Chapter 6 - Access to mental health services
6.1
Access to mental health services was a key issue for
the inquiry. This chapter deals with the role of mental health professionals,
workforce training and shortages and their uneven geographical distribution, government
initiatives intended to overcome these problems, barriers to utilising allied
mental health workers and alternative models of primary health care.
Workforce issues
Psychiatrists
6.2
Psychiatrists are medical practitioners with a
recognised specialist qualification in psychiatry.[441] They work in public hospitals, community
mental health services, private hospitals, and in private practice. The Royal
Australian and New Zealand College of Psychiatrists (RANZCP) stressed the
importance of their leadership role:
Psychiatrists are uniquely placed to integrate aspects of
biological health and illness, psychological issues and the individual’s social
context. They provide clinical leadership with many working in
multidisciplinary team settings. Psychiatrists treat patients and work with the
patient’s general practitioner, other health care providers, families and
carers of patients, and the general community.[442]
6.3
Access to psychiatrists is however very limited. The Australian
College of Psychological Medicine
(ACPM) submitted that private psychiatrists were largely inaccessible because
few bulk-billed, most are located in metropolitan areas and too few psychiatrists
are employed in the public sector. ACPM pointed out:
Most [public psychiatrists] are too busy coping with acute
crises to be able to become pro-active in prevention and early intervention.
Most have no time to deal with the high prevalence disorders such as anxiety,
depression, personality disorders and drug abuse, in the main treating the
individually very demanding schizo-affective range of disorders. [443]
6.4
The RANZCP itself said; 'There is clearly a discrepancy
between the available psychiatric workforce and the mental health needs of the
population'[444]. Dr
Martin Nothling,
a psychiatrist representing the Australian Medical Association (AMA), said this
shortage translated into long waits for patients to see psychiatrists:
...in many cases there can be delays of weeks or months before
someone can be seen because psychiatrists are literally so busy. It is common
talk at any psychiatry meeting you go to where you talk to colleagues—everyone
is booked out. How can you keep seeing patients? You cannot. ... You just
cannot keep adding on patients and working on into the night.[445]
6.5
Several witnesses commented that not many private
psychiatrists bulk-billed, putting access beyond the financial reach of many.[446]
Psychiatrist Professor
Ian Hickie told the committee that the out-of-pocket costs
of seeing a psychiatrist had risen by 49 percent since 1998.[447]
6.6
Difficulty in attracting young doctors to train as
psychiatrists was identified as a serious problem. The AMA indicated that many
psychiatric registrar training positions across the country are not filled by
trainees:
Psychiatrists are among the poorest paid of all medical specialties
and it is not attracting sufficient new entrants which will show up in serious
workforce shortages in later years.[448]
6.7
The Australian Medical Workforce Advisory Committee
found that psychiatry was one of a minority of specialisations in which fewer
people were training than had been recommended, and the only one showing a
decline in numbers.[449] Dr
Nothling told the committee how potential
trainee psychiatrists were put off pursuing a career in the field:
They go into these emergency rooms and they see how dysfunctional
they are. If you have a patient who is psychotic, what do you do? It is
extremely difficult. You spend a lot of time on telephones trying to find a bed
somewhere. You cannot get them in. The treatment they need is in-patient
facilities. They are not available. The emergency rooms get clogged up. The
young doctors see all that and they start thinking, ‘Would you want to be in
this area?’ That is a big problem. Many doctors who have said to me: ‘Look, I
wanted to be a psychiatrist,’ said that once they started to see how the system
was not working decided they would go elsewhere.[450]
6.8
Compounding the shortage of psychiatrists is their poor
distribution geographically, with the majority concentrated in urban areas. The
National Rural Health Alliance (NRHA) observed
that at the general hospitals outside of major urban centres that must deal
with mental health in-patients, there are few or no psychiatrists, and that less
than 3 percent of psychiatrists or psychiatrists in training work outside major
cities and inner regional centres.[451]
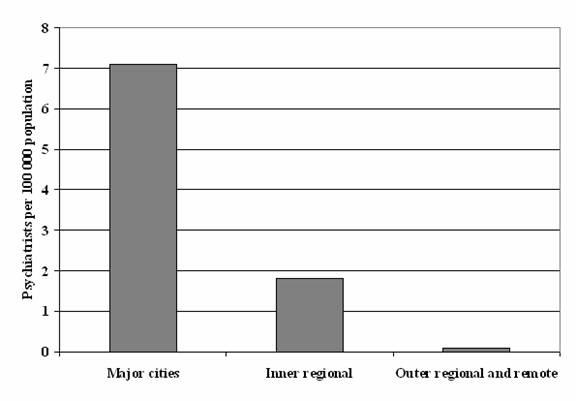
Data from the Australian Institute of Health and Welfare (AIHW) indicates that
whereas there are 7.1 private psychiatrists per 100 000 population
practising in major cities, the equivalent figure for non-major city areas is far
less, with only 1.8 per 100 000 in inner regional areas, and less than 0.1
per 100 000 for outer regional and remote areas. (Figure
5.1)[452] Even within urban areas,
psychiatrists are more likely to be located in more affluent neighbourhoods.[453]
Figure 5.1 Number of psychiatrists per 100 000
population
6.9
Lifestyle appears to be a factor in the maldistribution
of psychiatrists. The RANZCP commented that psychiatrists liked to be close to
fellow psychiatrists to share information and for continuing education
programs.[454] Other evidence pointed
to problems with practising in small communities:
Unless you have a critical mass of psychiatrists on call ... you
are going to meet most of your patients in Coles and your kids
are going to be playing on the football team with some of your chronic patients
et cetera. So there are issues about living in rural communities for mental
health professionals generally that are tricky.[455]
6.10
Initiatives are being taken
to address the lack of psychiatrists in rural and regional areas. These are discussed
further in Chapter 16 in the context of the needs of rural and regional
Australians.
6.11
The practice of psychiatry came in for criticism for its
reliance on a medical model of treatment.[456]
Some witnesses said psychiatrists assessed patients and formed a diagnosis too
quickly and prescribed treatment that was all too often medication and/or
confinement, They were also criticised for not treating the patient with
respect and without taking into account the patient's perspective or broader
needs.[457]
6.12
Mrs Pearl Bruhn, with personal experience of the mental
health system, expressed frustration with the perfunctory treatment sometimes
received:
Psychiatrists, if you are lucky enough to see one, and not just
a medical officer, spend only 15 minutes with each patient, with time only to
discuss medication. There is no time to deal with the many other worries a
patient is likely to have.[458]
6.13
Others complained:
...psychiatrists knew that mania was a possible side effect of
many anti-depressant drugs but they weren’t apparently on the alert for it, and
they apparently did not know how to recognise it, or what questions to ask.
