Emma Vines and Rebecca Storen, Social
Policy
Key issue
The 46th Parliament oversaw the launch of new strategies and plans that respond to challenges related to the sustainability, regulation and support of the health workforce. However, concerns continue to arise over these and other issues, such as the registration, distribution, training and retention of healthcare professionals.
The health workforce will need to grow to meet the anticipated demand of an ageing population with increased incidence of comorbidities. Now more than ever, the existing workforce is under sustained pressure due to the COVID-19 pandemic.
In 2020, there were:
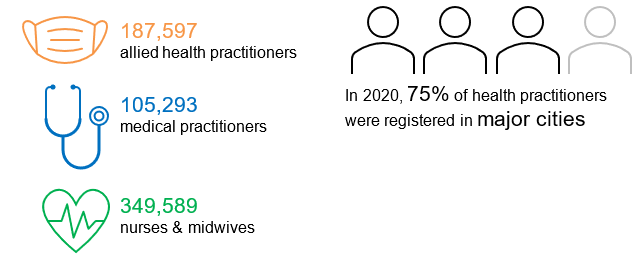
Source: Department of Health, Health
Workforce Data – Dashboard, 2021.
Responsibility for health workforce planning and
most regulation is shared by the Australian and state and territory governments,
with input, especially for training and education, from other organisations,
such as universities and specialist colleges. The Australian Government has
several policy levers available to it that impact the workforce, including:
According to the new National
medical workforce strategy 2021–2031 (Medical Strategy), in 2020–21,
the Australian Government spent $1.5 billion on health workforce and training
programs, with an additional $320 million allocated to universities for CSPs in
medicine (p. 12).
Caring for the workforce
The COVID-19 pandemic has
exposed and exacerbated significant vulnerabilities within the health system as
it has highlighted the challenges of caring for its greatest resource, its
workforce. Although this is not a new issue, the pandemic has focused attention
on it due to the unprecedented pressure people working in the health sector are
under and the anticipated long-term effects this may have on individuals and
the system more broadly.
While responsibility for
the workforce often sits with employers under mostly state and territory
legislation, the sheer scale of some problems, such as burnout, and the
potential risks associated with them, means that an interconnected response is
needed across the sector.
Emotional wellbeing,
burnout and COVID-19
Concerns over health
professionals’ wellbeing have been heightened by the COVID-19 pandemic. As
stated in one article,
‘the staffing crisis is self-perpetuating, creating a vicious cycle. The worse
it gets, the more remaining staff are under pressure’.
Several emerging studies
have examined this issue, with the Frontline Healthcare Workers Study- one of the largest Australian surveys conducted so far during the pandemic- finding that
mental health symptoms had become commonplace among frontline workers with:
- 59.8% of participants experiencing mild to
severe anxiety
- 70.9% experiencing moderate to severe
burnout
- 57.3% experiencing mild to severe
depression.
Another study, which surveyed almost 1,000 Victorian health professionals, found 22.5% reported moderate to severe
depression, 14% reported moderate to severe anxiety and 20.4% reported moderate
to severe post-traumatic stress symptoms, with higher rates reported by
paramedics and nurses. In addition, 65.1% of participants reported emotional
exhaustion, which the authors state reflects moderate to severe burnout. Burnout
has been associated with poorer quality care and patient safety and linked to moral distress in Australian frontline health workers during the
pandemic.
These issues have been noted at a
national level, with initiatives introduced to try to address the increased
pressure on health professionals, including:
Despite these measures, concern remains over the sustainability of the healthcare workforce,
the retention of staff and the quality of service delivery possible from an
exhausted and stretched workforce. It is also
worth noting that emotional wellbeing and
burnout is only one component of caring for the workforce, and issues such as
physical safety and moral distress are equally important considerations.
Regulation of the workforce
The National Registration and Accreditation
Scheme (National Scheme) was
established following the passage of the Health Practitioner Regulation National Law (National Law) in each state and territory parliament
and came into effect in 2010. Under the National Law, 15 national boards are responsible
for registering and regulating the 16 health professions that have ‘protected titles’. The professions with protected titles include doctors, nurses, pharmacists and psychologists.
