Chapter 3
Identification and disclosure of mental ill-health
Introduction
3.1
This chapter considers the mental health strategies for ADF members and
veterans; identification and disclosure policies in the ADF in relation to
mental ill-health; and recordkeeping for mental ill-health for ADF members.
ADF Mental Health Strategies
3.2
In 2002 the Department of Defence (Defence) developed its first Mental
Health Strategy (MHS), seeking to promote mental health and wellbeing as well
as raise awareness of suicide and the misuse of alcohol, tobacco, and other
drugs. In 2009, the Review of Mental Health Care in the ADF and Transition
through Discharge (commonly referred to as the Dunt Review)
was published. The Dunt Review praised the ADF finding that its MHS compared
favourably to mental health strategies from militaries in other countries:
The establishment of the MHS by the ADF in 2002 was
far-sighted. The Strategy compares favourably with mental health strategies in
other Australian workplaces. It also compares favourably with what exists in
military forces in other countries. Some of these military forces have mental
health policies and programs in place, particularly in relation to PTSD. Others
have individual mental health programs in place however they do not have the
suite of programs at a whole of forces level that exists in the ADF. The
enthusiasm and commitment of ADF members in delivering these programs adds to
the ongoing achievement of the MHS. This has meant that programs are well
received by members.[1]
3.3
The Dunt Review noted that, despite its achievements, the ADF's Mental
Health Strategy needed further improvement 'for it to truly be a Strategy,
rather than a small number of small programs as at present'.[2]
The Dunt Review made 52 recommendations.[3]
ADF Mental Health Reform Program
3.4
Defence commenced the Mental Health Reform Program in 2010, based
substantially on the findings and recommendations of the Dunt Review.[4]
Defence invited a number of external mental health experts, clinicians, policy
advisors and researchers (including Professor Dunt) to form the Mental Health
Advisory Group, together with representatives of Joint Health Command (JHC),
single Services, Defence Community Organisation, Defence Families Association,
Department of Veterans' Affairs (DVA) and the Veterans and Veterans Families
Counselling Service (VVCS). The Group has met seven times.[5]
3.5
In 2011, Defence released its Mental Health and Wellbeing Strategy
(MHWS) and in 2012 released the supporting Mental Health and Wellbeing Action
Plan (MHWAP).[6]
The MHWAP lists six strategic objectives and the priority actions that need to
be taken to achieve them (see Table 1.1). The MHWAP also outlines the goals and
deliverables and describes 'what success will look like', for each of the
objectives.[7]
The Chief of the Defence Force (CDF), Air Chief Marshal Mark Binskin AC,
outlined Defence's achievements in the area of mental health since 2009:
...we have upskilled and increased our mental health workforce
as well as strengthened our resilience training and prevention strategies,
which now begin at recruitment. We have improved the screening programs used to
identify problems and we have also undertaken world-class mental health
research and surveillance. As a result, we know more now than at any point in
our history about the impact military service can have on the mental, physical
and social health of current and ex-serving personnel. We have a comprehensive
body of data about the causes and prevalence of mental health issues in the
Australian Defence Force population.[8]
3.6
Defence advised the committee that it has implemented all 52 of the
recommendations from the Dunt Review, investing $146 million in mental health
services and support (as at 30 March 2015). Defence has improved policy and
training for Defence health professionals; increased mental health research and
surveillance; and strengthened resilience training and prevention strategies.[9]
3.7
The Returned and Services League of Australia (RSL) commented on the
MHWAP, stating that its priority actions, whilst positive, are far from
achieved:
These hoped for outcomes have at best been only partially
obtained at this point in time and a great deal more work is yet to be
undertaken in order to achieve them. Too many individuals are suffering in
poorly managed circumstances at the present time without the necessary care and
supervision that's required from a number of appointed agencies.[10]
3.8
Consultations for the development of the ADF Mental Health and
Wellbeing Strategy 2016-2020 commenced in March 2015. The consultations are
being led by Joint Health Command and 'will involve engagement with a broad
range of stakeholders, both internal and external to Defence'.[11]
Table 3.1 – Strategic objectives
and priority actions of the ADF Mental Health and Wellbeing Plan 2012-15
|
Strategic
Objectives
|
Priority Actions
|
|
Promote and support mental fitness within the ADF
|
Addressing stigma and barriers to care
Strengthening the mental health screening continuum
Improving pathways to care
Developing e-mental health approaches
Developing a comprehensive peer support network
|
|
Identification and response to mental health risks of
military service
|
|
Delivery of comprehensive, coordinated, customised mental
health care
|
Improving pathways to care
Enhancing service delivery
Upskilling service providers
|
|
Continuously improve the quality of mental health care
|
|
Building an evidence base about military mental health and
wellbeing
|
|
Strengthening strategic partnerships and strategic
development
|
Strengthening the mental health screening continuum
Enhancing service delivery
|
Department of Defence, ADF
Mental Health & Wellbeing Plan 2012-15, p. 11.