Even after I crashed, they had no idea how to deal with the aftermath, or how
to deal with the devastation caused except to write more prescriptions.[459]
6.14
The Mental Health
Foundation ACT was also critical:
Professionals, especially medical people, still hold power and
authority in our society. Psychiatrists are mainly educated in the medical
model of prescribing medication, but are not necessarily clued into the importance
of the relationship between themselves and their client, although this is
changing.[460]
6.15
The pressure in public hospitals, and emergency
departments in particular, contributed to what was seen as unsatisfactory
psychiatric treatment:
Many trainees are now forced to work on crowded, busy acute
adult inpatient units, where the disorders are generally restricted to three or
four diagnoses. The patients are chronic and almost impossible to treat and the
focus is mainly on the biological therapies.[461]
6.16
Obviously not all consumer experiences with psychiatric
treatment are negative. Consumer advocate, Mr
John Olsen, a
person with schizophrenia, described himself as 'one of the lucky ones' for
whom medication worked. He told the committee of his gratitude to a
psychiatrist (in a prison setting) who coerced him into taking medication, and
established him on the road to a stable life.[462]
Others referred to the positive experience of finding a 'wonderful
psychiatrist' whose care greatly assisted them or family for whom they cared.[463]
6.17
The RANZCP responded to criticisms of psychiatry by saying
that psychiatrists were working with a biopsychosocial model of care that was
consumer-centred:
In the clinical setting, the more information you can get about
someone’s social circumstances and social network and the involvement of their
carers and their families and their own views, quite simply the better able you
are to plan with them what needs to be done and then to implement a plan that
will be successful and acceptable to them.[464]
6.18
Dr Freidin
argued that inadequacies in psychiatric assessment and treatment are often the
result of factors beyond the clinician's control, agreeing that sometimes this
resulted in consumers and carers being marginalised:
We are also aware, though, that practically, in stressed,
under-resourced services, when people do start having to act fast to make
decisions more quickly than ideally they should—for a host of reasons—one of
the things that slips by the wayside is the time that should be taken
to consult in detail with family and with the patient before deciding on an
ongoing management plan. It is a little easier in private practice because one
is a bit more able to control the pace of things.[465]
Mental health
nurses
6.19
Mental health nurses work in public and private
hospitals, community mental health centres and teams, prison mental health
services, and in private medical practices. They are a significant part of the
mental health workforce: in 2001 there were 62.2 mental health nurses per
100,000 population.[466]
6.20
A joint submission by peak nursing representative
bodies, the Association for Australian Rural Nurses (AARN), the Australian and
New Zealand College of Mental Health Nurses
(ANZCMHN) and Royal College of Nursing Australia (RCNA), identified the current
nation-wide shortage of psychiatric nurses as critical, and affected the
ability of nurses to do their jobs properly:
The mental health nurse may be so overburdened by their workload
that they are unable to perform their roles to its fullest potential, and are
themselves being exposed to stress and anxiety. Staff going on leave,
especially in community services, are usually not replaced resulting in the
remaining staff not having the time to follow up all of their clients.[467]
6.21
This joint submission from nursing peak bodies also
pointed out that the workforce shortage is more marked in rural, regional and
remote areas:
There are a higher proportion of mental health nurses in the
capital cities and very low numbers in smaller regional and remote areas
(Australian Institute of Health and Welfare 2001). The shortage further
compounds the under-servicing of rural and remote locations.[468]
6.22
The numbers of mental health nurses in major cities,
inner and outer regional areas and remote and very remote are shown in Figure
5.2.[469]
Figure 5.2 Number of mental health nurses per
100 000 population

6.23
Submissions referred to the difficulty in recruiting
and retaining nurses in the field of mental health. The ageing of this
workforce was noted as a significant problem, with mental health nurse Mr
Jon Chesterson
observing that:
...the average age of the mental health nursing workforce is
47+, and more than half of the existing workforce is expected to retire within
the next 15 years. The pitifully small trickle of new graduates into mental
health today compared with the late nineteen seventies and early eighties has
already resulted in a workforce crisis.[470]
6.24
The Health Services Union pointed out that the bulk of older
nurses are graduates of the former direct entry psychiatric nursing courses.[471] Unlike their older colleagues, nurse
trainees today must first undertake a three-year generalist nursing degree (with
very limited content on mental health theory and clinical practice)[472], followed by post-graduate studies
in mental health nursing. Thus there is a reliance on generalist graduates
being attracted to pursuing further studies in mental health. The committee
heard that this was not happening to a sufficient extent. The NSW Nurses'
Association commented that 'the appeal of the sector to new graduates is
diminishing.'[473] Stressful working
conditions and significant levels of violence in the mental health workplace
were mentioned in several submissions as negative factors.[474] The AMA commented:
...nurses are not being attracted to work
in psychiatry because the system is dysfunctional and because of security
problems. It is a common theme across the nation that nurses and doctors
attending severely disturbed patients are being assaulted at a rate which
is causing concern and public discussion amongst these groups.[475]
6.25
A study of a psychiatric unit at one hospital in NSW
revealed high levels of violence and aggression, and pointed to the heavy toll
on mental health nurses:
[Psychiatric] Units where high levels of aggression and violent
behaviour are experienced in the workplace on a daily basis must be
acknowledged as dangerous workplaces. Staff work continuously under elevated
stress levels (physical, mental and emotional). Staff locked in [these] units
for eight hours per day for five shifts per week with aggressive patients must
pay a toll in some way. [476]
6.26
To address the problems of recruitment, the joint submission
from peak nursing bodies argued that mentoring in mental health nursing needed
to be provided to encourage already practicing nurses into the field, and that funding
incentives were also required:
It is ... important that appropriate funding be made available
for transition programs specifically for mental health ... for newly graduating
nurses coming into the workforce, to attract them into this specialty field.[477]
6.27
The shortage of mental health nurses has been the
subject of many reviews and studies. Submissions made reference to the 2003
report of the Australian Health Workforce Advisory Committee, Australia Mental Health
Nurse Supply, Recruitment and Retention.[478] This report made a number of recommendations
to address workforce shortage issues, including that an agreed framework for
mental health content in undergraduate general nursing degrees be developed.[479] The committee notes the recent
Victorian State Government Victorian
Taskforce on Nurses Preparation for Mental Health
Work Report (September 2005), which recommends, amongst other things, the trial
of a specialist university degree with a major in mental health.[480]
Psychologists
6.28
The greater role that could be played by psychologists,
particularly clinical psychologists, in Australia's
mental health workforce was a strong theme in the inquiry.
6.29
Psychologists, as defined by the Australian Institute
of Health and Welfare, consult with individuals and groups, assess
psychological disorders, and administer programs of treatment.[481] They do not prescribe medication,
and according to the Australian Psychological Society (APS), have spearheaded
the development of non-pharmacological treatments.[482] There are several different
specialisations within psychology, all requiring additional post-graduate study
and training. The APS advised of a number of specialist affiliated colleges covering
the fields of clinical, community, counselling, educational and developmental,
organisational, neuropsychology, and health psychology.[483] The committee received evidence that
psychologists can play an important role in the assessment and treatment of mental
disorders.[484]
6.30
The public sector is a major employer of psychologists,
particularly in community mental health teams. Yet evidence from representative
psychologist bodies suggests that psychologists in these teams are increasingly
employed in generic positions as 'case managers' or 'allied health workers', and
not providing psychological assessment and treatment for which they are
trained.[485] Many are too busy dealing
with clients with serious mental illness to be able to provide effective early
intervention 'upstream' treatment, or to provide treatment to those with high
prevalence disorders such as depression. The Victorian Section of the APS
explained:
Mental health services are currently only available to those
with the most severe mental health disorders. Many people suffering from
complex and disabling psychological problems, including disorders of high
prevalence, are unable to access psychological treatments in the public mental
health sector, despite evidence of their effectiveness. In addition, the long
waitlists and increasing caseloads present in continuing care mental health
teams mean that little or no opportunity is available for clinical
psychologists to provide early intervention and relapse prevention.[486]
6.31
Clinical Psychologist Dr Jillian Horton
argued that public mental health services should maintain the capacity to
provide psychological treatments by making more positions available for clinical
psychologists:
There needs to be many more positions available to six year
trained Psychologists in Community Health Centres and public mental health services
so that consumers can access these services. Psychological therapy positions
should not be down graded into generic mental health worker positions or to
other professions with short training in a limited number of psychological
therapy skills.[487]
6.32
Better access to psychologists was not only supported
for its potential to increase the scope of mental health services but also for
helping to provide a better balance between 'drug-therapy' and 'talk therapy'.