As part of its function, the Australian Health Practitioner Regulation Agency (Ahpra) manages registration and renewal for health
practitioners and publishes a register of practitioners.
In February 2022, the Health Ministers Meeting agreed to amend the National Scheme through the
Health Practitioner Regulation National Law Amendment Bill. The Bill was
introduced in May 2022 to the Queensland Parliament, as the host
jurisdiction of the National Law.
Some health professions are ‘self-regulated’ (that is, not regulated under the National Law),
including social workers, speech pathologists and audiologists. For healthcare
workers outside the National Scheme, there is a Code of Conduct for Health Care Workers, which establishes expected standards of care and
allows for investigations into alleged breaches of the code. The implementation
and regulation of the code is a state and territory responsibility.
During the last
Parliament, the Senate Community Affairs References Committee conducted an inquiry into the administration of registration and notifications by Ahpra and related
entities under the National Law. The inquiry made 14 recommendations aimed at not only simplifying and amending the registration process,
but also recommending aged care workers, social workers and personal care
workers be included in the National Scheme (pp. xiii–xiv). This recommendation
reflects the position of the Australian Association of Social Workers, which expressed concern that ‘social worker’ was not
a regulated, protected title (p. 7). The Morrison Government did not respond to
the inquiry prior to the election.
Workforce challenges
The provision of a
sustainable health workforce that provides safe, high-quality care to everyone
who needs it is a continuing challenge, and one experienced worldwide that has been made even more difficult with the unprecedented
demands placed on the system and the workforce by the COVID-19 pandemic. This
section briefly considers some of the ‘wicked problems’ associated with the
system, touching on geographic distribution, medical education and training, and
the complex and evolving health system.
Geographic
(mal)distribution
The majority of health
professionals work in major cities, with the number of practitioners decreasing steadily by remoteness area, despite reports
illustrating that people living outside major cities have increased health risk factors, chronic
conditions and higher mortality rates. As illustrated in Table 1, some health
professions are in very short supply by geography, particularly specialists and
psychologists (noting that issues accessing psychologists have been reported across Australia).
Table 1 Employed
health professionals per 100,000 population, by remoteness area, 2018
|
Major cities |
Inner regional |
Outer regional |
Remote |
Very remote |
| Dentists |
57.4 |
40.6 |
35.5 |
27.1 |
21.1 |
| General practitioners |
105.2 |
108.9 |
103.5 |
136.6 |
152.8 |
| Nurses and midwives |
1,030.2 |
1,004.6 |
970.5 |
1,137.0 |
1,191.3 |
| Occupational
therapists |
57.3 |
48.0 |
44.7 |
32.7 |
19.6 |
| Optometrists |
18.1 |
15.7 |
10.8 |
8.4 |
6.9 |
| Pharmacists |
81.4 |
69.3 |
66.8 |
65.3 |
45.7 |
| Physiotherapists |
94.5 |
65.7 |
52.6 |
44.7 |
50.9 |
| Podiatrists |
16.0 |
16.4 |
10.4 |
10.7 |
6.9 |
| Psychologists |
74.6 |
47.7 |
33.5 |
27.1 |
18.5 |
| Specialists |
143.1 |
82.7 |
62.9 |
60.6 |
22.2 |
Notes:
Calculations are based on the FTE clinical rate and report health practitioners
working in clinical practice using the Estimated Resident Population as at
2019. Numbers represent those employed and working in their registered
profession. See original source for all data notes.
Source: Australian Institute of Health and
Welfare, ‘Rural and remote health’ – Figure 3 data table, 2020.
Accessibility to health
professionals by geography is not a new issue, with several policy levers available
to encourage more people to practise in rural and remote areas. Approaches
currently used by the Australian Government include:
- programs to offer students clinical
placements in rural and remote locations – for example, the Rural Health Multidisciplinary Training program
- postgraduate training programs, such as the Junior Doctor Training Program
- financial incentives for health
professionals – for example, the Workforce Incentive Program
- working with the relevant Colleges and the
Medical Board of Australia to recognise ‘rural generalist medicine’ as a distinct field of general practice
- location restrictions on overseas-trained doctors and medical graduates,
limiting where they may practise to access Medicare benefits
- rules associated with CSPs, such as the Bonded Medical Program (BMP), in which participants need to meet their
return-of-service obligations by working in a Distribution Priority Area (DPA)
‘BMP’ location.