Requirement for ADF members to be 'medically fit'
3.9
Defence has an obligation to ensure that ADF member's duties do not
detrimentally affect their health, that ADF members can undertake their duties
without compromising the safety of themselves or others, and that the ADF as a
whole maintains its operational capability. As outlined in the 2013 Review
of Health Information Practices in Defence, Defence must balance the health
of the individual ADF members with the effect that an individual's health issue
may create within an operational situation:
The requirement that a member be fit for the performance of
their duties is of paramount concern to the ADF. A member's employability and
deployability goes to the very reason for being of the ADF; its operational
capability. Members must be fit to undertake their duties without compromising
the safety of themselves or others. Defence has an obligation to ensure that
the undertaking of their duties does not have detrimental effects on the
member's health. Accordingly the seeking of health treatment by a member, the
provision of health treatment to the member by the Commonwealth, and, the
requirement by the ADF that a member undergo a health examination or treatment,
renders the provision of such a service as being outside the normally
understood relationship of health practitioner and patient. The relationship
becomes a 'three cornered' relationship with the ADF having a clear interest
not only in the effect of a member's current health statement vis-à-vis the
individual but also the greater effect that any health issue may create within
an operational situation.[12]
3.10
The Defence Act 1903 provides for regulations to be made in
relation to medical treatment of ADF members and cadets. It a condition of an
ADF member's service that they be physically and mentally capable of performing
the duties required of them and, if determined to be medically unfit (including
unfitness because of incapacity due to mental ill-health), a member's service
may be terminated under the provisions of the Defence (Personnel)
Regulations 2002.[13]
3.11
ADF members may be ordered to submit to medical examination. Part 6 of
the Australian Military Regulations 1927 provides for compulsory medical
examination of an Army member where directed by a superior officer to so
attend, including the requirement that the member provide the person conducting
the examination with all information and do anything required by the examiner
for the purpose of such an examination.[14]
Part 4 of the Air Force Regulations 1927 also provides that an Air Force
member may be examined in a way approved by the Chief of Air Force to determine
a member's level of medical fitness.[15]
The Navy operates similarly, however without such a legislative provision.[16]
Screening and early identification of mental ill-health
3.12
The Chief of the Defence Force stated that 'we are looking for early
recognition of a mental health injury and then looking to get early
rehabilitation to be able to get people back to work'.[17]
Defence advised the committee that it has implemented a comprehensive Mental
Health Screening Program to identify and provide assistance to individuals who
have been exposed to potentially traumatic events through activities such as
deployments, Border Protection operations, humanitarian and disaster relief
missions or training accidents.[18]
Referral pathways
3.13
Aspen Medical found that the most common referral pathway for ADF
members seeing a mental health professional was self-referral (29 per cent),
closely followed by referral by a Medical Officer (25 per cent) (See Figure
3.1). Aspen Medical noted that this suggests that ADF mental health policy
regarding the shared responsibility between commanders, individuals, and
clinicians for the identification and early treatment of mental ill-health is
working:
This success is evident in the high self-referral rate. It is
possible that another person such as a commander, padre, family member or
friend encouraged a patient to self-refer. However, the high rate of
self-referral indicates that many individuals are willing to seek treatment. It
also suggests that the stigmatism, once attached to [ADF members] mental
health, is changing at the individual level.[19]
Figure 3.1 – Referral Pathway for
Mental Health
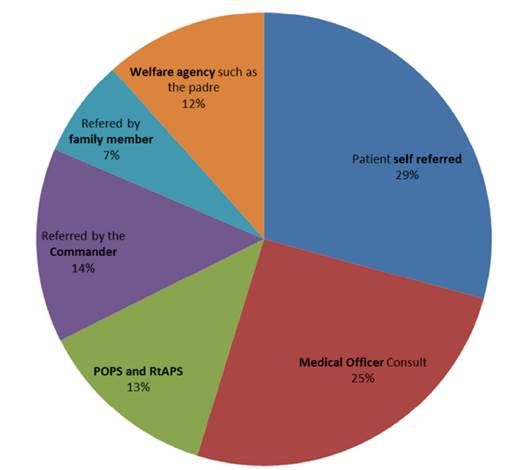
Aspen Medical, Submission
38, p. 15.
3.14
Some submissions questioned the effectiveness of screening in the early
identification of mental ill-health.[20]
Walking Wounded acknowledged that ADF mental health evaluation screening has
'improved markedly over recent years', but noted that it can be circumvented by
ADF members who do not wish to be identified as struggling with mental
ill-health:
The concept of post-operational psychological screening
(POPS) is good but can often be "gamed" by soldiers who are keen to
go on leave, etc, rather than be delayed by admitting to stress disorders.
While not widespread, there are many who feel that once they go on leave, they
will return to normal. Sadly, we know this isn't always the case.[21]
3.15
However, Dr Kieran Tranter informed the committee of a recent study,
using participants from the MHPWS, which considered the diagnostic accuracy of the
screening tests used by the ADF—the Kessler Psychological Distress Scale (K10),
Alcohol Use Disorders Identification Test (AUDIT) and the Post-traumatic
Checklist (PCL)—in a population-based military cohort. [22]
The study found that 'all three scales showed that good to excellent levels of
overall diagnostic validity' and 'could sensitively detect disorder whilst
maintaining good specificity'.[23]
3.16
Aspen Medical noted that it has found that screening activities are
'useful at identifying early some [members] who need help'. Aspen Medical
commented that the number of referrals to medical health professionals from
Post Operational Psychological Screening and Return to Australia Psychological
Screening indicates that screening is effective at early identification of
deployed member's mental ill-health and that 'this suggests that the policy and
conduct of these mandatory screens are achieving the effect that they were
designed to achieve'.[24]
3.17
Currently, there are a number of time points or key events that trigger
mental health screening within the ADF, with approximately 8,000 members being
screened every year. The majority of mental health screening is connected to
deployment and after critical incidents. ADF member's participation in
psychological screening, both on deployment and after returning from deployment,
is mandated by each operation's Operational Health Support Plan (OHSP). Routine
physical health checks, which occur every three to five years, also include an
alcohol use screen.[25]
3.18
Defence advised that mental health support and screening may also be
tailored to meet the requirements of a particular operation, giving the example
of the program for Operation RESOLUTE, which aims to provide psychoeducation,
surveillance and early identification and referral of members who require
follow-up mental health support.[26]
Types of screens
Return to Australia Psychological
Screening (RtAPS)
3.19
Return to Australia Psychological Screening (RtAPS) is provided to all
deployed ADF members nearing the end of their deployment. The aims of the RtAPS
are to document traumatic exposure; document and manage current psychological
status; provide advice and education to facilitate a smooth post-deployment
transition; and provide information to Command on the psychological health of
the deployed force. Further, in addition to identifying individuals at risk and
arranging referral for more detailed assessment, the data gained from the RtAPS
is used by the senior psychologist to brief the deployed element commander and
to enable trend analysis.[27]
The RtAPS comprises:
-
group psycho-education brief on:
-
the RtAPS and its aims and process (including confidentiality
issues and data use);
-
readjustment to family life (including reactions of partner,
children, and friends);
-
readjustment to work (including relationships with peers and
career decisions); and
-
health issues (including post-deployment fitness, and tobacco and
alcohol use).
-
a questionnaire, comprising the:
-
Deployment Experiences Questionnaire (including data on
operational temp and unit climate);
-
Kessler Psychological Distress Scale (K10);
-
Traumatic Stress Exposure Scale – Revised (TSES–R);
-
Major Stressors Inventory – Revised (MSI–R); and the
-
Posttraumatic Checklist (PCL).
-
one-on-one semi-structured screening interview, which covers the
following (as a minimum):
-
introduction;
-
deployment experiences;
-
potentially traumatic events;
-
coping strategies;
-
current symptoms;
-
homecoming and adjustment issues;
-
screening questionnaire summary; and
-
psychoeducation.[28]
Post-Operational Psychological
Screening (POPS)
3.20
Post Operational Psychological Screening (POPS) is mandatory for all ADF
members who were eligible to receive RtAPS (regardless of whether they did or
not) and is usually conducted within three to six months of a member's return
to Australia from an overseas deployment. The POPS process aims to identify
individuals who have not reintegrated into occupational, familial, or social
functioning and/or are demonstrating signs of adverse post-trauma responses. The
POPS questionnaires and write-up are placed on the ADF member's psychology file
and Unit Medical Record. The POPS process comprises:
-
a questionnaire, comprising the:
-
Kessler Psychological Distress Scale (K10);
-
Posttraumatic Checklist (PCL);
-
Alcohol Use Disorders Identification Test (AUDIT); and
-
additional Command and research questionnaires as approved by the
senior psychology asset for the services.