Some submissions expressed a view that medication as a treatment was sometimes
overused by both psychiatrists and GPs, and that non-pharmacological treatment
was often effective as an alternative or in combination with medication. The Western
Australia Section of the College of Clinical
Psychologists – APS - submitted that:
Research from overseas indicates that most consumers with less
serious mental health problems do not receive adequate care for their mental
health problems from GPs and this can lead to a worsening of their mental
health problems. Research also indicates that GPs tend to prescribe medication
for less serious mental health problems which adds to the high cost of medical care,
yet these individuals could be treated as effectively (and sometimes more
effectively) by psychological interventions provided by clinical psychologists.[488]
6.33
Beyondblue argued:
Non-pharmacological treatments, such as cognitive behaviour therapy,
are effective and therefore need to be more accessible to the general community
through improved access to psychologists and allied health.[489]
6.34
Access to psychological services was perhaps the single
biggest issue about which the committee heard evidence. In the private sector,
many psychologists registered to practise offer a range of psychological
treatment for mental health problems. However, as many submissions pointed out,
access to these private-sector services was beyond the financial reach of many.
The cost of a one hour sessions with a psychologist usually ranges from $100 to
$175[490] for which there is no
Medicare rebate, unlike consultations with private GPs and psychiatrists. The Mental
Health Association of NSW pointed out that 'people with
depression often want a choice between medication and counselling, but find
that their only access to counselling is through private practitioners, and
Medicare does not cover these services'.[491]
The Public Health Association of Australia commented that:
...for most people with mental disorders, clinical psychologists
in private practice are only accessible to those with the ability to pay. This
is therefore a greatly under-utilised resource, particularly as many of the
newer psychological treatments are provided by this group of mental health
professionals.[492]
6.35
This issue of whether or not governments should fund or
subsidise access to psychological treatment in the private sector, either
through Medicare or in some other way, was a recurrent theme of the inquiry. This
matter is discussed in more detail in a later section of this chapter.
6.36
The committee notes that private health insurance (ancillaries
cover) can provide some reimbursement of costs for psychological services, but the
benefits paid cover only a small portion of the cost paid for the service[493] and many people needing mental
health services are socially and financially disadvantaged, and cannot afford
private health insurance.[494]
General
practitioners
6.37
GPs are the first point of professional contact for a
great majority of people seeking help with mental health problems.[495] Although
research suggests that only 38 per cent of those with mental health problems
seek help, of those that do, 75 per cent do so in the first instance from
a GP.[496] Many with chronic physical
conditions visiting GPs frequently also have comorbid mental health conditions
such as depression and anxiety.[497] The
role of GPs in mental health is especially significant in rural and remote
areas, where there are often no other health workers.[498]
6.38
Dr Rob Walters of the Australian Divisions of General
Practice (ADGP) told the committee that 'it is general practice and not the
specialist mental health system that delivers the greater majority of mental
health care in this country', with over 10 million general practice visits in
2003-04 related to mental health.[499] Most
people with high prevalence disorders such as depression and anxiety are seen
by GPs.
6.39
The role of GPs as a 'gateway' to other services was
mentioned in a number of submissions.[500]
The AMA submitted that:
General Practitioners (GPs) are the most accessible medical
resource in the community and are the gatekeepers to other community resources
such as specialist psychiatric care and acute care.[501]
6.40
The ACPM argued that, because of the limited access to
psychiatrists and psychologists, GPs were significant providers of mental health
care, especially to the financially disadvantaged:
General practitioners ... have to provide a large proportion of
mental health services in this country. It cannot be overemphasised that the
mental health services general practitioners provide are to the most
financially needy, those who cannot access the private sector, and those with
the most difficult diagnoses in terms of their social impact – those with
chronic as opposed to acute problems who therefore cannot access the
crisis-focussed public system either.[502]
6.41
GPs should not be regarded as the last resort in
service provision. The AMA argued:
[It is necessary to] Recognise that GPs will not be able to
‘pick up the pieces’ when other mental health services, public specialist
mental health services in particular, are not able to provide sufficient
services to their consumers, particularly those with supposedly less serious mental
illnesses and those in extreme disadvantage, including financial disadvantage.[503]
6.42
In recognition of the reliance on GPs for the provision
of primary mental health care, the Australian Government in 2001 introduced and
funded the Better Outcomes in Mental Health
Care initiative (Better Outcomes). Better Outcomes provided education and
training for GPs in mental health, improved access to psychiatrist support for
GPs, and funded referrals to psychological services in private practice. Evidence
to the inquiry indicates that Better Outcomes has been a useful initiative,
though take-up by GPs and caps have limited its distribution. Better Outcomes is discussed in more detail
later in this chapter.
6.43
The Inquiry into the Human Rights of People with Mental
Illness in 1993 (the Burdekin Inquiry) had found that the training of GPs in
mental health was inadequate, and that they often failed to identify mental
illness.[504] The inquiry recommended
that GPs receive more comprehensive mental health education.[505] One of the results of Better
Outcomes has been an improvement in the mental health care skills amongst the
approximately 20 per cent of GPs who have undertaken
training. Several submissions argued that curricula at the undergraduate level
and in GP registrar training were deficient in mental health assessment skills
and care.[506] The ADGP suggested that the
training provided in Better Outcomes should be incorporated into GP registrar
training.[507]
6.44
It was argued that the general practice fee structure
for Medicare rebates discouraged the long consultations often required when
dealing with patients with mental health problems.[508] The Royal
Australian College
of General Practitioners (RACGP) submitted that more effective and
comprehensive care was achieved within longer consultations, yet the GP
consultation item structure encourages shorter consultations.[509] Evidence from the ACPM indicated
that a GP dealing with usual medical problems could normally see four or more
patients in the same time that they could consult with one patient with a
mental health problem.[510]
Other
professional groups
6.45
Social workers and occupational therapists are often
members of community mental health teams, performing case-worker and other
roles. However, the committee received little evidence regarding these
professional groups. Training courses for a relatively new group – Aboriginal
mental health workers – is addressed in Chapter 16 in discussion of the needs
of Indigenous people.
6.46
A submission from Psychotherapy and Counselling
Federation of Australia (PACFA) argued that the counsellors and
psychotherapists they represented (different from psychologists) were
under-utilised in the mental health field:[511]
Counsellors and psychotherapists are unique within the mental
health field with respect to undertaking in-depth training, usually at a
post-graduate level, in counselling and psychotherapeutic theory and skills, as
well as their mandatory requirements for ongoing clinical supervision for the
duration of the therapist’s career.[512]
6.47
PACFA argued that PACFA-registered practitioners should
be granted the GST-exempt status applied to psychologists and GPs, and should be
included in Better Outcomes. Such inclusion, PACFA argued, would 'provide a
much needed addition to the severely stretched mental health system and provide
greater consumer choice, and better mental health outcomes.'[513]
6.48
There are also non-health professionals who, in the
course of their work regularly encounter people with mental health problems.
Teachers are often the first to identify mental health problems in young
people; police officers are often relied upon to transport people with mental
illness to hospital; government agency employees deal with people affected by
mental illness; and family members are usually integral in care arrangements.