Workforce
classifications
The Department of Health uses
the DPA and District of Workforce Shortage (DWS) as health workforce classifications for medical
practitioners (and general practitioners) and medical specialists, respectively.
In general, a location is classified as DPA or DWS if the community has
insufficient access to doctors. However, some locations automatically qualify
as DPA:
A Senate inquiry into the provision
of primary care in regional locations recommended in its interim report, among other things, that the Department of Health
urgently review the Modified Monash Model (p. xiii).
Medical education and
early postgraduate training
The Australian Government
tightly controls the number of medical CSPs, which are allocated to accredited medical schools through funding agreements. While the Government does not impose a cap on the total number of
medical students enrolled, the cap on medical CSPs does significantly impact
enrolment numbers. This approach to CSP allocation by the minister is currently only applied to medical CSPs.
One of the priorities in
the Medical Strategy is to reform the training pathways. The strategy estimates that a
person invests 10–20 years in their medical education before attaining
specialist registration. This training usually includes a medical degree,
followed by an internship, residency and specialist training to meet the
standards to become a fellow of a specialist medical college. In dollar terms,
the overall cost of this training is approximately $1 million to $2.6 million
(p. 45).
The Medical Deans Australia and New Zealand propose redeveloping the medical training continuum
to deliver a sustainable medical workforce that better meets people’s health
needs, which is the right size, shape and distribution (p. 2). The Medical
Deans state ‘in essence, the current training continuum is not delivering the
doctors our communities need and is hindering our ability to prepare doctors
for their roles in the future’ (p. 7 and see Figure 1).
Figure 1 Current and
proposed outcomes for medical training models

Source:
Medical Deans Australia and New Zealand, Training Tomorrow’s Doctors: All Pulling in the Right
Direction, discussion
paper, September 2021, 7.
Internships and an
increased focus on generalist competencies and skills
The Australian Medical
Council (AMC) is currently working on changes to the medical internship training,
which arose from 2 separate, although somewhat overlapping, reviews.
In 2014, the Council of
Australian Governments (COAG) commissioned an independent review of the
existing model of medical intern training with the aim of considering potential
reforms. The final report was released in October 2015. The Australian Health Ministers’ Advisory Council accepted most of the recommendations, including that
internships move to a 2-year ‘transition to practice model’ to emphasise
generalist competencies and skills. At the same time, the AMC had commenced a review of the National Framework for Medical Internship. Given the overlap with
the COAG review, the AMC are undertaking activities to respond to both reviews.
The work to date by the AMC on the 2-year framework indicates that people would be eligible for general registration at the end of their first year and specialist training at the end of
their second year. As part of this shift to a 2-year program, the Medical Strategy ‘proposes that specialist medical colleges reduce the length of
training by recognising prior learning where relevant’ (p. 64).
Postgraduate training
bottlenecks
Despite some calls for an increase in CSPs for medical students to better meet rural workforce needs and decrease
dependency on overseas-trained doctors (p. 6), the later stages of the training
system have limited capacity to absorb additional medical graduates. The Australian Medical Students’ Association has stated ‘there is a significant risk that
increasing medical student numbers, without proportional increase of internship
places and speciality training positions, will detrimentally exacerbate the
bottlenecks we have in training doctors…’. Instead, it called on the Morrison Government
to provide adequate funding for the Medical Strategy, with a specific focus on the
proposed data strategy, establishing an advisory body to inform a holistic
approach, as well as creating additional training places in regional areas.