-
a one-on-one semi-structured psychological screening interview
that includes:
-
introduction;
-
review of the member's deployment experience;
-
homecoming;
-
reintegration;
-
current symptoms; and
-
psychoeducation.[29]
Special Psychological Screen (SPS)
3.21
A Special Psychological Screen (SPS) may be provided to individuals and
groups 'whose operational role routinely exposes them to intense operational
stressors, critical incidents, and/or potentially traumatic events while on
deployment'. The aim of the SPS is to aid the monitoring of the mental health
status of such individuals and groups. The SPS may be administered regularly
(every two to three months) and comprises:
-
a psycho-educational briefing;
-
a questionnaire comprising the:
-
Kessler Psychological Distress Scale (K10); and the
-
Acute Stress Disorder Scale (ASDS); and
-
a one-on-one psychological screening interview.[30]
3.22
The need for SPS is negotiated between commanders and mental health
professionals, and the completion of SPS does not negate the necessity for
RtAPS or POPS. Furthermore, the SPS can only be conducted by a mental health
professional.[31]
Critical Incident Mental Health
Support (CIMHS)
3.23
Critical Incident Mental Health Support (CIMHS) is initiated when a
'critical incident' has occurred, such as deployed members being exposed to
potentially traumatic events.[32]
The activation and timing of the CIMHS is determined by the Commanding Officer
in consultation with the CIMHS coordinator (the most senior CIMHS-trained
mental health professional available). The CIMHS process comprises a number of
activities across three stages:
-
provision of social support, and psychological first aid (PFA) if
necessary;
-
provision of psychoeducation and administration of psychological
screens (Acute Distress Disorder Scale and Mental Status Examination) to
facilitate the identification of individuals at risk of psychological injury
and initiation of referral for further assessment and treatment;
-
follow-up (Kessler Psychological Distress Scale (K10),
Posttraumatic Checklist (PCL) and Alcohol Use Disorders Identification Test (AUDIT).[33]
3.24
The timing of the follow-ups generally take place between three and six
months after the initial screen. According to the CIMHS database, a total of
354 individuals received a CIMHS initial screen between March 2012 and March
2014, with the majority of those 354 individuals also having completed a
follow-up screen.[34]
Informal screening
3.25
The Australian Defence Force Mental Health Screening Continuum Framework
Repot (MHSCF Report), conducted by the Australian Centre for Posttraumatic
Mental Health in 2014, highlighted the importance of informal screening for
mental ill-health and noted that formal screening is not intended to replace
informal processes, but rather, to complement them:
These informal processes may include families, friends, and
peers helping the member identify that he or she has a problem. This type of
informal screening is of great relevance in organisations such as the ADF that
place a high emphasis on "looking after your mates". A commander,
manager, or representative can also order a member to undergo psychological
assessment or gain psychological support through administrative referral.
Additionally, a Medical Officer (MO) can refer a member for psychological
support or assessment through medical referral. Of course, members may also
self-identify that they are experiencing mental health difficulties and request
assistance. These informational processes of identifying members who are
struggling with psychological adjustment issues are of primary importance in
early detection and access to care.[35]
3.26
Aspen Medical emphasised the importance of maintaining multiple ways to
identify and bring ADF members to treatment, noting that 'the multi-faceted
strategy taken by the ADF appears to be working'. It noted that in the ADF 'if
one method does not identify a case an alternative method is highly likely to'.[36]
Family involvement in
identification and screening
3.27
The importance of involving the ADF member's family in the
identification and treatment of mental ill-health was raised by a number of submissions.[37]
Australian Families of the Military Research and Support Foundation (AFOM)
asserted that families of ADF members are often the first to become aware of
signs of mental ill-health and called for family to be involved in
post-deployment screening processes.[38]
3.28
Aspen Medical noted that its practitioners strongly supported greater
involvement of a supportive family member in the treatment of mental health
conditions for ADF members.[39]
Furthermore, it found that seven per cent of referrals for ADF members to
mental health professionals were from a member's family, commenting that 'the
involvement of family also suggests that the ADF and JHC messaging to members'
partners, spouses and the broader community are having an effect'.[40]
3.29
The Australian Association of Social Workers highlighted the importance
of family involvement and assessment of family dynamics in the identification
and assessment of mental ill-health, noting that 'without a clear understanding
of family dynamics, including stresses and strengths, mental health assessments
will miss important information relevant for treatment and counselling
outcomes':
An early family assessment is not only crucial in
understanding the impact of a psychological diagnosis on the service personnel
and their family, but also means that important supports can be mobilised
early. It also alerts the clinician of areas in which clinical treatment might
be undermined by family dynamics. Often treatment is disrupted by events in the
external environment. Social work assessments that include a family assessment
and an assessment of other psychosocial factors are highly valued in mental
health teams.[41]
3.30
In 2011, the Family Sensitive Post Operational Psychology Screens
(FSPOPS) were trialled with Mentoring Taskforce-2 (MTF-2) in Darwin and with
MTF-3 in Townsville in 2012. The FSPOPS project involved training Defence
psychology staff in family sensitive practices that can be applied to the POPS
process. ADF members undertaking their POPS in Darwin and Townsville were invited
to bring an adult family member to their POPS to 'provide an opportunity to
discuss issues and challenges that may arise post-deployment'. This opportunity
was promoted by Regional Mental Health Teams and Command elements.[42]
3.31
Defence informed the committee that only a very small number of the
hundreds of ADF members deployed with MTF-2 and MTF-3 brought family members to
their POPS during the trial period. The majority of ADF members who did not
bring a family member to their POPS indicated that they 'felt no issues existed
that warranted discussion with a family member' or 'simply did not want to
bring a family member'. However, those family members who did participate
indicated that the experience was 'very good' and that they would participate again
if offered.[43]
3.32
Defence advised that the outcome of the trial 'suggests that this
initiative was not one that appealed to the wider ADF audience' and that, as
such, the trial was not extended or developed into business as usual. However,
Defence assured the committee that it remains committed to a family sensitive
approach to screening and mental health and rehabilitation service delivery:
The trial has not been extended or developed into business as
usual, but the concept of ensuring that family related matters and family
sensitive questions are raised during Post Operational Psychology Screens by
psychology staff has been adopted. This has resulted in a more family focussed
approach to operational mental health screening of ADF members.