6.49
The Burdekin Report in 1993 recommended mental health
training for a broad range of professionals in the community and Mental
Health First Aid training is now available, increasing
knowledge, reducing stigma, encouraging supportive responses and assisting with
early intervention and the ongoing support of people with mental illnesses.[514]
6.50
Professor Tony Jorm and Ms Betty Kitchener (the
originator of the Mental Health First Aid
course), put the case that the course has been proved to be effective, and
recommended Australian Government funding to support and train a national cohort
of instructors:
Once these are trained, the program can be self-supporting just
like conventional first aid courses. For example, to train 100 additional instructors
and to provide seeding support for them would cost around $400,000. These
instructors would then train people who are outside the mental health sector,
but have an increased probability of contact with mental health issues. These
groups include teachers, nurses, welfare workers and family carers.[515]
6.51
The committee supports the idea of training in mental
health for the wider community, and notes that Mental Health
First Aid training can not only assist professionals such as teachers and
police, but can also reduce stigma in the community, as a result of the greater
general awareness of mental health issues in the community that results. The committee
heard, for example, about the provision of mental health support training for
hairdressers in Horsham, Victoria[516] – an excellent example of a group
who talk to a lot people in their community and who could thus benefit from
mental health first aid knowledge.
Initiatives that can improve access to better mental health care
6.52
In recognition of the need to increase the mental
health skills of the existing GP workforce, and the need to improve access to mental
health and allied health professionals, a number of initiatives have been
developed in recent years. This section of the chapter looks at these
initiatives, and discusses their achievements as well as some criticisms that
have been levelled. In particular, this section examines the following
initiatives:
-
Better Outcomes in Mental Health;
-
Chronic Disease Management Medicare items; and
-
More Allied Health Services program.
Better Outcomes
in Mental Health
6.53
The stated aim of the Better Outcomes initiative was
'the achievement of better outcomes for people with mental health problems by:
providing GPs with training; introducing incentives to GPs for delivering
structured, quality care; and enabling access by GPs and consumers to allied
health professionals and psychiatrists.'[517]
The initiative has been funded by the Australian government since 2001-2002 and
has five related components:
-
education and training for general practitioners
to familiarise them with the initiative and to increase their mental health
care skills and knowledge;
-
3 Step Mental Health
Process which rewards best practice mental health care by general practitioners
by providing remuneration for assessment, care planning and review of consumers
with mental health problems;
-
increased remuneration to general practitioners
for the extra time they spend with mental health consumers providing focused
psychological strategies;
-
access to allied psychological services to
enable general practitioners registered with the initiative to access focused
psychological strategies for their consumers from allied health professionals;
and
-
access to psychiatrist support for GPs by
providing remuneration to psychiatrists who participate in case conferencing
with other health providers, and who provide mental health consumer management
advice via the GP Psych Support service.[518]
6.54
The training component involves two levels:
-
Level One skills based training in managing
mental health disorders in general practice (six hours of training), and
-
Level Two training in extending skills in
psychological treatment such as counselling and therapy (20 hours of training).
These psychological treatments are known as Focussed Psychological Strategies (FPS)
under the Better Outcomes, and include treatments which are evidence-based. That
is, there is evidence to prove their effectiveness. Specific psychological
treatments included are cognitive behaviour therapy, interpersonal therapy, and
psycho-social education.
6.55
Once trained and credentialed, a GP can deliver these
treatments as claimable items under the Medical Benefits Schedule (MBS). The specific
MBS item numbers allow greater remuneration for the longer time spent in
consultation, such as for consultations over 40 minutes that are used to
provide focussed psychological strategies.[519]
6.56
In the 3-step Mental Health
Process GPs make a patient assessment, devise a care plan, and review progress.
On completion, GPs are entitled to a Service Incentive Payment (SIP) of $150. The
GP Psych Support service operates nationally 'to provide all general
practitioners with telephone, facsimile and email access to quality consumer
management advice from psychiatrists, within a 24 hour timeframe, seven days a
week'.[520] Also under this component,
psychiatrists are remunerated for case conferencing with GPs.
6.57
The component of Better Outcomes which attracted the
most comment during the course of the inquiry was Access to Allied Health
Services, which allows GPs who have completed Level One training to refer a
patient to allied health professionals under arrangements whereby the out-of-pocket
cost to the patient is nil or is a small co-payment, usually less than $10. The
great majority of referrals have been to psychologists, although the eligible
professional groups include social workers, mental health nurses, and
occupational therapists.[521] Referrals
in the first instance are for six visits, with an additional six visits allowed
subject to a review by the GP.
6.58
The Australian Government funds the Access to Allied
Health Services through Divisions of General Practice around Australia,
who then make their own funding arrangements with allied health services. Most commonly
this is either by individual contract, or by direct employment.[522] In Round 1 of the pilot stage of the
program, 15 Divisions received funding for Access to Allied Health Services
projects. In 2005 over 100 of Australia's
118 Divisions took up the initiative and receive funding.[523]
6.59
Uptake by GPs in the three years since the program
began has, according to the ADGP, far exceeded initial predictions of GP
interest,[524] if not government
projections. Data indicates that 20 percent (one in five) GPs had completed
training and registered.[525]
6.60
The ADGP submitted that:
The allied health component has been a particular drawcard for
GPs who have found that better access to allied health support has resulted in
improved clinical outcomes for patients and improved management in the primary
care setting.[526]
Of all the measures funded by the federal government under
recent national mental health plans, Better Outcomes has been a relative policy
success, a success that has been consistently supported by all national mental
health stakeholders...[527]
6.61
Local evaluation reports compiled through ADGP showed
that participating GPs, allied health professionals and consumers were 'very
satisfied' with the evolution of services through Better Outcomes.[528] ADGP commented that the nation-wide
Divisions of Practice have been instrumental in driving reforms and encouraging
GPs to take up the initiative, and they have called for the capacity of the
Divisions Network to be expanded to improve the delivery of mental health care
to better meet community needs, including access to health care by key groups:[529]
The
network, which is already in place and funded, is a unique infrastructure and
agent of change that can build and support GP led sustainable primary mental
health care teams, support primary mental health care work force development,
promote coordinated and integrated care by linking general practice with other
systems, deliver quality primary mental health care services, deliver models of
service delivery tailored to local contexts and reach rural and regional
Australia.[530]
6.62
Concerns have been expressed about the limitations of
Better Outcomes, including:
-
Insufficient take-up by GPs;
-
Difficulties for rural GPs in undertaking Better
Outcomes training;
-
The need for GP practices to be accredited;
-
Adequacy of 20 hours training in psychological
treatment;
-
Lack of access to psychologists in rural and
remote areas;
-
Limits placed on the number of patients GPs can
treat and refer;
-
Conflict of interest in pharmaceutical companies
funding training; and
-
The need to remove disincentives for longer
consultations by GPs.
Insufficient
take-up by GPs
6.63
Despite the positive reaction by GPs, it is
nevertheless the case that only one in five GPs has undertaken
at least Level One training. Thus four in five GPs – often including those with
the least expertise in mental health - are not eligible to refer patients to a
psychologist under Better Outcomes.
6.64
It was suggested that the take-up so far was largely by
those GPs who already had an interest in mental health, and saw registering
with Better Outcomes as part of their continuing interest and professional
development and that GPs whose interests lay outside of mental health would be
unlikely to undertake the training. [531]
6.65
It certainly appears that the proportion of GPs
credentialed under Better Outcomes is unlikely to rise. The Department of
Health and Ageing indicated that 'the number of additional general
practitioners (GPs) who will complete Level One training under the Better
Outcomes in Mental Health Care Program is
about 150 each quarter and the number of GPs who will complete Level Two
training is about 50 per quarter'.[532]
While 600 GPs are completing Level One training each year, this seems no higher
than the annual rate of turnover in the profession. In 2004, 557 places were
filled in the General Practice Training Program,[533] and in addition to these new
entrants, some doctors are recruited directly into the system as general
practitioners from overseas. Thus the rate at which doctors are being credentialed
for Better Outcomes Level One is no greater than the rate at which new doctors
are entering the system, while the rate of training at Level Two may mean that
the proportion of doctors accessing this option will actually fall.
