queensland to undertake a research study on 'Self-reported health
of ADF personnel after use of antimalarial drugs on deployment'[135]
using 'de-identified data extracts from the Bougainville, Timor-Leste, and
Solomon Islands deployment health studies'.[136]
4.121
In its submission, DVA explained the new research will:
...focus specifically on the health outcomes of deployed
veterans who took anti-malarial medications. It is anticipated that this
research will be completed in the second half of 2018.[137]
4.122
Defence added that this research will examine the following research
questions:
- Did deployed veterans who reported taking mefloquine have
different rates of mental and general health outcomes compared to veterans who
reported taking doxycycline or other antimalarials?
- Did deployed veterans who reported taking primaquine on
return to Australia have different rates of mental and general health outcomes
compared to veterans who did not?
- Did deployed veterans report a significant reaction to
specific medications received during their deployment or raise use of
antimalarial drugs as an area of concern in response to open ended questions?[138]
4.123
At the time of the hearing in October 2018, there was no further
information available about the ongoing research. It was confirmed that the
research will be finalised later in 2018 and that the report will be published.[139]
The need for a multi-disciplinary
approach
4.124
The health issues identified by veterans in this inquiry are complex
with several individuals submitting long lists of symptoms and documenting a
range of conditions. Some had been diagnosed with particular conditions by a
health professional while others were still undergoing various tests and
consults to determine a diagnosis.
4.125
It was noted that responding to such varied and complex health needs
requires a multi-disciplinary approach. One veteran described the range of
supports he needs as follows:
One of my recommendations moving forward is that sitting in
front of a psychiatrist and being prescribed medication is not going to help or
do anything for my brain injury. What I need is psychosocial support...I've got
to the point where I need to start re-learning how to do things. I've managed
to get access to a social worker and I'm basically learning how to schedule a
day and tasks—things like that—and that's the support that we need.[140]
4.126
The RACGP has defined 'multidisciplinary care' as occurring:
...when professionals from a range of disciplines with
different but complementary skills, knowledge and experience work together to
deliver comprehensive healthcare aimed at providing the best possible outcome
for the physical and psychosocial needs of a patient and their carers'.[141]
4.127
Health professionals may include community health professionals, general
practitioners, and medical specialists. This approach is often used to treat
and support people with conditions such as cancer, and systematic approaches to
team based care are also emerging in 'primary care clinical areas such as
diabetes, aged care, mental health and disability'.[142]
4.128
Associate Professor Quinn emphasised the importance of including a broad
support network when providing treatment:
Managing those [people with brain injuries] isn't just a
matter of giving somebody a script with an antipsychotic or a sedative drug and
expecting them to go away and get better. There is also a whole family support
network that needs to be drawn up around somebody with a long-term brain
injury. If we were looking at somebody who had been brain injured in a car
accident and was going to be anticipated to have long-term neurological and
cognitive deficits, there's no way that we would be suggesting that that person
was going to manage their environment, manage their work-life balance or manage
their employment prospects without having a network of support around them and
their family. This is the thing that is missing when we have a situation with a
system that doesn't recognise this as a brain injury.[143]
4.129
Dr Stephanie Hodson CSC, National Manager, VVCS, DVA, acknowledged that
it can be challenging to confirm a diagnosis when individuals present with a
range of complex symptoms. The symptoms reported by veterans are wide ranging:
concerns about the 'neurocognitive element', anxiety, PTSD as well as other
'somatic symptoms' including digestive issues and skins problems. She
acknowledged that the complexity of these issues requires a holistic response:
All of this means that we've got to get to person-centred
care. We've got to have a way that we assess comprehensively the individual for
all those domains and then assist them to get to pathways. Just saying, 'Go to
your local GP,' doesn't necessarily mean that you're going to get the sort of
wraparound assessment you need. We need to help GPs actually identify the more
complex individuals who we need to put into a signposted pathway where we can
link them to the right professionals.[144]
4.130
Dr Hodson spoke further about the recognition by DVA that some
individuals need tailored, wrap around assistance which needs to include
neurocognitive aspects:
Across this journey, we've reached back into the department.
We hadn't, when we first started, thought a lot about rehab. With the pathways
to care that [Mr Stuart McCarthy] talked about, we are now figuring out how
someone gets there from maybe turning up in a VVCS office. We do the right
assessment and say, 'We do think there are some problems here that are not down
the anxiety end of the spectrum, or PTSD; they're actually in the
neurocognitive end,' and we now need to get those people to rehab specialists,
to speech pathology, and we are working for the first time ever with rehab
occupational therapists. There's a whole specialty here.[145]
Neurocognitive Health Program
4.131
In addition to offering existing treatments and support through DVA's
non-liability pathway, DVA advised that they are developing a new Neurocognitive
Health Program to assist veterans who may indicate symptoms of a neurocognitive
disorder (NCD). This program has been developed following feedback from
veterans that they have been unable to access appropriate support to address some
of the concerns they have attributed to mefloquine use.