Defence recognises the importance of engagement with and
support to families of members who are ill or injured. Defence is focusing on
developing services and processes that support a family sensitive approach to
mental health and rehabilitation service delivery, to promote positive outcomes
for members and families. These processes include inviting family attendance at
health assessments (where appropriate and with member consent), inviting
attendance at psychosocial workshops and information sessions, and referral to
available programs and services as appropriate. Resources available to family
members are also reinforced through unit family days and direct communications
from support services such a Defence Community Organisation or Veterans and
Veterans Families Counselling Service.[44]
Privacy
3.33
Some submissions noted that, linked to the stigma associated with mental
ill-health, many ADF members were not comfortable disclosing mental health
issues due to concerns that their privacy would not be respected and they would
be subject to ridicule.[45]
The Australia Psychological Society noted that:
Members report that stigmatisation may occur during service
within the immediate base community and the larger organisation. This stigma
and issues with confidentiality reportedly create difficulties particularly at
the lower level of command where information about confidential disclosures [of
mental ill-health] reportedly is disclosed to others in the base community.[46]
3.34
Defence assured the committee that it is required to comply with the
provisions of the Privacy Act 1988 (Privacy Act) and the Australian
Privacy Principles. Health Directive 610 Privacy of health information of
Defence members and Defence candidates outlines the policy regarding
the collection, use, and disclosure of health information in Defence by health
professionals, commanders, managers, and members. A Health Information Privacy
Notice, which details how health information is collected, used, and disclosed,
is available to all ADF members on the Defence Intranet.[47]
3.35
ADF members must give consent for their personal health information to
be used or disclosed in all but exceptional circumstances (as defined by the Australian
Privacy Principles).[48] Exceptional circumstances include when use
or disclosure is necessary to lessen or prevent a serious threat to an ADF member's
life, health, or safety; or a serious threat to public health or public safety,
including in military workplaces and safety critical areas such as deployment.[49]
3.36
Defence informed the committee that health information is primarily
collected by Defence health practitioners 'in order to clinically manage and
treat a Defence member's health on an ongoing basis'. This health information
is shared between all treating health professionals in order to provide
coordinated health care services, particularly when ADF personnel are receiving
mental health care. Health information can also be shared with external health
care providers with the consent of the ADF member.[50]
3.37
Defence stated that Defence health professionals are obliged to keep
commanders and managers informed of the health status of ADF personnel to
enable them to manage the workplace and operational impact of an ADF member's
health condition. The health information provided is limited to information
'that enables a member's administrative management to be coordinated with their
health support and rehabilitation management plans', unless the ADF member
consents to more information being provided.[51]
Commanders' need to know and
members' right to privacy
3.38
Some submissions highlighted the conflict between commanders' need to
know about the mental health of their personnel and ADF members' right to privacy.[52]
The Inspector General of the Australia Defence Force (IGADF) noted that
compliance with Privacy Act requirements and the confidentiality obligations of
members of the medical profession can 'sometimes impede the reasonable sharing
of medical and psychological information concerning a member that may be
important for their better management by their chain of command or other
Defence agencies with responsibilities for members' welfare and safety'.[53]
3.39
The Alliance of Defence Service Organisations (ADSO) asserted that
commanders 'should surely have the right to know, and medical professionals the
right to inform [them]', regarding any medical (mental or physical) problems
that could compromise a mission or the safety of other ADF members. Further,
the ADSO called for the application of the Privacy Act, as it applies to ADF
members, to be reviewed:
The bargain struck between the ADF and the individual should
be that the ADF provides comprehensive health care free of charge because it
has to have a solid base of confidence that the individual meets the fitness
standards demanded by the mission. This should mean that the individual
surrenders that part of the right to privacy that is relevant to the mission,
as he does in other areas, such as military security. Indeed it could be argued
that physical and mental fitness is, at least in part, a security matter. ADSO
urges that this aspect of the application of the Privacy Act to members of the
ADF to be reviewed as a matter of urgency.[54]
3.40
The IGADF advised the committee that some ADF members will choose to
seek assistance from sources outside of the ADF for mental ill-health to
prevent the chain of command from accessing information about the member's
mental health. Such members fear putting their career, job categorisation, or
deployment opportunities at risk. The IGADF described this as a 'catch-22
situation for Defence', for any attempts to relax patient confidentiality
requirements to better identify and address mental ill-health might further discourage
members from seeking assistance/treatment for mental ill-health within the ADF:
...the reluctance of some members who are aware they may have a
medical or mental health problem to advise their chain of command or seek help
from Service health authorities for fear of putting their career, job
categorisation, or deployment opportunities in jeopardy. This can sometimes
create a catch-22 situation for Defence where members may be minded to seek
assistance from private sources in order to preserve confidentiality of their
condition. The catch-22 arises where any relaxing of patient confidentiality
requirements within Defence might potentially have the unintended effect of
encouraging members to seek help outside the Service system.[55]
3.41
The RSL also commented on ADF members' reluctance to disclosing mental
health concerns, noting that some members choose not to disclose symptoms to
avoid medical downgrading, which may interfere with their deployment or result
in discharge. The RSL stated that 'members are well aware of the financial
incentives associated with deployment and the need to be physically fit and
mentally fit to deploy'.[56]
The RSL, pointing to an opinion expressed in an interview with Dr Andrew Khoo,
asserted that:
...encouraging Defence members to seek early treatment for
mental ill-health will not be successful until Defence allows members to be
treated and continue in their career with Defence. Until then, serving members
will continue to believe disclosure of mental ill-health will threaten their
Defence career.[57]
3.42
Defence acknowledged that there are times when 'despite all the best
efforts on rehabilitation...people will end up inevitably being discharged',[58]
but that 'of the 869 individuals with a mental illness who completed a rehabilitation
program, a total of 420 or 52 per cent are recorded as having a successful
return to work at the end of their rehabilitation program'.[59]
3.43
The adequacy of mental health services is discussed in greater detail in
Chapter 4 of this report. Stigma surrounding mental health and other barriers
to disclosure is discussed in greater detail in Chapter 5.
Family access to members and
veterans mental health records
3.44
Slater & Gordon Lawyers called for a review of the Privacy Act,
asserting that details of mental health records should be released to families
if the ADF member or veteran presents symptoms of mental illness that pose an
immediate risk to personal safety, such as self-harm and suicide attempts.
In such situations, the ADF must have the authority to
release certain details of a serviceman or woman's mental health record to
their families in order for them to assist in providing support...the Committee
must do everything in its power to ensure that families do not have to endure
the heartbreak of losing a loved one from a potentially treatable mental
illness.[60]
3.45
Slater & Gordon pointed to the family of 27 year-old Navy Sailor
Stuart Addison, who took his own life in 2002. His family have been campaigning
for the next of kin to be contacted immediately by a member's commanding
officer in circumstances where suicide attempts or self-harm is evident.[61]
3.46
One submitter called for families to be notified of suicide attempts.