6.66
The paperwork in the 3-step process was cited as a
disincentive to take-up and, in particular, GPs were frustrated with the 'red
tape' and paperwork required to claim the Service Incentive Payment (SIP) of
$150. In recognition of these concerns, changes were made by the government in
May 2005, allowing the process to be completed in two consultations rather than
three. Nevertheless, take-up by GPs has been less than expected, resulting in a
reduction in the forward estimates for funds earmarked for SIPs of $85.4
million over four years.[534] The
Department of Health and Ageing told estimates hearings that in addition to the
revised 3-step process, other changes were being contemplated to try to improve
the take-up and make the process easier to use[535] and said in its submission to this
inquiry:
...more needs to be done, especially in terms of engaging more GPs
to use the components available in the Better Outcomes initiative. In
recognition of this the Australian Government has committed $228.5 million over
four years from 2005- 09 in supporting GPs in their role as primary carers of
people with mental illness.[536]
Difficulties for
rural GPs in undertaking Better Outcomes training
6.67
A further barrier to take-up by GPs according to some
submissions was the fact that it was difficult for GPs in rural and remote
areas to take time away from their practices to attend training, often
conducted in a city, as it could leave a town without any medical care. The
South Australian Divisions of General Practice submitted that:
The more remote Divisions report considerable difficulty
accessing the required training for their GPs to participate in the [Better
Outcomes] scheme... Training of GPs to do counselling themselves (Level 2 under
[Better Outcomes]) is likewise difficult as it requires the GP to do 20 hours
of training – not available in the country thereby necessitating the GP to
leave their practice unattended for a number of days. With the lack of
available locum coverage to backfill, and rural doctors required to provide
after-hours emergency care, this may leave entire towns and regions without any
medical care.[537]
6.68
The associated costs of travel, and of finding a locum,
were also a disincentive for rural GPs:
At present, there is no alternative for a rural or remotely
located GP but to travel to a regional or major centre in order to undertake
the entry point training for the Better Outcomes initiative (Level One or Two
accredited training). The travel requirements impose a significantly greater
burden on rural and remote GPs who often have difficulties finding and funding
a locum GP to service their area during their absence, and of course incur substantial
travel, accommodation and loss of income costs.[538]
6.69
The GPMHSC suggested that some accredited Level One
Better Outcomes training packages could be adapted for online or distance
delivery, but also recognised that face-to-face training was preferable. The
GPMHSC recommended that there be financial support provided for rural GPs
needing to travel to undertake training, and incentives for training providers
to deliver training in non metropolitan areas.[539]
The need for GP practices
to be accredited
6.70
Another barrier to GP take-up of Better Outcomes is the
requirement that for a GP to be eligible for the Service Incentive Payment, the
3-step mental health process consultations must be provided from a practice
participating in the Practice Improvement Program (PIP) or an accredited
practice.[540] The ACPM pointed out
that this requirement excludes qualified medical practitioners who for various reasons
do not see patients at an accredited practice – for example they may work at a
university medical centre. The requirement can also lead to anomalies:
[The requirement can result] in the absurd situation where some
practitioners are registered in one site and not in another. As an example the
College can cite a member ... who works in two accredited practices. In one, he
uses a room which is part of the accredited practice. In the other, the
consulting room which he rents is not physically part of the accredited practice
- it is in the same building but in a part designated as the Specialist Centre.
In that practice he cannot be registered for [Better Outcomes] despite doing
the same work and having the same qualifications (namely a Masters
degree in Psychological Medicine and additional qualifications) in each
setting![541]
6.71
The costs and resources associated with achieving
accredited status were also a barrier for some practices. Fundamental
reorganisation of practice structure could be necessary, which was a disincentive
for many.[542] The Northern Territory Government
said this was a particular issue for practices in the Northern
Territory:
While the Australian Government’s ‘Better Outcomes in Mental
Health Care’ initiative attempts to increase the capacity of
GPs to provide mental health care, the success of this initiative in rural and
remote areas of the NT has been marginal. Although a number of GP practices and
Aboriginal controlled health services in the NT were initially accredited and
accessed training, fewer practices are
now making that commitment due to the costs associated with achieving the
expected standards and the relative benefits for individual practices. The
uptake rate in the NT has been confined to a small group of Darwin
based GPs.[543]
6.72
The AMA and the ADGP pointed out that the practice
accreditation requirement excluded many Aboriginal Medical Services and
youth-specific services[544] yet these
were some of the highest need populations in the community.[545] The ADGP recommended exception criteria for GPs working outside
accredited practices, particularly those working with these high need groups.[546]
6.73
It was also pointed out that Better Outcomes
accreditation operates independently of other accreditation and professional
development for GPs. RACGP suggested:
At the moment the accreditation processes for mental health
training are separate from the RACGP quality assurance and continuing
professional development program. In the future it would make good sense to
roll these into one so that GPs do not have separate accreditation for mental
health and all their other areas of education. It makes sense to roll these
into the one QA and CPD program.
6.74
The committee agrees, and hopes that such streamlining
might encourage some more GPs to take up Better Outcomes accreditation.
Adequacy of 20
hours training in psychological treatment
6.75
A view strongly expressed to the committee was that the
20 hours of training comprising Level Two training was inadequate to equip GPs
with the necessary skills to provide effective psychological treatment (Level
Two training covers specific psychological treatments including cognitive
behaviour therapy). Organisations representing psychologists were adamant that
20 hours of training could not be considered the equivalent of the many years
of study and clinical supervision undertaken
by psychologists in order to register to practise. The APS submitted that:
The techniques that GPs are expected to master in 20 hours are components
of those required of psychologists to be registered to practise. Psychologist's
training for registration involves a four-year university degree in psychology,
two years post-graduate study (usually a Masters degree) and
at least one subsequent year of clinical supervision (at least six years
training). We believe that twenty hours of instruction in psychological therapy
techniques is not adequate training and does not meet appropriate professional
standards for mastering the skills for effective psychological intervention.[547]
6.76
The Association for Counselling Psychologists commented
that the 20-hour Level Two training for GPs has been seen by psychologists as
the equivalent of allowing psychologists to undertake brief training in
medicine in order to prescribe drugs,[548]
and argued that the delivery of psychological interventions should be reserved
to appropriately qualified licensed and experienced mental health specialists.[549]
6.77
There was some evidence that GPs were not necessarily
using the psychological treatment skills they had obtained under Level Two
training, but preferred to refer patients on to psychologists. Professor
Ian Hickie
told the committee that the training often had the effect of making a GP more
likely to refer on, rather than deliver the service him or herself:
What you see is that those GPs who have undertaken further
training actually make more referrals, not fewer referrals. There is a belief
system, which I think is quite wrong, that if GPs get more access to these
items themselves or further training they will not refer. All the research
evidence shows the opposite. The better trained people are, the more aware they
are of what they cannot do and the more aware they are of options and of what
others can do.[550]
6.78
At December 2004, almost 2000 GPs had referred almost
13 000 consumers for focussed psychological care by allied health
professionals, and almost 50 000 sessions of therapy had been received by
consumers.[551] GP-provided focussed
psychological strategies totalled over 33 500 for the period January 2003
to December 2004.[552]
6.79
A number of submissions commented that, with a shortage
of GPs in Australia,
it made sense to utilise the workforce of psychologists, rather than further
burden the already overstretched GP workforce.[553] Dr
Jillian Horton
commented that the long consultations required to deliver psychological treatments
were time-consuming for GPs, and encroached on their medical practice:
There is already a shortage of GP hours for medical care, and consumers
often complain about the difficulty in getting medical appointments. Why would
the Federal Government wish to burden this sector further and make the hours
for medical care even less available to the public, when there are clear
alternatives? Wouldn’t supporting a way to ease and re-direct the mental health
burden from GPs make more sense?[554]
6.80
Psychologists argued that the Medicare item numbers
used by GPs to deliver psychological treatments should also be available to
six-year trained psychologists:
Enabling psychologist access to the Medicare items for Focussed
Psychological Strategies ... would ease the mental health burden through
mobilisation of a significantly under-utilised trained psychology workforce.[555]
6.81
Whilst there appears to be general support across the
health professions for the idea of making better use of psychologists in the
provision of mental health care, there is some debate over how best to achieve
this, whether it should be through direct or indirect access to Medicare items
by psychologists, or through some other method. This matter is discussed
further in a later section of this chapter.