An increase in medical
graduates with limited consideration of postgraduate training places has previously
occurred (p. 7). At the time, the state and territory governments, which are
primarily responsible for the provision of internships, raised concerns that they did not have capacity to offer places to all additional
graduates. In response, the Morrison Government announced the Additional Medical Internship to increase places for Australian-educated international
students, mainly in private hospitals (pp. 176–7). Postgraduate training places
in private hospitals is an element of the Stronger Rural Health Strategy under
the Junior Doctor Training Program.
Complex and evolving
system
Bulk-billing
As Medicare rules and
legislation become increasingly complex, health professionals are at risk of being
unaware of all rules under the scheme. A small study of medical practitioners concluded that doctors are ‘ill-equipped to manage their Medicare
compliance obligations, have low levels of legal literacy and desire education,
clarity and certainty around complex billing standards and rules’ (p. 1). The first
author, Margaret Faux, has suggested that while the (Morrison) Government stated
that 80–90% of patients are bulk-billed, this may only be occurring properly in around 30% of cases due to doctors misunderstanding the bulk-billing rules. Faux also suggested the high bulk-billing rates promoted by the Morrison Government enabled
it to keep Medicare rebates low.
In its General Practice Health of the Nation, the Royal Australian College of General
Practitioners states that the rate of bulk-billing in general practice has been declining for years, though it noted recent artificial
growth due to COVID-19 items. Indexation of Medicare rebates is shown to have
not kept pace with inflation while patient out-of-pocket costs have increased by
almost 50% in a decade (section 3.2).
Digital technology
Realising the
opportunities and overcoming the challenges of using digital technology in the
health system is not an issue unique to Australia. A recent
OECD (Organisation for Economic Co-operation and Development) report on empowering the health
workforce noted that digital transformation in the health sector is not merely
about technical change, but requires changes in human attitudes and skills, how
work is organised, and legal and financial frameworks. Digital technologies on
their own cannot transform the health sector, requiring health professionals and
patients to put them to productive use.
Services alongside governments
are investing in digital technologies and with
the release of the National digital health workforce and
education roadmap in 2020,
national work has commenced to
support the existing and future health workforce in developing the skills to
realise the benefits of digital technologies. The roadmap envisages a
technologically confident and capable health workforce, and improved
sustainability of the system, while delivering safe and quality care.
A recent joint report led by Deloitte suggests that many people are willing and ready to use
‘virtual care’ (70% of survey participants) and even more are ready to share
their health data in a digitally enabled health system. The authors estimate
that if the system does not change, then the health workforce will need to be 4
times more productive by 2050 to meet forecast demand (see Figure 2).
Figure 2 Current and
anticipated demand on health workers without systemic change

Source:
Baxby et al., Australia’s Health Reimagined (Deloitte, Digital Health Cooperative Research Centre,
Consumers Health Forum of Australia and Curtin University, March 2022), 12.
New and anticipated strategies and plans
The Coalition Government developed
a number of workforce strategies and plans, along with broader plans that
include workforce elements. These include:
The strategies seek to
identify measures for workforce sustainability, health professionals’ wellbeing,
geographic distribution and changing models of care. The focus now shifts to
implementation, which will require commitment, collaboration and ongoing support
and resourcing, and ultimately define the success of these strategies and
plans.
What next?
An effective, sustainable
and accessible health workforce has been a concern for successive governments.
While changes to training and recruitment have been prioritised alongside
high-level workforce strategies, gaps remain. This is particularly the case in
terms of access to health practitioners in regional, rural and remote areas. While
new workforce strategies and frameworks have been welcomed, until they are implemented,
they have little practical impact.
However, it is not only
the pre-pandemic issues that challenge the sustainability of the health
workforce. The last few years have highlighted and heightened issues underpinning
the capacity of Australia’s healthcare system, as well as the incredible
demands placed on health workers. Burnout among health professionals and its implications
is unlikely to be a short-term problem. Addressing this issue will require
resourcing and cooperation across governments and the sector.
Back to Parliamentary Library Briefing Book
For copyright reasons some linked items are only available to members of Parliament.
© Commonwealth of Australia

Creative Commons
With the exception of the Commonwealth Coat of Arms, and to the extent that copyright subsists in a third party, this publication, its logo and front page design are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Australia licence.