The submitter told the committee of their experiences strugglingly with mental
ill-health and suicide, stating that their first attempted suicide took place
while still a serving member. The submitter noted that 'suicide prevention
takes inside information' and called for the introduction of a 'Family in
Crisis Action Plan' to be triggered in the case of a suicide attempt:
...when a Veteran attempts Suicide, that contact is immediately
made with the Veteran Family. Implementation of an Action Plan should include
ESO Contact, Family Social Worker Contact to be able to assist any needs of the
family during the Crisis. Also emergency Crisis care for children should be
initialised and paid for by DVA whilst the Veteran is hospitalised and in
treatment so that the partner or designated carer or eldest child can
participate in the support and information process with the Veteran. "It
must not be a journey taken alone by the Veteran."[62]
3.47
Defence acknowledged these concerns but asserted that its focus is on ensuring
ADF members are 'afforded appropriate privacy protections' while encouraging
them to involve families and support networks in their mental health safety
plan, treatment and recovery:
Defence recognises that there have been concerns expressed by
family members about what information can be disclosed to them and how
disclosing certain health information could have resulted in better mental
health outcomes, or in extreme situations prevented a death by suicide.
Defence's focus is on ensuring that ADF personnel are afforded appropriate
privacy protections while encouraging the member to involve their families and
support networks in their mental health safety plan, treatment and recovery by
sharing their health information should they wish to do so.[63]
Recordkeeping for ADF members
3.48
Defence informed the committee that 'health-related record keeping is
managed in accordance with the Defence Records Management Policy and the
relevant legislation'. Defence also advised that it is currently reviewing its
health records management policy to provide a 'single policy for all ADF
personnel that receive health services from Defence'.[64]
However, the management of ADF mental health records has been criticised for a
number of decades and have been the subject of a number of inquiries and
audits.[65]
3.49
The committee received a number of submissions commenting on the
difficulties with accessing health records and the complications that can arise
when a veteran is making a claim if health records are incomplete or
inaccurate.[66]
Furthermore, comprehensive health records of veterans can be even more
challenging, as noted by Mr Robert Shortridge: 'maintaining records of those
ex-service personnel once they have left the ADF will be very difficult as
there is no compulsion for them to identify themselves as ex-service personnel
or veterans'.[67]
3.50
Walking Wounded described ADF recordkeeping as a 'weak area', noting
that, despite good recordkeeping policies, 'human error, tiredness, inattention
and carelessness' lead to incidents being reported 'badly or not at all':
Anecdotally, all soldiers have stories of how a particular
incident was recorded badly or not at all, including events where injuries
occurred. This often leaves the record incomplete or disjointed, particularly
where operational imperatives take precedence. In addition, the retrieval of
records pertaining to a specific incident some years in the past is often
almost impossible, owing to personnel turnover and the reasons cited above.
When an ADF member is no longer an ADF member, the task gains a further degree
of difficulty.[68]
3.51
One submitter noted that a complete and accurate record of a member's
mental health is dependent on the member disclosing their mental ill-health,
something that many may be reluctant to do.[69]
Defence e-Health System
3.52
In 2009, Defence launched the Defence eHealth System (DeHS) (originally
called the Joint eHealth Data and Information System). The key features of the
DeHs include:
-
Primary Care System (PCS): an eHealth care system used to record
all clinical, dental, mental health, and allied health consultations,
treatments and findings;
-
DeHS Access: an online patient- accessible summary of each
patient's eHealth record; and
-
DeHS Reporting: a suite of reporting tools available to report on
individual or corporate information requirements.[70]
3.53
These three features are intended to provide a clinical management tool
'that enables safe and quality health care for the ADF member'. The DeHS
business case noted that the system would:
-
inform ADF Commanders of the readiness for operational
deployments of individuals and Force Elements;
-
contribute to the generation of health performance and work
health and safety metrics to support the management of resources as well as
planning and accountability; and
-
provide for effective health management after an ADF member's
discharge by facilitating the transfer or access of an ADF member's health
record by DVA as part of ongoing care and/or to inform compensation
determinations.[71]
3.54
Furthermore, the DeHS is intended to complement the civilian National
e-Health Strategy and link with the national Personally Controlled Electronic
Health Record:
The Joint eHealth Data and Information (JeHDI) Project [now
called DeHS] will facilitate the provision of one electronic health record for
ADG personnel, from recruitment to discharge, then through to management in
other agencies...[DeHS] is building the capability to interact with the National
Personal Controlled Electronic Health Record (PCEHR) for the interchange of
health information across private and public health systems. Members will be
able to consent to participation in the PCEHR system while in Defence or when
they discharge.[72]
3.55
Defence advised that the DeHS was implemented within all Joint Health
Command Garrison health centres on 11 December 2014 and that the DeHS project
to implement the system on-board ships is scheduled for implementation on the
"First of Fleet" by June 2016, with subsequent roll out to the
remainder of the fleet in accordance with the Fleet schedule.[73]
3.56
Defence informed the committee that it is expected that ADF members will
be able to access their e-Health record via the internet portal from the
second-half of 2015. ADF members will be able to view a summary of their health
record, view recent and scheduled appointments, and complete health
questionnaires in preparation for a mental health consultation. ADF members will
be able to access routine mental health questionnaires and screening tools
online, which, Defence advised, will notify mental health professionals if the
results of a questionnaire need to be responded to urgently.[74]
3.57
Defence explained that the data analysis and reporting functions of DeHS
will allow Defence to 'target reporting for specific mental health
presentations and disorders and that the DeHS system has minimised the use of
paper records, with the majority of ADF members receiving primary health care
treatment through a Garrison Health Organisation'. All mental health and
psychology records created prior to the implementation of DeHS will continue to
be available. In addition, as legacy systems are decommissioned, all pertinent
records will be transferred to Objective (the approved restricted Defence
electronics records management system).[75]
3.58
Aspen Medical reported that it received a number of positive comments in
its initial survey regarding the benefits of the new DeHS, with 39 per cent of
respondents agreeing that the DeHS has improved the availability of relevant
documents and only 18 per cent disagreeing or strongly disagreeing. Aspen
Medical noted that many positive comments also expressed a degree to
frustration with DeHS.[76]
Hospital admissions, external
referrals, and fatalities
3.59
Defence explained that the DeHS incorporates ADF members' external
mental health provider reports, ensuring that a member's health record reflects
a continuous view of their mental health care that can be monitored by Defence:
The Defence e-Health System allows for the timely monitoring
of external mental health provider reports by the local Mental Health and
Psychology Section, and these reports are reviewed at the regular
multidisciplinary Case Review meetings to ensure that treatment is meeting the
needs of the member, and that the member remains engaged with the external
provider. The external reports are then electronically appended to the member's
health record via Defence e-Health System in order to provide a continuous view
of the member's mental health care.[77]
3.60
If an ADF member requires admission to an external treatment facility as
an inpatient, either as an emergency or planned admission, the referral is
noted in the member's e-Health record and a Notification of a Casualty
(NOTICAS) and a Medical Casualty (MEDICAS) are raised. The NOTICAS and MEDICAS
notifications allow command, health, and welfare agencies to ensure that the