Lack of access to
psychologists in rural and remote areas
6.82
A number of submissions pointed out that although GPs
welcomed the Access to Allied Health, the program fell down when no suitable
professionals were available. This problem was most pronounced in rural and
remote areas.
6.83
The South Australian Divisions indicated that their
more remote Divisions had considerable difficulty in attracting appropriately qualified
and experienced personnel. [556] The ADGP observed:
...regional and rural Divisions face challenges such as
attracting suitably credentialed allied health workers to their communities.
This is often due to the availability of relatively short term (annual)
employment contracts. Recruitment and retention challenges are compounded by
Better Outcomes’ current status as a lapsing program which means it is
difficult for divisions to offer ongoing positions to allied health
professionals and facilitate recruiting and retaining them in rural and
regional centres.[557]
6.84
The South Australian Divisions suggested:
Some requirement or enticement for allied health workers to do
some rural service, either as a fly-in model, or for a limited period of time,
would also be welcome to address the workforce difficulties.[558]
Limits placed on
the number of patients GPs can treat and refer
6.85
The Better Outcomes framework imposes a cap on GPs and
their use of the Medicare items, presumably to control the budgetary
implications of the program. The cap limits GP's claims for individual services
(completed 3-step processes) to $10 000 per year per GP, which is the
equivalent of 67 mental health plans.[559]
6.86
Professor Hickie
argued that the cap discouraged GP practices from undertaking the practice
reorganisation needed to participate in the program:
The biggest disappointment from a GP point of view is what we
see as the cap on the number of services. The Commonwealth rejects this as an
issue, but what you want here is fundamental practice reorganisation, for GPs
to alter the way they work. In fact, if you say there will be a limit to the
number of people whom any individual or practice can service then you get a fundamental
disincentive. So there has not been the degree of GP practice reorganisation
that we would have hoped for...[560]
6.87
The government indicated that in 2004-05 only 17 GPs
out of over 4 000 who are trained had reached the cap.[561]
6.88
This was however not the only cap within Better
Outcomes that attracted criticism. Another cap limits the number of referrals
GPs can make under Access to Allied Health Services by limiting funding within individual
Divisions. The AMA submission expressed this concern:
[The] counselling component is subject to capped funding and GPs
are very limited in the numbers of services that they may refer patients to,
some Divisions reporting that they can only refer 5 patients per annum.[562]
6.89
The ADGP argued that allied health services are popular
with GPs, allied health providers and consumers, but that demand is far
outstripping supply. The ADGP called for an increase in funding for allied
health,[563] and pointed out the
inconsistency:
It is perverse that GPs belonging to Divisions who have worked
hard to enrol a large number of GPs in the program are then penalised when the
available allied health services are 'rationed' due to capped funds.[564]
Conflict of
interest in pharmaceutical companies funding training
6.90
The committee was told that pharmaceutical companies
are involved in funding for training in Focussed Psychological Strategies
(FPS). The appropriateness of this was questioned:[565]
The financial involvement of pharmaceutical companies in FPS
training is also a matter of serious concern. ... Such involvement represents a
grave conflict of interest that undermines the focus of FPS training.[566]
6.91
The concern originates in part from the tension that
currently exists between professional groups and their different approaches to
treatment, as well as an understandable concern about the motives of
pharmaceutical companies in funding training in non-pharmaceutical treatment
options.
The need to
remove disincentives for longer consultations by GPs
6.92
While Better Outcomes attempted to address the
financial disincentives to GPs for conducting the long consultations often
necessary when caring for people with mental health problems, the ACPM argued
that:
While the [Better Outcomes] item numbers redress [the
disincentive problem] to some extent their use is limited and not always
applicable...
The
College recommends that an extension of item numbers to recognise and reward
those performing more complex services should be introduced as a matter of
urgency. This should include item numbers for longer consultations, preferably
up to two hours in duration, as exist for psychiatrists and for ongoing
psychological care of patients with complex problems.[567]
6.93
The submission from bluevoices (the consumer body of beyondblue)
recommended a further increase in the rebate for longer consultations:
Beyondblue/blueVoices acknowledges the advances made in General Practice
in the Better Outcomes in Mental Health Care
Initiative, and recommends that in subsequent budget cycles, the level of
rebate offered to General Practitioners offering high quality mental health
services to consumers was increased even further. There must be a reduction in
the incentive to reward doctors for the number of patients they see each hour, when
it is widely accepted that the volume of patients seen does not equate to good
health care.[568]
Multidisciplinary
care planning, and Medicare items for chronic disease management
6.94
Historically, Medicare has only provided rebates for
services delivered by doctors.[569] In
recent years, however, the Australian Government has experimented (in a limited
way) with broadening the rebate to services delivered by allied health
professionals, such as psychologists, practice nurses, physiotherapists and
podiatrists.
6.95
Under Chronic Disease Management (CDM) Medicare items,
GPs can involve allied health professionals in the care planning of patients
with chronic and complex care needs, including patients with mental health
problems. The CDM items replaced (in July 2005) Medicare items for Enhanced
Primary Care (EPC). Medicare rebates are available for a maximum of five allied
health services per patient in a 12-month period, following referral from a GP.
Allied health professionals eligible include psychologists, Aboriginal health
workers, occupational therapists, physiotherapists, and podiatrists. An allied
health professional must be registered with Medicare Australia
to provide Medicare rebateable services. The allowable five visits per 12-month
period can be to different allied health professionals, for example, two visits
to a physiotherapist, and three visits to a psychologist. The Medicare rebate
for any of these services is $44.85.
6.96
The Central Australian Aboriginal Congress, which
provides health services to Indigenous Australians in Alice Springs,
was positive about this initiative:
The advent of ... multidisciplinary care plans have also enabled
better coordination of team care arrangements for [patients with complex and
comorbid conditions], especially the coordination of GP involvement with the
necessary allied health professionals such as psychologists and other
counsellors who provide holistic care to these patients.[570]
6.97
The NSW Nurses' Association also welcomed the
initiative:
The introduction of the new allied health items under Medicare
is a great initiative which the Association supports and we look forward to
working with the Government to ensure that people with mental illness benefit
from greater access to skilled nursing interventions. We recommend that the
Government examine more closely the role of the mental health nurse
practitioner with a view to making the benefits and advantages of wider implementation
more widely available to the public.[571]
6.98
However, the Medicare items for CDM are limited to patients
with complex and chronic conditions. Further, although visits to allied health
professionals are subsided through Medicare, the level of rebate is just $44.85,
leaving a patient with high out-of-pocket costs after visiting, say, a
psychologist, whose session can cost $100 - $175 per hour.[572] Mr
Keith Wilson,
Chair of the Mental Health Council of
Australia, expressed this concern:
The recently introduced mechanisms under the chronic disease
management items ... cost a person up to an additional $50 or $60 out of pocket
to see a psychologist. You might get a $45 rebate, but it will cost you over
$100. ... I think that, worryingly, [this initiative] has still left a very
large burden of out-of-pocket expenses on those who wish to access [psychology]
services.[573]
6.99
For a person receiving care under a CDM care plan, the
$44.85 Medicare rebate applies regardless of the type or cost of service
provided. A session with a physiotherapist or podiatrist, for example, attracts
the same $44.85 rebate, despite the fact that these sessions may take less time
and cost less than that with a psychologist. The Department of Health and
Ageing indicated that:
[There has been] debate ... about the structure of the rebates
in relation to how services are provided for; for example, something like psychology
versus physiotherapy and the amount of time that is taken and the rebates which
are available. Where that structure might go in the future is a matter that is
being considered.[574]
6.100
Mr Wilson
indicated a preference for psychologists to be, in the main, contracted
directly and for out-of-pocket cost for consumers to be nil or very small:
[The Chronic Disease Management Medicare items arrangement] is
quite different to the system that the Council and most other professional
groups have championed under Better Outcomes, which essentially involved no
additional out-of-pocket expenses or a small co-payment.[575]
6.101
It is important to note that, unlike arrangements under
Better Outcomes, GPs do not require any particular training to make referrals
to psychologists under CDM arrangements.