4.132
Dr Hodson advised that:
The DSM-5 [Diagnostic and Statistical Manual of Mental
Disorders] made quite a big step forward around the fact that we all do tend to
forget the brain and psychology. Mental health is all interconnected, and it
starts with the brain. There is an area in the whole diagnostic continuum which
is about neurocognitive disorders, which can be caused from a range of issues.
It can be exposures, it can be playing sport, it can be mild traumatic brain
injury and it can be long-term life alcohol use. All of these can result in
impacts that are about a loss in memory, speech, neurocognitive functioning.[146]
4.133
Dr Hodson explained that a number of veterans from the 'mefloquine
cohort' had raised concerns that when they have tried to access DVA services to
discuss a possible brain injury, the response was to discuss PTSD.[147]
This experience reported by Dr Hodson is consistent with the evidence to the
committee's inquiry.
4.134
Dr Hodson explained that DVA had reflected on those representations and
acknowledged that the response to veterans' concerns may need to change:
We acknowledged, about a year ago, that we were not well
equipped to be able to do those assessments. It's actually a very specialised
area within the community. Over the last 12 months, we've been working really
hard to look at whether this is an area we can measure. The good news is that
we've we talked to Westmead Hospital and we've talked to people like Professor
Richard Bryant and Dr Ian Baguley, who do specialist work in this area, and
they've said that the science has really moved forward. A lot of it has come out
of the US to do with mild traumatic brain injuries. In fact, we've now got much
better neurocognitive screening that we can do. Importantly, there is
remediation we can do to bring about better outcomes.
What we're trying to do at the moment is develop a pathway so
that, if you come in, we can baseline where your functioning is. For anyone who
has served in the military, that's super important. If you've had a 20-year
career, you may have been around exploding ordnance, you may have played a lot
of rugby, you have potentially had toxic exposures, you may have drunk a bit of
alcohol—there are a whole range of reasons why your cognitive functioning would
be putting you at risk for early onset Alzheimer's down the track. We want to
be able to assess functioning baseline for anyone who is worried about
functioning. Where we find there is a problem, we have to have pathways to
care.[148]
4.135
It is envisaged that the program will be accessible to veterans assessed
as requiring treatment from anywhere in Australia. The assessment of current
functioning and provision of treatment will not be linked to any possible
cause.[149]
4.136
Dr Hodson further reported to the committee advice she has received from
a neuroscientist:
...it doesn't really matter whether the inflammation in the
brain was caused by PTSD or it came from a toxic exposure; at the end of the
day we've got to work with the inflammation of the brain.'[150]
4.137
This program is being developed 'initially through a Discovery Phase of
consultation and co-design to establish what the service would need to
provide'.[151]
In his submission, Professor McFarlane, noted that he has been asked by DVA to
advise on the development of the Neurocognitive Health Program. Mr Stuart
McCarthy also advised the committee that the AQVFA was invited to 'co-design
this program with them, in consultation with ABI rehabilitation specialists
already experienced in providing health care to affected veterans...'.[152]
4.138
Associate Professor Quinn also discussed the development of the Neurocognitive
Heath Program and in particular focused on the benefits of the co-design model
being used for its development as an example of different groups working
together in a cooperative manner:
I think we're beginning to work on that with the
neurocognitive health program that's being extended through VVCS, now Open
Arms, with DVA presumably sitting in the background of that. So that program
encompasses us, as QVFA, and senior leaders from Open Arms/VVCS. In that
process, we have engaged a number of healthcare experts who sit outside the normal
VVCS psychological counselling banner. Those include people who are specialist
in brain rehabilitation, people who are specialist in trauma psychiatry, people
who are specialist in providing family support, particularly around
rehabilitation. That's the kind of team that you start to need to build
together. It doesn't exist currently under the DVA/VVCS banner. So these are
specialists and agencies that are not routinely employed by either of those
organisations. But they are the types of agencies, and we'll find out who those
people are, and that group will extend the more that we go through that
process.[153]
4.139
The committee notes that DVA has discussed the development of the
Neurocognitive Health Program at the recent consultation forums and will
continue to inform veterans about the program.
Navigation: Previous Page | Contents | Next Page