member's occupational, health, and domestic needs are met and that the member's
family is supported during the admission. Once discharged, a discharge summary
report is provided to the treating garrison health facility and uploaded into
DeHS. Defence advised that the admission of an ADF member to an external
treatment facility for mental health in-patient treatment is regularly followed
up by the local Mental Health and Psychology Section.[78]
3.61
Defence advised that, following the death of a serving ADF member, the
e-Health record is moved from the DeHS to Objective, the approved restricted
Defence electronic record management system for archival purposes. The archived
record can be accessed by Defence health care professionals and member's
families can request access 'using normal Defence record access request
processes'.[79]
Suspected or confirmed suicide
3.62
Defence informed the committee that the release of post mortem results
and coronial inquiry outcomes remains at the discretion of the coroner and are
not routinely provided to Defence unless pursued by the ADF Investigative
Service. Defence noted that post mortem updates can be made to an ADF member's
DeHS record upon receipt of a death certificate or coronial record but that
this is not mandated:
Clinicians do not currently update the record regarding
speculative diagnosis or causal finding. The finding of suicide has to be a
post mortem update and this is permitted to be added to the record by
authorised users. The content of these updates/entries are not mandated in any
way. If Defence does receive a death certificate or coronial record it will be
added to the record.[80]
3.63
Defence advised that Joint Health Command maintains a database, separate
to the DeHS, of suspected or confirmed deaths as a result of suicide since 1
January 2000. Suspected or confirmed deaths as a result of suicide are included
in the database on the advice of the ADF Investigative Service and/or the
findings of State/Territory Coroner Reports.[81]
Medical records during deployment
3.64
Aspen Medical reported that that it 'is rarely easy to find relevant
clinical information collected or recorded in-theatre' regarding mental
ill-health or potentially traumatic incidents:
Just over 75 per cent of respondents found that it is usually
not easy to find clinical information on incidents that occurred in theatre. In
many instances the trigger event for a mental health condition may not have an
immediate impact on the [member], so in effect there is no clinical record of
the event occurring.[82]
3.65
Aspen Medical noted that some clinicians suggested that Medical Officers
(MO) and Mental Health Professionals (MHP), when treating a member, should be
given access to the member's commander when the traumatic event occurred which
might have caused mental health problems. This would allow the MO and MHP to
understand the events without forcing the member to 'relive' them.[83]
3.66
A number of submissions highlighted the importance of accurate and
detailed records when lodging a claim with DVA.[84]
This is discussed in greater detail in Chapter 5 of this report.
Identification and screening of mental ill-health during transition
3.67
The ADF does not currently conduct post-transition screening. The
Defence Community Organisation emails a post-separation survey to all ADF
members who have been discharged for at least three months. The post-separation
survey asks questions regarding the separation experiences, the member's chosen
post-transition occupation, and their perceptions of support received around
transition.[85]
3.68
The MHSCF Report noted that screening at discharge was challenging due
to transitioning members' concerns that identification of mental health
problems might delay their discharge:
During the discussions about timing, the process at
transition was raised. Both senior leaders and health professionals noted that
screening at transition was challenging as members may be concerned that
identifying mental health problems may delay their discharge. There were some
suggestions that, if screening were to be included in the transition process,
it should occur around six months prior to transition in order to be able to address
any concerns without the risk of delaying the member's leave.[86]
3.69
Discharge and transition from the ADF to civilian life with be discussed
in greater detail in Chapter 6 of this report.
Veteran Mental Health Strategy
3.70
The Department of Veterans' Affairs (DVA) is responsible for the
development and implementation of programs to assist the veteran and defence
force communities. It provides administrative support to the Repatriation
Commission and the Military Rehabilitation and Compensation Commission. It is
responsible for advising the Commissions regarding policies and programs for
beneficiaries as well as for administering these policies and programs. Mr Shane
Carmody, the Chief Operating Officer for DVA, advised the committee that mental
health is a priority for DVA:
Mental health is a priority for DVA and any suicide is a
tragedy, so we must do all we can to prevent it. As the committee knows,
funding for mental health treatment is demand-driven and is not capped. We
spend around $182 million annually on veteran mental health services, but our
focus remains on early intervention. If people are worried about how they are
feeling or how they are coping we encourage them to seek help early. There are
services and there is support ready and waiting to help.[87]
3.71
The Veteran Mental Health Strategy 2013-2023 outlines the
strategic framework to support the mental health and wellbeing of veterans. The
strategy lists six strategic objectives to guide mental health policy and
programs:
-
ensure quality mental health care, which puts the client at the
centre, is evidence-based, efficient, equitable, and timely;
-
promote mental health and wellbeing, addressing the diverse needs
of clients and barriers to help-seeking such as stigma;
-
strengthen DVA workforce capacity, ensuring a strong
understanding of military and ex-military experience, and knowledge of best
practice mental health interventions;
-
enable a recovery culture, reducing the stigma surrounding mental
health in the veteran and ex-service community and encouraging help-seeking and
support recovery;
-
strengthen partnerships, leading to improved service systems,
enhanced communication and coordination, efficient use of resources, and
opportunities for continuous feedback and improvement; and
-
build the evidence base, building capacity within the mental
health provider community and informing policy and program development.[88]
3.72
DVA described the focus of its mental health policy as 'firmly on early
intervention':
The benefits of early intervention are clear, both for the
veteran and their family. Recent Government budget initiatives further
highlight the commitment to treating mental health conditions. Over recent
years, significant funding has been invested in new initiatives aimed at
improving the mental health of veterans, from improved access to treatment and
counselling, through to improvements in the Department's management of clients
with complex needs, including those with mental health conditions. Further, the
Government is very focussed on improvements to reduce the time taken to process
compensation claims, a key early initiative.[89]
3.73
Mr Carmody reiterated this, stating that 'DVA's major focus is on early
intervention. This is the critical step in identifying and meeting the mental
health needs of the veteran community'.[90]
Identification of mental ill-health in veterans
3.74
Unlike ADF members, veterans are not required to be screened for mental
ill-health and veterans cannot be 'ordered' to seek treatment or assistance
when they display symptoms of mental ill-health. However, veterans can access
the ADF Post-discharge GP Health Assessment, a 'comprehensive health
assessment from their General Practitioner (GP)'. The scheme provides GPs with
screening tools for alcohol use, substance use, post-traumatic stress disorder
(PTSD) and psychological distress 'to help GPs identify and diagnose the early
onset of physical and/or mental health problems'. The scheme is funded under
the health assessment items on the Medicare Benefits Schedule.[91]
3.75
Generally, DVA is made aware of a veteran's mental ill-health once a
veteran has lodged a claim. A number of submissions noted that this puts the
impetus for recognising and seeking treatment for mental ill-health on the
veteran.[92]
Walking Wounded commented that 'once a Defence member leaves the service, the
responsibility for overarching care falls foremost onto the individual and, if
he or she is lucky, close family members'.[93]
The Australian Psychological Society described this as a critical barrier to
identifying the scope of veterans' health needs:
Post discharge, veterans are unable to be identified by DVA
where they do not seek entitlements to pensions, compensation or treatment.