6.102
Departmental officials advised that CDM items have been
funded by transfer of a projected underspend against, primarily, the Service
Incentive Payment (SIP):
There was, going back over the history of the mental health Service
Incentive Payments as part of the Better Outcomes program, an underspend
against what we had anticipated the level of expenditure to be, without the
capacity for particular precision in that process. Some of that projected
underspend going forward ... has been transferred to the [Medical Benefits
Scheme] to create the new chronic disease management items.[576]
6.103
Concern was expressed that this transfer shifted funds
from mental health to the more general area of chronic disease. In response, departmental
officials argued that chronic disease management comprised a strong element of
mental health, including in all the major chronic disease categories of cancer,
heart disease and strokes. Chief Medical Officer Professor John
Horvath told the committee that 'mental
health is ... an important component of the entire chronic disease spectrum'.[577]
More Allied
Health Services
6.104
The More Allied Health Services (MAHS) program aims to 'improve
the health of people living in rural areas through allied health care and local
linkages between allied health care and general practice'.[578] As with Better Outcomes, the federal
government funds Divisions of General Practice, which then administer and fund
allied health services. Unlike Better Outcomes, MAHS can fund a range of allied
health professionals, such as dieticians and audiologists, and not just mental
health professionals.
6.105
The MAHS program funds 66 Divisions - those with at
least five percent of their population living in rural areas - to provide
clinical care by allied health providers.[579]
Divisions can use direct employment by the Division, or engage allied health
service professionals under contract. The guidelines indicate that services
should be provided free of charge.[580]
6.106
The ADGP commented:
While MAHS was not a mental health initiative, a great
proportion of the eligible rural Divisions elected to devote it to the establishment
of allied psychological services in their community.[581]
6.107
In 2003-2004, the MAHS program engaged 45.7
psychologists, 23.2 mental health nurses, 8.6 counsellors and 12.5 aboriginal
mental health workers (full-time equivalents).[582] The Top End Division of General Practice
in the Northern Territory has
used MAHS funding to employ Aboriginal mental health workers.[583]
6.108
The Government guidelines for MAHS however discourage its
use where Better Outcomes is available:
If Divisions receive funding from multiple sources, they should
use this funding effectively. For example, a Division could seek to consolidate
their mental health services using Better Outcomes in Mental Health, leaving MAHS
for other allied health professionals.[584]
6.109
However, not all GPs are registered with Better
Outcomes and therefore cannot refer to psychologists. The Limestone Coast Division
in South Australia (covering an area around Mount Gambier) found MAHS to be an
important component of the mental health services available to GPs in that area[585] and MAHS, like CDM, allows GPs to
refer patients to psychologists or other mental allied health professionals,
without needing to have undertaken particular
training, as is the case with Better Outcomes.
What is the best model for increasing access to cost-supported
psychologists?
6.110
There was broad agreement that psychologists and other
allied mental health professionals play an important role in primary mental
health care, but that they are currently an under-utilised resource. Psychiatrist
Professor Ian Hickie
said:
...there is agreement across the whole medical and psychological
health work force. All we need is an integrated work force. We need people to
be working in partnership with each other, particularly at the primary care
level and at the specialist level. We are different in Australia,
in that we do not recognise psychologists as mental health specialists in the
way they are recognised in other systems, and we do not use them effectively.[586]
6.111
In the United Kingdom,
the National Health Service (NHS) funds psychological therapy services, and
patients can receive treatment on GP referral at no cost. Services are provided
at GP's surgeries, hospitals, or local community mental health teams.[587] The committee also notes reports
that the UK
system has waiting lists of nine months to access counsellors. Nevertheless,
there is significant recognition of the importance of psychological counselling
services.
6.112
Mental health teams in Australia often include
psychologists, but these staff are often have high work loads acting as case
managers for people with serious mental illness, and do not have the time to
provide psychological treatment, early intervention or relapse prevention
strategies. Dr Georgina Phillips commented that in her experience on a
community mental health team there were not enough counselling or therapy
services available, and that it was difficult to find affordable alternatives:
My experience was that we were constantly swamped with referrals
for young people who had long-term issues that needed long-term therapies and
we really struggled to appropriately refer them to something that was not going
to be quite financially difficult for that person.[588]
6.113
Affordable access remains limited and many submissions
supported expansion of the current Government initiatives. The following section
discusses the issues involved.
Should GPs need
particular training in order to refer patients to allied health professionals?
6.114
As previously discussed, GPs must have completed Level
One training and stay registered with Better Outcomes in order to refer
patients for low-cost psychological treatment through the Better Outcomes
program. This requirement seems inconsistent with the other Government
initiatives discussed above, which allow GPs to refer patients to cost-supported
mental health allied professionals without any additional training or
registration requirement.
6.115
More broadly, there also seems to be an inconsistency
in the fact that, in the case of referrals to medical specialists such as
cardiologists or psychiatrists, GPs do not require special additional
post-graduate training. Presumably this is based on recognition that GPs
receive enough basic training (in cardiology or psychiatry, say) in their
undergraduate degree or GP registrar training to equip them to recognise a need
for additional specialist care. It could be argued that the training received
at the undergraduate level in psychiatry and psychology should similarly allow
a GP to refer a patient to a psychologist, without a requirement for further
training. It would appear that arrangements under the CDM care plans and also
under the MAHS program already accept this proposition; yet a GP referring
under Better Outcomes needs additional training to make the same referral.
6.116
It was suggested to the committee that the Level One
training requirement (which allows a GP to refer to a cost-supported
psychologist) reflected the incentive nature of the Better Outcomes program,
which aimed to reward GPs for undertaking training and up-skilling.[589] However, a result of this limitation
on GPs is that patients are affected by their GP's willingness and ability to
undertake the Better Outcomes training. The training requirement precludes the
four out of five GPs who have not undertaken Better Outcomes training from
referring patients. The patients of these GPs are clearly disadvantaged by this
requirement.