This creates critical barriers to identifying the scope of service-related
health and welfare issues and the demand for associated services. While DVA
advocates that there should be service pathways which operate under the 'no
wrong door policy' approach and maintains registration information about
veterans and current serving personnel who seek entitlements, in the absence of
such registration, there is little chance that ex-service personnel will seek
or receive the DVA funded treatment to which they are entitled.[94]
3.76
The Royal Australian Regiment Association (RARA) noted that 'many
veterans leave the ADF without lodging any claims for disability but they
develop problems later in life and who are, or consider themselves to be
healthy, may feel a little embarrassed about seeking help'. The RARA asserted
that 'DVA is the appropriate sponsor for embracing these people' and called for
a review of the processes for identifying and monitoring veterans mental
health:
There needs to be a major conversation and paradigm shift in
the mindset of the Government and Parliament, Defence Department that includes
DVA, veterans, and the broader community as to how we can best keep track of
all our veterans well after their service and not just those who have become
DVA clients.[95]
3.77
The RSL also noted that many veterans are reluctant to respond to early
symptoms of mental ill-health, stating that 'ignoring symptoms and not seeking
help can sometimes go on for eight to 10 years after discharge':
We are told by many veterans and their families that symptoms
are ignored for a variety of reasons, including pride, learned responses in
Defence to ignore emotions and keep going, the financial incentives associated
with deployment, a belief that they are not the problem, and a lack of
knowledge of the symptoms of mental ill-health.[96]
3.78
DVA acknowledged these concerns, noting that 'the challenge for DVA is
to encourage clients to seek help early if they are worried about how they are
coping or feeling, and not wait until the symptoms become overwhelming'.[97]
Mr Carmody advised the committee that DVA is working to raise awareness of its
services, assisting transitioning members, and encouraging the early lodgement
of claims:
To ensure that people know about our services and the support
that we can provide, the department secretary now writes to all 6,000 or so ADF
personnel who separate each year. This letter outlines what DVA can do for them
and that we are here to help them if and when required. Even so, around 25 per
cent of separating ADF personnel opt out of receiving information from DVA.
DVA's on-base advisory service has developed into a very important service,
providing advice and support as well as encouraging the early lodgement of
claims. DVA now has an on-base presence at over 44 bases around the country. In
2013-14, our on-base service responded to over 13½ thousand inquiries—an
increase of over 4½ thousand on the previous year.[98]
3.79
DVA asserted that it is using 'new and innovative ways' to reach out to
contemporary veterans and encourage them to take action early to address any
mental health concerns. DVA provides a single mental health online portal, known
as 'At Ease', which brings together all of its online products. These include:
self-help and supportive phone apps; videos of veterans talking about their
mental health recovery; and information about professional support and
treatment options.[99]
3.80
DVA advised that it also works in partnership with the ex-service
community to implement health and wellbeing programs, which focus on seeking
help when needed and healthy lifestyle behaviours such as healthy eating, social
connectedness and physical activities.[100]
The RSL stated that it is working together with DVA and other ex-service
organisations (ESOs) to reach out to veterans who are struggling with mental
ill-health:
The RSL, other Ex-Service Organisations (ESOs) and DVA are
working hard to 'pick up the pieces' and intervene as soon as anyone in
difficulty is brought to our attention. Informal networks of support, both
face-to-face and online are extensive. There is a collective goodwill and
concern for mates that characterises this sector (among both current and
ex-serving members) and together many veterans have saved the lives of others
in trouble.[101]
3.81
However, the RSL warned that 'relying on informal networks alone can be
fraught with potential problems'.[102]
Veterans identification system
3.82
The RARA and the Alliance of Defence Service Organisations called for
the introduction of a veteran identification number or identification card to
assist in the collection of data regarding the health and wellbeing of veterans
who are not DVA clients.[103]
The RARA noted that:
In recent times, the media has highlighted the incidence of
veterans being incarcerated and sadly self-harm and suicide. These three issues
raise the possibility that many of the homeless, veterans in the prison system
and self-harm are invariably in this state due to mental health issues. Too many
veterans are falling through "the cracks" because we don't know who
or where they are.[104]
3.83
The Veterans Care Association noted that the provision of a veteran
identification card would 'add dignity and honour the service of all veterans'.[105]
The ADSO asserted that the introduction of a veteran identification card would
allow support services such as medical, ambulance, police and government
agencies to better identify veterans:
One of the principle requirements of support is being able to
identify veterans. The need for a single identifier to follow and ADF through
service and into post ADF life is becoming more evident. It has the support of
the AMA [Australian Medical Association]. It should cover all serving and
former ADF members.
A National Veteran Identity Card could fulfil this need and
would allow support agencies (medical, ambulance, police, government agencies,
etc.) to identify and allocate veterans to the appropriate assistance needed.[106]
3.84
Mr Carmody advised the committee that DVA is working with Defence to
implement a single identification number but that there are a number of
complications including non-ADF DVA clients (such as war widows) and privacy
issues:
We are also trying to work with Defence on this single number
but, as I have said, we have 340,000 clients and a large number of our clients
do not have ADF service; they are war widows. So 60,000 to 70,000 people do not
have a Defence number. We also have the situation where, particularly, our
World War II and or Korean veterans had different prefixes on the numbers that
they were allocated when they were in service, by state. There were different
prefixes by gender. Our history of engagement with the numbering system is a
very long one, and there is a range of very different numbers. We are in the
process of working with Defence to try and resolve that in looking forward;
however, in terms of all of our current client base, we need a very complex
system of cross-referencing the various numbers that they might have been
given, including DVA numbers. It is not a straightforward matter of just giving
everyone a number, because as I said, a large number of our clients will not
have one to start with.[107]
3.85
The records required for DVA claims, and the systems under which these
records are stored and accessed, is discussed in Chapter 5 of this report.
Committee view
3.86
The committee acknowledges the challenge of ensuring that ADF members'
duties do not detrimentally affect their health; that ADF members can undertake
their duties without compromising the safety of themselves or others; and that
the ADF as a whole maintains it operational capability. The committee commends
the ADF for its mental health and wellbeing strategy and acknowledges the
significant achievements that it has made since the introduction of its first
Mental Health Strategy in 2002. Early identification and treatment of mental
ill-health is crucial for ADF members struggling with mental ill-health to
achieve the best possible outcomes as well as ensuring that the ADF maintains
operational capability.