6.117
Professor Harvey
Whiteford, Clinical Mental
Health Advisor to the Department of Health and Ageing,
acknowledged this as an issue:
You could take the position ... that the GPs who have less
interest in mental health—do not bother to do the training—should be the ones
who get better access to the psychologists who have the skills. I think the
view that has prevailed is that we want to encourage all GPs to upskill and the
quality of the referral to the psychologist is greater than the knowledge base
of the GP. ... I have sympathy with [the] view that the patients of GPs who are
not interested in mental health should in some way get support if they have
mental health problems. As Mr Davies
[Acting Departmental Secretary] said, there are some GPs who will not ever be
interested in mental health. It is not their area and they do not like it
particularly, but they may well have patients with those issues. I do not think
this strategy necessarily helps them as much as those GPs who are more
interested in mental health, so we needed to broaden the strategy as we work it
through.[590]
6.118
The question thus arises of whether it is sound and
reasonable to allow referral to cost-supported psychologists by all GPs. Professor Ian Hickie thought
that the medical profession would be willing to allow referral to
cost-supported psychologists by all
GPs, not just those who had undertaken particular training. The problem, Professor
Hickie suggested, was there not being
sufficient government funding to cover that increased degree of psychological
service and support.[591]
6.119
Professor Hickie
further suggested that allowing GP referrals to appropriately qualified and
recognised practising psychologists would quickly boost the mental health
workforce:
Fundamentally, this is an issue for the psychological profession
itself. But if those who agreed to reach a certain standard of training behaved
as mental health specialists, just the way that psychiatrists do, and then saw
people essentially on GP referral then I think you would have absolute
agreement between psychology and psychiatry.
...
If the Commonwealth were to immediately recognise the number of
psychologists who would automatically meet that [standard of training]—there is
some debate about that number but there would be somewhere around 2,000
psychologists—and they were to behave like the 2,000 psychiatrists we are working
in practice, we would immediately double the mental health specialist work
force, and it would not kill the Treasury.[592]
6.120
On the question of requiring a recognised system of
qualifications and registration for practising psychologists, the committee
notes that there is already government recognition of psychologists providing
services through the CDM care planning Medicare items. These psychologists must
be registered with Medicare Australia
for their services to be rebateable.
If a system of
referrals to cost-supported psychologists by ALL GPs is supported, should this
be done through a Better Outcomes-type arrangement, or through Medicare?
6.121
As mentioned earlier, GPs currently have the ability to
refer some patients for
Medicare-rebateable treatment by a psychologist (under CDM Medicare items). This
arrangement leaves patients with significant out-of-pocket costs, however, as
the rebate of $44.85 falls short of the cost of a session with a psychologist,
which usually exceeds $100. It is this concern about out-of-pocket costs which
causes the MHCA to favour a system such as Better Outcomes, where consumers
receive psychological treatment at no cost, or for a small co-payment.[593]
6.122
The APS supports an expansion of the arrangements under
Better Outcomes for Access to Allied Health Services, to allow more GP referral
for psychological services. At the same time, the Society also supports a
Medicare-based arrangement, allowing psychologists access to the same Medicare
item numbers for Focussed Psychological Strategies available to GPs who provide
this service after having completed Level Two Better Outcomes training.[594]
6.123
The issue of expanding access to allied health
professionals through Medicare has been raised in other forums. In 2003 the
Senate Select Committee on Medicare considered suggestions of extending
Medicare to cover allied health services, and acknowledged in its majority
report that such action would have considerable and complex economic and
financial consequences. A concern of that committee was that an extension of
Medicare would raise the issue of which services would receive priority for
Medicare funding and which would not qualify. It was also pointed out that
decisions about extending coverage could arbitrarily create a financial
windfall for certain professions while excluding others.[595]
6.124
The Select Committee on Medicare concluded that rather
than extending Medicare coverage, it would be preferable instead to utilise more
targeted and effective mechanisms to increase access to allied health
professionals. The committee suggested building on existing initiatives such as
the MAHS program, and providing funding for shared access to resources via
groups such as the Divisions of General Practice.[596]
6.125
The issue of extending Medicare coverage to allied
health professionals was also considered by the Productivity Commission in its
position paper on 'Australia's
Health Workforce', released in September 2005. The Productivity Commission expressed
the view that existing mechanisms for assessing requests for changes to
Medicare coverage lack transparency. It proposed the establishment of a single,
broadly-based and independent body to make recommendations to government about extending
Medicare coverage to new services.[597]
Should GPs remain
the gateway for access to cost-supported psychological treatment, or should
consumers have access without a GP referral?
6.126
A possibility raised with the committee was not only
for the government to fund or subsidise psychological services (through
Medicare or by some other method), but to allow consumers direct access to
psychologists, without the need for a referral from a GP. It was argued that
GPs are not necessarily appropriate to perform the role of 'gatekeeper':
[The requirement for GP referral] ... means that GPs become
solely responsible for the identification of psychological health problems,
acting as gate keepers for psychological referrals, something which, for a
range of reasons, GPs have a poor track record with.[598]
6.127
Professor Ian
Hickie indicated that such a proposal had
been contentious:
...some areas of psychology have argued that it should be the
same as general practice, that somebody should be able to walk in off the
street and see someone in a primary care role and receive their psychological
care independently of any other aspect of the medical system. It is that model
which has created much more contentious discussion, because it would be a more
divided model, where psychological care and medical care would not necessarily
come together. You would essentially have another primary care work force
separated from the other work forces. So the issues of working together and immediately
recognising those who obviously have the expertise—and the numbers vary, but there
are 2,000 to 3,000 psychologists in Australia—would be a very effective,
immediate solution to the specialist side of the problem.[599]
Concluding remarks
6.128
The committee considers that most people with mental
illness do not currently have access to an integrated, specialised mental
health service that meets their needs and that fixing the problems identified
in this chapter is essential.
6.129
At the heart of the problems in primary care are three
related issues:
-
limited effective access to mental health
workers;
-
limited numbers of mental health professionals;
and
-
inadequate training of mental health
professionals.
6.130
There are many ways in which each of these three things
could be tackled. More direct involvement of psychologists in publicly-funded
health care is one. More university places and more funded positions is a
second. Stand-alone specialist degrees for mental health nurses is a third.
Many of these solutions will take time and resources.
6.131
It is also clear that the current reliance on GPs for
the bulk of those using primary mental health care and for prevention and early
intervention is ineffective. Initiatives
aimed at supporting GPs in this role have made some progress but relatively
minor adjustments, such as removing the need for GPs to have undertaken
Better Outcomes training as a pre-requisite for referring to allied health
professionals or direct access to Medicare rebates for psychologists, fall well
short of providing comprehensive, expert and timely care.
6.132
For greatest effectiveness, psychiatrists,
psychologists, psychiatric nurses, social workers and GPs should work together
in integrated teams. This does not seem
possible under the current arrangements.
6.133
The committee is of the view that publicly funded
community-based mental health centres should be established as the primary
mental health equivalents of the tertiary area mental health services that
currently operate in many states for the most seriously ill. These centres should be multi-disciplinary
and treat the broadest range of disorders.
GPs and psychiatrists in private practice who are interested and have
expertise in mental health would continue to practise in this area but would
have the support of the centre in doing so.
Whilst funding the infrastructure and the training would require
considerable investment, the committee considers that over time that investment
would be rewarded with far less demand on acute care and our prison system and
greater participation of people with mental illness in society.
6.134
A comprehensive shift toward multi-disciplinary
community based mental health centres would help complete a shift away from
acute hospital care, away from the old institutions (many of which continue to
operate, particularly in South Australia and New South Wales), and toward the
agreed goal of the National Mental Health
Strategy: an emphasis on community based care. The need for this shift to be given
a new impetus is starkly underlined by the findings in later chapters on inpatient,
crisis and community care.
6.135
The committee believes that this shift can ably be
supported by Divisions of General Practice, with their increased focus on
multidisciplinary teams and the broader emphasis on primary care generally
rather than just traditional general practice, as recommended by the Review of
the Role of Divisions of General Practice, and endorsed in the Commonwealth's
response to that review.[600]
Navigation: Previous Page | Contents | Next Page