Identification of mental ill-health
in the ADF
3.87
The committee is satisfied that the RtAPS, POPS, SPS, and CIMHS
screening processes, together with informal screening, are useful tools for the
early identification of mental ill-health among ADF members who have been
deployed. However, the committee is concerned that similar care is not taken to
identify mental ill-health among ADF members who have not been deployed. As
discussed in
chapter 2 of this report, the findings of the MHPW study indicated that there is
no significant link between deployment and an increased risk of developing
PTSD, anxiety, depression or substance abuse disorders. Yet, despite this, mental
health screening appears to focus primarily on identifying mental ill-health in
members who have been deployed.
3.88
The committee is encouraged by the referral pathways reported by Aspen
Medical and the high percentage of self referrals and referrals from medical
officers, which indicate that mental health policy regarding the shared
responsibility between commanders, individuals, and clinicians for the
identification and early treatment of mental ill-health is working. However,
the committee believes that regular formal and informal screening of ADF
members, regardless of their deployment status, will improve the early
identification and treatment of mental ill-health in the ADF.
3.89
The committee acknowledges that ADF members may be concerned about the potential
impact that the discovery of mental ill-health may have on their careers.
Nonetheless, the committee believes that the early identification and treatment
of mental ill-health is significantly less likely to negatively impact a
members' career, both within and beyond the ADF, than mental ill-health that is
left untreated. Furthermore, annual screening would provide a regular
opportunity for ADF members to pause and consider their mental health as well
as providing a forum to express concerns that they might have without the
member needing to initiate an appointment with their medical officer or
psychologist.
Recommendation 1
3.90
The committee recommends that Defence conduct annual screening for
mental ill-health for all ADF members.
Privacy and disclosure of mental
ill-health
3.91
The committee acknowledges ADF members' right to privacy and the stigma
and concerns regarding career prospects that might cause ADF members to conceal
mental ill-health from their commanders and colleagues. However, the committee
recognises that the ADF members' right to privacy must be carefully balanced
with commanders' responsibilities to ensure that ADF members' duties do not
detrimentally affect their health, that ADF members can undertake their duties
without compromising the safety of themselves or others, and that the ADF as a
whole maintains it operational capability.
3.92
The committee is satisfied that the provisions of the Privacy Act and
the Australian Privacy Principles appropriately govern the collection, use, and
disclosure of health information in the ADF. The committee notes the concerns
raised by the IGADF and the calls from ADSO and Slater & Gordon Lawyers for
the Privacy Act, as it applies to ADF members, to be reconsidered. However, as the
root of these concerns appears to be ADF members' reluctance to disclose mental
ill-health, the committee does not believe that stricter disclosure laws or a
lessening of ADF members' rights regarding privacy will assist in the early
identification and treatment of mental ill-health. More effort should be given
to addressing the stigma of mental ill-health in the ADF than tampering with
privacy laws.
Recordkeeping
3.93
The committee commends the goals of the DeHS, which, once fully
implemented and integrated with the civilian National e-Health Strategy, will
provide ADF members and veterans with an accurate, easily accessible, and
continuous health record. The committee also notes that Defence is currently
undertaking a review of its health records management policies to consolidate a
'single policy for all ADF personnel that receive health services from
Defence'.
3.94
Accurate health records are vital in ensuring that ADF members receive
informed and targeted treatment for mental ill-health as well as being a
crucial element in the DVA claims process. As such, the committee is concerned
by evidence from medical officers and mental health professionals that it
remains difficult to find relevant clinical information collected or recorded
during deployment.
3.95
The committee acknowledges that there are a range of factors that can
impact accurate recordkeeping, especially on deployment, and that accurate
recordkeeping of ADF members' mental health may also be inhibited by reluctance
to report mental ill-health. However, it is essential that mental ill-health
and potentially traumatic events are accurately recorded during deployment and
that medical officers and mental health professionals can easily access these
records when treating ADF members. It is also important to ensure that veterans
and DVA can easily and quickly access these records when assessing claims.
Recommendation 2
3.96
The committee recommends that the Australian National Audit Office
conduct an audit into the scope and accuracy of recordkeeping of relevant
clinical information collected or recorded during deployment regarding mental
ill-health or potentially traumatic incidents.
Identification of mental ill-health
in veterans
3.97
The committee commends DVA for its 'At Ease' online portal, which
provides comprehensive information regarding mental ill-health to ADF members,
veterans and their families. The committee recognises that veterans are private
individuals who, unlike ADF members, cannot be ordered to undergo mental health
screening or ordered to seek treatment or assistance when they display symptoms
of mental ill-health. DVA is limited in its ability to identify or monitor
mental ill-health in veterans to those veterans who have sought assistance or
made a claim with DVA.
3.98
The committee acknowledges these limitations and notes the calls for DVA
to monitor the health of veterans who have not made a claim. However, any move
to monitor veterans without their consent would constitute a significant breach
of privacy. Nonetheless, whilst engagement with DVA must be initiated by the
veteran, the committee acknowledges that more must be done to encourage
veterans to seek assistance early and to make the process for seeking
assistance simple and swift.
3.99
The committee is very concerned regarding the piecemeal identification
systems for veterans; more must be done to ensure continuity of identification
of veterans, regardless of whether they are clients of DVA. The committee
acknowledges that DVA is working with Defence to implement a single
identification number between the two departments, however the committee
believes that all veterans should be provided with a universal identification
number and identification card that can be linked to the veteran's service and
medical records and utilised by both Defence and DVA, as well as other services
such as the those offered by the Department of Health and Department of Human
Services. All ADF members should be issued with a veteran identification number
and identification card upon discharge. All current and future clients of DVA
should be issued with this number and card and veterans who are not currently
clients of DVA should be actively encouraged to register for the veteran
identification number and identification card.
Recommendation 3
3.100
The committee recommends that all veterans be issued with a universal
identification number and identification card that can be linked to their
service and medical record.
3.101
The ADF Post-discharge GP Health Assessment scheme is an
important tool for the early identification and treatment of mental ill-health;
however it too relies on the veteran to initiate. The DeHS (once fully
implemented and integrated with the civilian National e-Health Strategy) should
provide veterans with an accurate, easily accessible, and continuous health
record. This should ideally allow GPs and other health professionals to
identify that their patient is a veteran as well as allowing them to view
records regarding any mental ill-health concerns or exposures to potentially
traumatic events that may have occurred during the veterans' service.
3.102
Furthermore, annual reminders through the e-health system prompting GPs
to suggest the veteran undergo ADF Post-discharge GP Health Assessment
would encourage veterans to engage with the scheme or even simply provide an
opportunity for veterans to discuss any mental health concerns with their GP. In
the meantime, GPs should be encouraged to promote the ADF Post-discharge GP
Health Assessment to all veterans.
Recommendation 4
3.103
The committee recommends that the Department of Health and the
Department of Veterans' Affairs ensure that e-health records identify veterans
and that GPs are encouraged to promote annual ADF Post-discharge GP Health
Assessment for all veterans.
Navigation: Previous Page | Contents | Next Page